43
Metacarpophalangeal Joint Injuries: Fractures (Intraarticular) at the Base of the Proximal Phalanx, An Arthroscopic Technique
Joseph F. Slade III and John D. Mahoney
History and Clinical Presentation
A 20-year-old varsity football player sustained an avulsion fracture of the index finger when he struck his hand against another player’s helmet. The patient presented to the trainer at the end of the game, complaining of pain and swelling at the base of the index metacarpophalangeal (MP) joint.
Physical Examination
Point tenderness was noted at the base of the proximal phalanx, with moderate swelling. The patient had reduced range of motion of the MP joint, and a stress exam elicited significant pain.
Diagnostic Studies
Standard radiographs identified a displaced intraarticular fracture of the base of the proximal phalanx involving 50% of the articular surface. Had there been any question regarding laxity of the collateral ligaments, stress radiographs would have been appropriate. The special indications for further studies are detailed in Table 43–1.
PEARLS
- Implants deep in bone permit early restoration of motion without risk of secondary inflammation or tendon rupture due to rubbing of soft tissue or tendon on prominent hardware.
- The same techniques of percutaneous fixation of intraarticular fractures can be applied to extraarticular fractures as well.
PITFALLS
- Knowledge of neurovascular anatomy is essential to avoid injury when placing arthroscopy portals and when driving K wires.
- Care must be taken to limit traction time to less than 2 hours.
| Modality | Application | Comments |
| Plain radiographs (posteroanterior, lateral, and oblique) | Capable of diagnosing most fractures and dislocations of the hand | |
| Stress radiographs | Used for defining ligamentous laxity (e.g., gamekeepers’ thumb) | When fracture is not evident on standard views |
| Bone scans | Can detect increased activity in the joint, suggestive of an osteochondral defect | Nonspecific study |
| Computed tomography scan, aligned in sagittal plane | Used for defining the step-off of intraarticular fractures | |
| Magnetic resonance imaging | Used for ulnar collateral ligament injuries in the thumb | Most sensitive in detecting the Stener lesion |
Differential Diagnosis
Fracture
Intraarticular/extraarticular fracture of metacarpal head or proximal phalanx
Axial loading injuries (either fracture or ligament injuries)
Avulsion injuries (either fracture or ligament injuries)
Simple and complex dislocations
Sprain
Diagnosis
Avulsion Fracture at the Base of the Index Finger Proximal Phalanx
Displaced intraarticular fractures require anatomic reduction to prevent chronic instability and posttraumatic arthritis. The final functional results of healed hand fractures are determined by a variety of factors, both in and out of our control. Factors that we cannot control include the severity of the fracture and age of the patient. Factors that we can control include the surgical manipulation of the soft tissue envelope and the preservation of blood supply during operative exposure.
Hand function and motion require both a healed fracture and restoration of full tendon excursion. Surgical violation of tissues surrounding the joint contributes to scarring, which limits tendon excursion.
Because of the risk of additional soft tissue trauma and the potential for delayed healing related to open reduction of fractures, recent attention has been directed to the concept and benefits of biologic or indirect reduction techniques. These techniques preserve vascular blood supply to bony fragments by minimizing dissection of the soft tissue envelope surrounding joints and bones. These indirect reduction techniques have been reported to effectively treat comminuted metaphyseal fractures of the lower extremity.
Wrist arthroscopy has been described as an effective tool in the assisted reduction of displaced intraarticular fractures of the distal radius as well as the diagnosis of additional soft tissue injuries.
Surgical Management
The arm was prepped with antiseptic soap, draped with a sterile field, exsanguinated, and the tourniquet elevated to 250 mm Hg for less than 2 hours. Disposable, sterile plastic finger traps with a traction tower provided distraction of the MP joint.
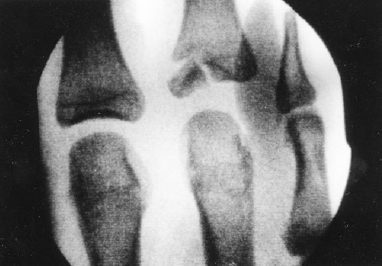
We used the minifluoroscopy unit to locate the exact location of the joint to minimize the chance of cartilage injury while establishing joint portals (Fig. 43–1). Using minifluoroscopic assistance, we marked the proposed dorsal-ulnar and dorsal-radial portals on the skin and used a free 19-gauge needle to locate the entry portals. We longitudinally incised the skin at the sites identified by the free 19-gauge needles. We were careful to incise only the skin and not the underlying tissue, as dorsal sensory nerves can cross through the area of the portals. We then performed blunt dissection with a small hemostat to the level of the joint capsule and used the hemostat to carefully spread the joint capsule and enter the joint.