Meniscal Débridement
Michael Shin
Geoffrey S. Baer
INTRODUCTION
Much has been learned about the anatomy and function of the meniscus since 1897 when Bland-Sutton described the meniscus as “functionless remnants of intra-articular leg muscles” (6). Since that time, there has been a significantly better understanding of the meniscus’s multiple important roles in load bearing, joint stability, shock absorption, proprioception, and lubrication (22).
Meniscal tears can occur from both acute injuries and from chronic degeneration. The exact incidence of meniscal tears is difficult to ascertain due to the high number of asymptomatic tears and the high rate of degenerative tears in patients with advanced degenerative joint disease. It is estimated that the incidence of acute meniscal tears in the United States is approximately 61/100,000 persons per year. An epidemiologic study from Europe estimated the incidence of meniscal tears to be about 60 to 70/100,000 persons (24,44). Meniscal tears are found more commonly in males, a ratio of 2.5:1 to 4:1, and up to one third of tears are associated with anterior cruciate ligament (ACL) injuries (16,49).
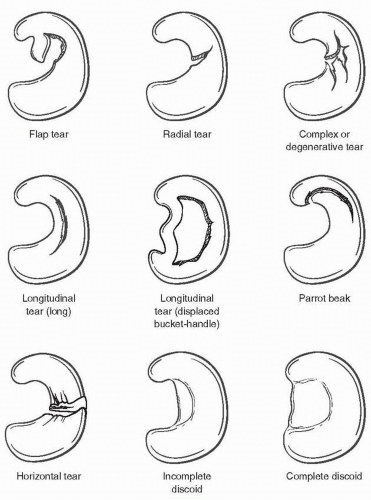
The classification of meniscal tears can be based on tear location, blood supply, or by tear pattern (Fig. 20.1). The classification of the tear, in addition to other patient and tear characteristics, assists in the process of deciding the appropriate treatment. Meniscal tears can also be found in meniscal variants, the most common of which is a lateral discoid meniscus. Arthroscopic studies have shown a prevalence of discoid menisci ranging from 0.4% to 16.6% and most are typically discovered incidentally, as they are usually asymptomatic. Discoid menisci are more common in patients of Japanese or Korean descent and can be bilateral in up to 20% of patients (5,30).
With an increased understanding in the importance of the meniscus and in preserving as much functional meniscal tissue as possible, meniscal repair has become an increasingly important option for the treatment of meniscal tears. The possibility of meniscal repair should be considered when evaluating meniscal injuries, especially in young, active patients with or without concomitant ACL reconstructions. However, some meniscal tears are not amendable to meniscal repair due to meniscal degeneration, tear location and pattern, limited vascular supply, or patient age. In these settings, meniscal repair can be impossible or unlikely to heal, and meniscal débridement is the treatment of choice for these patients with symptomatic meniscal tears. Arthroscopic meniscal débridement has become one of the most common orthopedic procedures performed in the United States today, and the AAOS estimates that over 636,000 arthroscopic knee procedures are performed each year (50).
INDICATIONS/CONTRAINDICATIONS
Arthroscopic intervention for meniscal tears are typically for patients who have failed nonoperative management that includes activity modification, physical therapy, and pain medication. Patients will typically have joint line pain and mechanical symptoms such as locking, catching, and giving way that affect activities of daily living, participation in sports, and work.
Meniscal tears in young patients and tears associated with ACL reconstructions should have a meniscal repair if possible. However, many tears found during surgery are not amendable to repair, in which case, a partial meniscectomy that removes unstable fragments and creates a smooth transition, while maintaining as much functional meniscus, should be undertaken (41).
Meniscal tears, especially degenerative tears, increase with increasing age and surgical intervention is contraindicated for asymptomatic patients with tears on imaging studies. A study evaluating one hundred patients with an average age of 43 years with a magnetic resonance imaging (MRI) of asymptomatic knees showed a 37% prevalence of meniscal tears (64). Also, patients with degenerative meniscal tears in the setting of significant degenerative joint disease may obtain minimal benefit from arthroscopic meniscal débridement, and arthroscopic intervention should be undertaken only after exhausting nonoperative management. Degenerative changes and damage to the articular cartilage found at the time of arthroscopic partial meniscectomy had the greatest impact on long-term outcome and correlated with significantly worse functional outcomes at 12 year follow-up (26,54).
