Fig. 5.1
Prepared allograft. A single stitch placed at the junction of the posterior horn and the body and a continuous loop suture is fastened to both horns utilizing a baseball stitch

Fig. 5.2
Residual meniscus prepared to accept allograft. Remnant is trimmed to a width of 1 mm
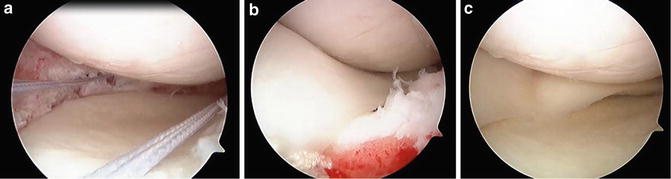
Fig. 5.3
(a–c) Delivering the allograft. The graft is pulled into the joint by sequentially pulling on the nitinol wire attached to the posterior horn and then the wires attached to the passing suture
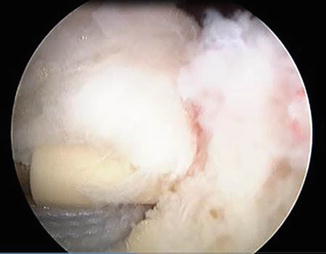
Fig. 5.4
Anterior horn fixation. A continuous loop suture initially placed in the anterior horn is secured to the tibial plateau with a knotless suture anchor
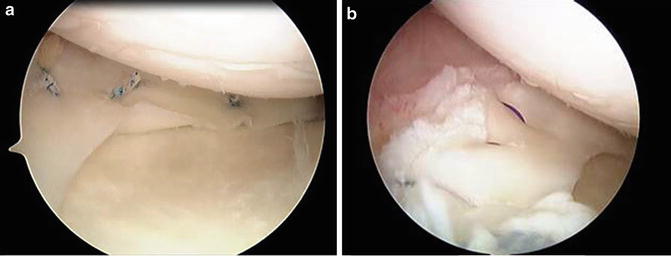
Fig. 5.5
(a, b) Peripheral allograft fixation. Two all-inside meniscal fixation devices placed within the posterior horn, then an additional all-inside meniscal fixation device is placed just anterior to the passing sutures, and lastly three synthetic absorbable monofilament sutures are placed in an outside-in fashion into the anterior horn
Technical Pearls
1.
Exposure is paramount. For medial-sided transplants, MCL release via trephination of the MCL origin, perforation with an awl or thermal release may be necessary. For lateral-sided surgery, a partial “recession” of the popliteus tendon with a thermal device can increase working space greatly.
2.
Know your tissue bank. Investigate the “track record” of vendors and compare service and tissue quality.
3.
“Back biting” instruments are very useful in removing anterior horn tissue.
4.
Ensure that your “suturing” portal for “outside in” or fixators is low enough to permit suture access to the capsular margin. Vertical mattress sutures provide appreciably higher pullout strength than horizontal mattress configuration.
Alternate Techniques
Repeatedly mentioned in the literature is a technique utilizing a dovetail bone block, described as such due to its trapezoidal shape when viewed in the coronal plane. This block, or bridge between the anterior and posterior horns, is placed in a congruent slot prepared in the recipient tibia. Also described is a technique utilizing cylindrical bone plugs fashioned at the donor meniscal horn attachments. These plugs are transfixed with suture into tibial tunnels drilled over a guide wire. The senior author has recognized that bone block containing grafts introduce an additional level of difficulty in graft passage. The technique herein described affords direct bone fixation and obviates the need for passage of bulky bone fragments through the joint and subjacent bone tunnels.
For lateral meniscal transplantation, the process is essentially identical, with some differences to consider. The anterior and posterior horn attachments of the lateral meniscus are much more closely approximated than the medial side. Thus, to gain access to the posterior horn of the lateral meniscus, a retractor probe may be necessary to shift the ACL medially in order to visualize the posterior horn drill site. Secondly, since the anterior and posterior horns are in close proximity, one must be mindful not to converge bone tunnels. The authors find that the best angle of approach to the anterior horn is via a high contralateral medial portal.
Although many advocate a “bone bridge” technique for the lateral meniscus transplantation, the authors have not found this necessary and maintain that direct bone fixation is attained in more facile fashion with the above-described technique.
Additional Considerations
As previously discussed, concomitant pathology from injury such as ACL deficiency or chondral defect should be addressed at the time of or prior to meniscal allograft transplantation. Varus and valgus deformity should also be taken into consideration in the setting of meniscal transplantation. In patients with axial malalignment, high tibial osteotomy or distal femoral osteotomy should be performed in conjunction with MAT.
Postoperative Management
For as many operative techniques described, there are twice as many proposed postoperative protocols proposed. At our institution, we prescribe the following restrictions: non-weight bearing for a duration of 6 weeks, to be followed by partial weight bearing with a gradual increase to full weight bearing over the next 2–4 weeks. Discontinuation of crutches is upon resolution of limp. Range of motion is limited to 0–70° for the first 4 weeks, followed by 0–90° for weeks 5 and 6, then increase as tolerated. Aside from aforementioned restrictions, physical therapists are instructed to rehab these patients in the same manner as they do meniscal repair patients. Return to sport is anticipated at 6 month.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








