Fig. 8.1
This coronal image shows an extruded medial meniscus
On the sagittal MRI images, root injury will manifest with anterior displacement of the meniscus. As the meniscus breaks free of its posterior horn attachment, its tendency is to slide anteriorly, rather than posteriorly. The amount of anterior displacement thus correlates with the degree of posterior horn detachment.
Axial images may reveal separation of the posterior horn and tibia. These “spaces” which enhance on T2 images are often subtle but may significantly reinforce evidence of a root injury.
Treatment
If degenerative changes are not pronounced, then repair of meniscal root injury should be considered. The Kellgren-Lawrence scale is helpful in formulating treatment plans. Harner et al. described some contraindications for meniscal root repair: significant medial joint space narrowing and/or Fairbanks changes, diffuse grade 3 or 4 cartilage changes in the articular cartilage of the femoral condyle or tibial plateau, and greater than 3° of asymmetric varus alignment [15]. In general, if there is less than 50 % joint space narrowing, the author favors an attempt at repair.
After the patient and surgeon have decided to pursue surgical treatment, the surgeon examines the tear arthroscopically during a diagnostic knee scope. The surgeon must examine the tear characteristics and the tissue quality (Fig. 8.2). In addition, the surgeon should evaluate the articular cartilage of the knee joint. At times, during arthroscopic inspection, the tissues are too poor to support repair, and the arthritis index is greater than anticipated. Otherwise, a properly executed repair presents minimal harm to the patient. After the tear and the surrounding knee structures have been thoroughly evaluated and the decision is made to pursue fixation, then the tear should be debrided to remove any meniscal flaps or fraying that may worsen visualization and/or impede fixation (Fig. 8.3).
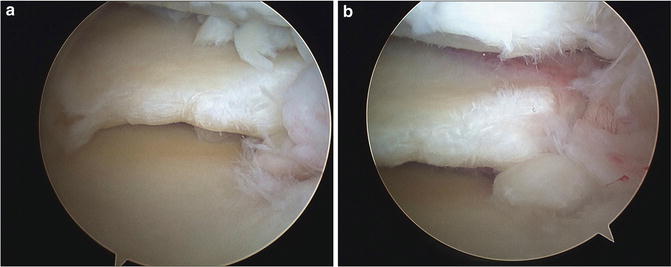
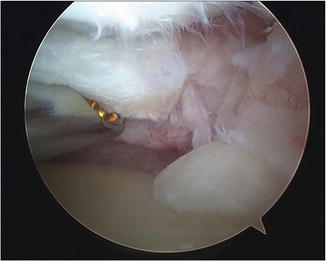
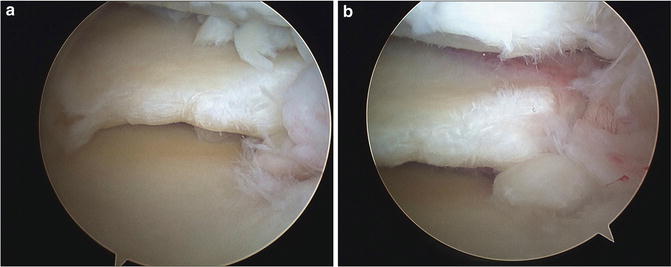
Fig. 8.2
(a, b) These arthroscopic images demonstrate a root tear of the posterior horn of the medial meniscus
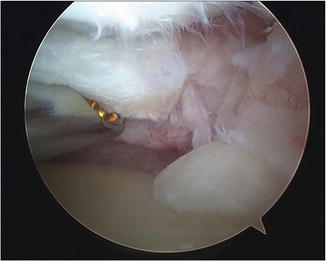
Fig. 8.3
An arthroscopic shaver is used to debride the frayed edges of the tear
Once the tear has been debrided, then an assessment must be made as to which type of repair should be performed. A probe can be used to examine the tear and evaluate tissue quality and extent of the tear (Fig. 8.4). Since the essence of the injury is an avulsion, most repairs require fixation to bone. Rarely, there is enough residual posterior horn tissue to allow a repair using all-inside meniscal fixators (Fig. 8.5a–e) or using a luggage tag technique (Fig. 8.6a–c). In most cases, the tissue will not support suture fixation, and attachment of the avulsed segment to bone is required.