Another advancement in the current management and treatment of meniscal tears is demonstrated by the further understanding of the importance of preserving as much functional meniscal tissue as possible, without leaving unstable flaps or abrupt transitions. This evolution in philosophy is demonstrated by our current management when contrasted to past treatment of meniscal tears evidenced by McMurray, who in 1942 stated, “a far too common error is shown in the incomplete removal of the injured meniscus” (38). The effects of this type of treatment for meniscal tears were described a short time later by Fairbank who in 1948 described the radiographic “changes in the knee joint after meniscectomy” including “ridge formation, narrowing of the joint space, and flattening of the femoral condyle” (19). Other studies have further delineated the importance of preserving the meniscus through demonstration of decreased contact areas and increased peak contact stresses after partial and total meniscectomies and by showing worsening radiographic progression of osteoarthrosis in patients with <50% meniscal rim remaining compared to patients with >50% meniscal rim remaining after arthroscopic partial meniscectomy (4,26). Another study demonstrated the importance of maintaining the peripheral circumferential meniscal fibers in order to preserve the ability of the meniscus to resist hoop stresses. By retaining the periphery of the meniscus, there was a decrease in mean contact pressures, while loss of this peripheral meniscus, resulting in a segmental meniscectomy, was functionally equivalent to a total meniscectomy. This cadaveric study demonstrated that this peripheral portion of the medial meniscus had a greater
contribution to increasing contact area and decreasing mean contact stresses than the central portions (36). Clinically, Northmore-Ball et al. (45) reported significantly worse outcomes in patients who had undergone open total meniscectomies compared to the arthroscopic partial meniscectomy group with 68% versus 90% good to excellent results.
contribution to increasing contact area and decreasing mean contact stresses than the central portions (36). Clinically, Northmore-Ball et al. (45) reported significantly worse outcomes in patients who had undergone open total meniscectomies compared to the arthroscopic partial meniscectomy group with 68% versus 90% good to excellent results.
PATIENT EVALUATION (HISTORY, PHYSICAL EXAMINATION, AND RADIOGRAPHIC EVALUATION)
A complete history and physical exam is essential when evaluating any patient with knee pain and possible meniscal pathology. Patients with meniscal tears typically complain of pain localizing to the joint line, swelling, locking, catching, giving way, and loss of motion. The mechanism of injury often is a twisting or hyperflexion injury that presents with acute pain and swelling. In a study of patients with normal radiographs and a meniscal tear at arthroscopy, Drosos and Pozo (16) reported that approximately 32% of the tears occurred during a sporting activity, 39% were sustained during nonsporting activities, the majority of which were during activities of daily living most commonly squatting, and 29% had no identifiable mechanism.
Physical exam usually demonstrates a patient with a joint effusion, pain in deep flexion, or pain with squatting. With a flipped bucket-handle meniscus tear, patients may have a mechanical block to motion, typically full extension. Specialized tests for meniscal tears include joint line palpation, McMurray test, and the Apley grind test; however, these tests have been reported to have poor sensitivity, specificity, and positive predictive values, especially in isolation (17,39,62). Joint line tenderness with palpation is the most sensitive of the physical examination tests and has 74% sensitivity. A positive McMurray test with a palpable “clunk” at the joint line is very specific for a meniscal tear with 98% specificity but is only 15% sensitive, and pain alone with a McMurray test makes the test more sensitive but less specific. A positive Apley grind test has a sensitivity of 60% and a specificity of 70% (25,40,59). Patients with discoid menisci may present with the classic presentation of a “snapping knee,” but this is the least common presentation. It usually presents as lateral sided joint pain of insidious onset in a child or young adolescent (30). Physical examination should also include a ligamentous examination to assess for ligamentous damage and instability and an examination for degenerative joint disease.
Diagnostic studies are used to supplement and confirm diagnosis made through history and physical exam. Standard radiographs do not confirm a diagnosis of meniscal tears but are very important in evaluating the knee for joint space narrowing, calcification of the meniscus, and degenerative changes. The 45-degree posteroanterior flexion, standing weight-bearing radiograph is more sensitive for evaluating joint space narrowing, and full-length standing radiographs may also be utilized to evaluate overall limb alignment (51). Radiographs of a patient with a discoid meniscus are frequently normal but may have subtle findings of a widened lateral joint space, cupping of the lateral tibial plateau, or flattening/squaring of the lateral femoral condyle (30).