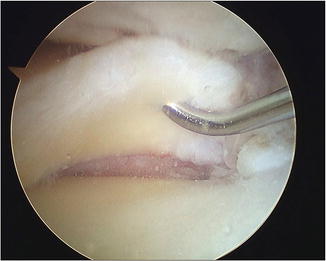
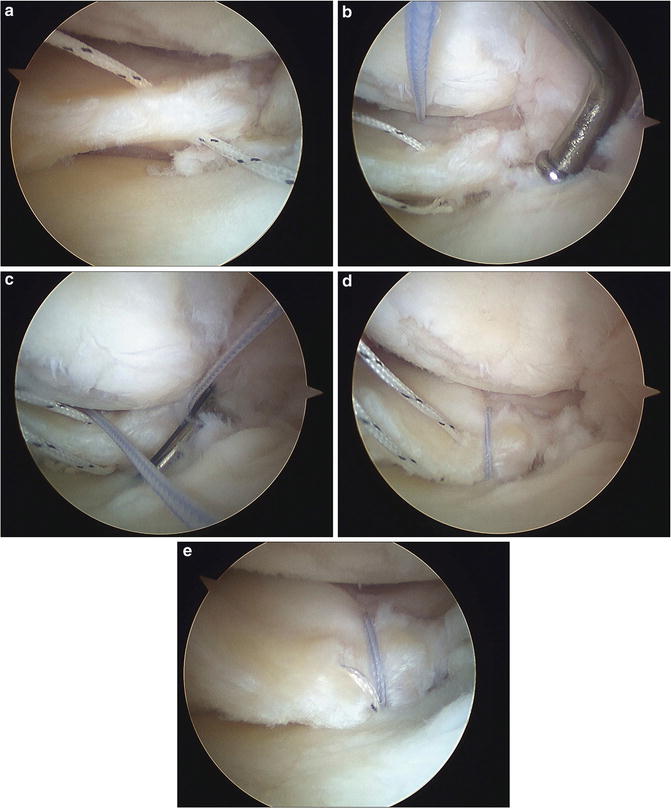
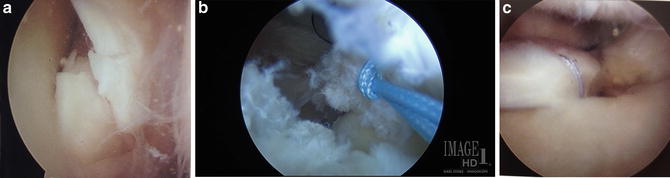
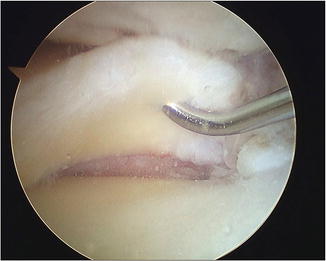
Fig. 8.4
A suture hook is used to pass a shuttle into the posterior horn fragment
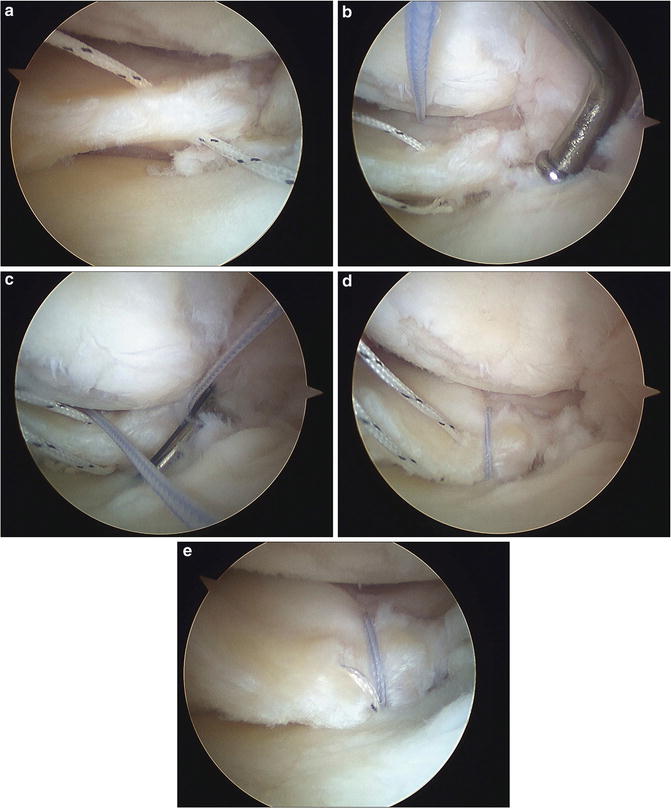
Fig. 8.5
The tissue quality of this meniscus was deemed to be suitable for an all-inside repair. (a) The first suture is passed through the tear. (b) The second suture is then passed through the tear. (c, d) The first suture is tied. (e) A final image demonstrating the repaired tear
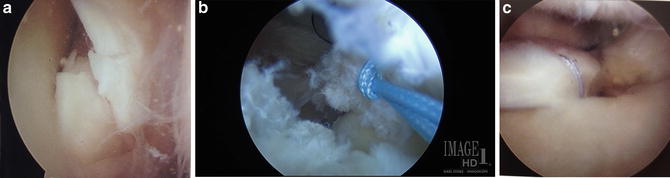
Fig. 8.6
(a) This image demonstrates a meniscal root avulsion tear. (b) A luggage tag stitch has been thrown through the fragments of avulsed meniscus. (c) The avulsed meniscus is now repaired
Bone Tunnel Technique
A leg holder is extremely helpful in applying the necessary valgus stress to the knee to open up the medial compartment. For medial injury, a high lateral viewing portal is created and the diagnosis confirmed with probing of the meniscus. A low medial parapatellar portal is established first for probing and later for viewing. Medial portal creation closer to the joint line affords easier access to the posterior horn. A second medial portal is made more medially, just above the joint line, and is necessary for suture shuttling.
In order to execute the surgery readily, release of the medial collateral ligament (MCL) is necessary. This can be performed numerous ways. A simple spinal needle can be used to trephinate the origin of the MCL. Alternatively, a microfracture awl or spinal needle can be employed from the lateral portal to create small perforations in the meniscocapsular junction. Finally, in especially tight knees, the author favors thermal ablation of the superficial and deep MCL.
To execute repair, the arthroscope is switched to the medial portal, and the contralateral high lateral portal is used to gain suture purchase of the meniscus. The author favors a spectrum 45-degree type suture hook to pierce the meniscus with a PDS suture. The No. 1 PDS is used to shuttle a No. 2 FiberWire (Arthrex, Naples, FL) (Fig. 8.7). The accessory medial portal is used for retrieving during shuttling. After the first suture is passed and shuttled, a second “bite” is then obtained, as perpendicular as possible to the first, with the shuttle steps repeated. It is important to take more than one bite as tissue quality may be suboptimal. Rarely, use of the posteromedial portal, or even a posterior puncture with a spinal needle, may be necessary to pierce the meniscus in an orthogonal fashion. Once both suture limbs are shuttled through the avulsed segment, they are retrieved through the accessory medial portal (Fig. 8.8).

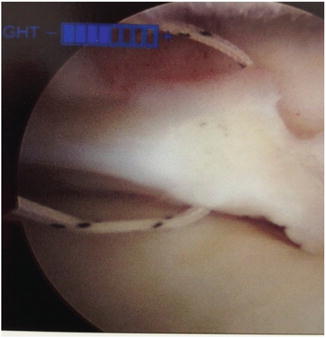

Fig. 8.7
No. 1 PDS is used to shuttle FiberWire through the avulsed meniscus
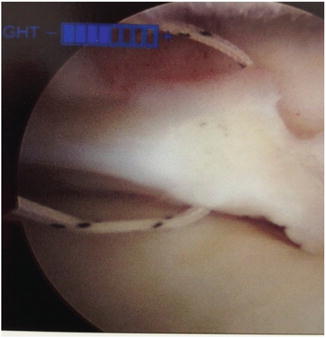
Fig. 8.8
A FiberWire has now been passed through the avulsed meniscus
The bone tunnel for suture anchorage must now be created. An ACL guide with a low profile tip is placed via the medial parapatellar portal, while viewing is performed from the lateral portal. Before the tip is placed on the posterior horn insertion, the drill guide location is marked with an electrothermal device. Recall that the posterior horn of the medial meniscus is much more posterior than that of the lateral meniscus.
The bullet tip of the drill is applied to the skin overlying the tibia, then the tip is removed, and a small incision is created on the medial tibia down to periosteum. Enough exposure to ensure suture retrieval is attained. The bone tunnel is created with a standard 3/32-in Steinmann pin and the drill “bullet” is firmly applied to the bone surface. Marking the tip of the Steinmann pin with marker ink helps locate the drill tunnel when the pin is removed. A Hewson suture passer is immediately threaded into the tunnel through the bullet to retrieve the first pair of sutures.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