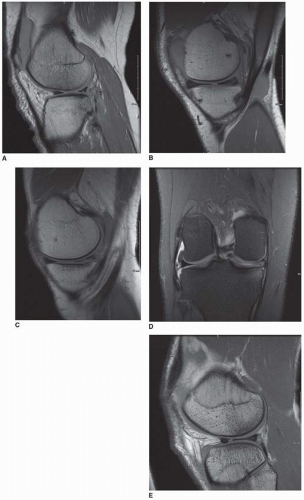
MRI may be utilized to accurately evaluate tear location, tear pattern, and associated ligamentous and chondral pathology (Fig. 20.2). The limitations of MRI include its high cost and potential for misinterpretation, especially due to normal increased signal in the meniscus found in children and with increasing age in adults. Despite this potential for error, advances in technology and experience have increased the accuracy of MRI in diagnosing meniscal tears to 95% or better (43). Another consideration when evaluating MRI includes the high rate of positive readings in asymptomatic individuals (7,35). Therefore, MRI should be used as a diagnostic tool to supplement the clinical diagnosis. Discoid menisci are often found incidentally on MRI, and there are characteristic findings on both the sagittal and the coronal planes. In the sagittal plane, three or greater contiguous 5-mm sections that show the classic “bow-tie” appearance representing continuity of the anterior and posterior horns are diagnostic for a discoid meniscus. In the coronal plane, when viewing a image from the midpoint from anterior to posterior, revealing the free edge of the lateral meniscus to extend past the midpoint of the femoral condyle or further toward the intercondylar notch is suggestive of a discoid meniscus (30).
SURGICAL TECHNIQUE (GENERAL, POSITIONING, TECHNIQUE)
Meniscal débridements have transitioned from total meniscectomies performed open to the current treatment of arthroscopic partial meniscectomies. Open total meniscectomies were originally thought to be benign procedures and were commonly performed for all types of meniscal pathology. However, as more has been learned about the long-term sequelae of open total meniscectomies and with the improvement of arthroscopic techniques, this procedure has fallen out of favor.
Arthroscopy can be performed under many forms of anesthesia including general, regional, and local based on multiple factors including length and type of procedure, patient’s medical conditions, and the preferences of the patient, surgeon, and anesthesiologist (11,12,55,63). After adequate anesthesia has been achieved, the procedure begins with an examination under anesthesia (EUA). This exam utilizes the ability to get a thorough examination with the patient relaxed and without causing patient discomfort. The examination should evaluate for the presence of an effusion, passive range of motion (ROM), a Lachman test, anterior and posterior drawer tests, a pivot shift, varus and valgus testing at full extension and at 30 degrees of flexion, a Dial test, and examinations for patellar instability. Upon completion of the EUA, the patient is then positioned for the arthroscopic portion of the case. The patient is positioned supine on the operating room table, and care is taken to adequately pad the contralateral peroneal nerve and all bony prominences. A well-padded tourniquet is placed on the upper thigh of the operative leg but is typically not required unless necessary for visualization (34). Two common methods of setup include the use of a lateral post or leg holder, which help to assist the surgeon in positioning and manipulating the leg intraoperatively.
If the lateral post technique is used, the patient is positioned supine on the operating room table and the post is placed at the level of the tourniquet at approximately the level of the mid to upper thigh. A footrest can be secured to the bed and allows the leg to rest at 70 to 90 degrees of flexion and can be used with or without a bump under the ipsilateral hip. The lateral post assists in placing a valgus force through the knee, and advantages include better access to both posterior and superior accessory portals and the ability to rest the leg on the table when the knee is in full extension. A foot rest or hanging the leg off the side of the operative table assists with holding the leg when the knee is in flexion. The lateral post also has the advantages of not acting as a venous tourniquet and not fixing the thigh in place and therefore allowing more flexibility in positioning the leg, including in the figure-four position (Fig. 20.3).
When using the leg holder technique, the patient is positioned supine on the operating room table and the patient’s thigh is placed so that the knee is past the break of the table so that the bed does not block the ability of the knee to flex. The leg holder stabilizes the thigh while the foot of the table is dropped and the operative leg hangs free (Fig. 20.4). The nonoperative leg is then placed into a padded well-leg holder. The foot of the patient’s operative leg can be placed on the surgeon’s hip and then be manipulated into varus and valgus. Exsanguinating the leg by elevating the tourniquet prior to placement of the leg holder can help prevent venous bleeding. Proponents of the leg holder remark that it allows for greater valgus stress to be placed across the knee and therefore provides better visualization and access to the posteromedial joint. However, extra attention must be taken during patient positioning to assure that the leg holder is proximal on the thigh to not block access to accessory portals and to allow the knee to maximally flex. Proper positioning can be especially difficult in heavy patients with short thighs. The leg holder should also not be overtightened to avoid it acting as a venous tourniquet, which can be a significant concern during longer procedures.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree