Medial Patellofemoral Ligament Reconstruction
Miho J. Tanaka
Andrew J. Cosgarea
Medial patellofemoral ligament (MPFL) reconstruction is indicated for patients with recurrent lateral patellar instability; the goal of this procedure is to restore the primary medial restraint of the patella. However, patellofemoral instability is a complex entity. Although the MPFL is disrupted in 94% of patients after acute patellar dislocations (15), there are a multitude of factors that can contribute to patellofemoral instability, including bony deficiencies, malalignment, ligamentous laxity, and muscle imbalance. Successful outcomes after MPFL reconstruction require the recognition of both the function and limitations of this procedure in the setting of those other factors. An understanding of patellofemoral kinematics combined with thorough preoperative assessment and planning will allow one to provide the appropriate treatment for patients with lateral patellofemoral instability.
INDICATIONS/CONTRAINDICATIONS
Patients with recurrent episodes of lateral patellar instability typically present in adolescence, often after an acute inciting event. They may describe symptoms of anterior knee pain that accompany the episodes of instability. As with most conditions, the first line of treatment for patellar instability is nonoperative interventions, including activity modification, brace protection, and physical therapy. A brace with a lateral buttress, along with oral analgesics and icing, can help minimize the initial symptoms. Physical therapy is useful in helping the patient regain strength and function. The goals of rehabilitation are to minimize the lateral forces on the patellofemoral
joint by strengthening the vastus medialis obliquus (the dynamic medial stabilizer of the patella) and by stretching the lateral extensor mechanism and retinaculum. Activity modification, which is generally not well accepted in a young, active patient, includes avoidance of activities involving planting and twisting motions.
joint by strengthening the vastus medialis obliquus (the dynamic medial stabilizer of the patella) and by stretching the lateral extensor mechanism and retinaculum. Activity modification, which is generally not well accepted in a young, active patient, includes avoidance of activities involving planting and twisting motions.
In the event that nonoperative treatment fails, choosing the appropriate operative intervention by correctly understanding the source of the patient’s symptoms is key in attaining successful outcomes. First, because MPFL reconstruction recreates the primary medial stabilizer of the patella, patellofemoral pain alone must be carefully differentiated from patellofemoral instability in the history and physical examination. MPFL reconstruction is reserved for lateral instability of the patella and should be regarded as a stabilization procedure. In contrast, symptoms of maltracking, arthrosis, and excessive lateral patellar pressure are better addressed by tuberosity osteotomy procedures that realign the extensor mechanism and unload the lateral patellofemoral cartilage.
Second, a thorough assessment of the factors contributing to the patient’s patellofemoral instability must be considered before proceeding with MPFL reconstruction. Numerous factors can contribute to patellar instability, most of which involve a combination of hyperlaxity, malalignment, and bony abnormalities. Trochlear dysplasia and insufficiency of the medial retinaculum and MPFL can reduce the medial restraint of the patella and facilitate lateral instability. Such cases without concomitant malalignment can be treated with MPFL reconstruction. In contrast, instability secondary to substantial malalignment indicated by excessive lateralization of the tibial tuberosity (tibial tuberosity trochlear groove distance >15 mm), with or without patella alta, is better treated with tuberosity osteotomy procedures. MPFL reconstruction can be used to supplement these procedures in the event that adequate patellar stability is not attained after distal bony realignment.
Third, medial patellofemoral instability, although rare, should be distinguished from lateral instability because the former is a contraindication to MPFL reconstruction. Medial instability is usually an iatrogenic problem that occurs after an overly aggressive lateral retinacular release. MPFL reconstruction restores lateral patellar instability only and does not address medial instability. Other contraindications include active infection and inability to comply with postoperative instructions. Skeletal immaturity is not an absolute contraindication to MPFL reconstruction, but it necessitates an alternative procedure that avoids drilling a tunnel through the distal femoral physis (6).
PREOPERATIVE PLANNING
History
A thorough preoperative history and physical examination is required to evaluate each individual’s causes of patellar instability. The obtained history should include the duration of symptoms and the number of episodes of instability. Patients may present after the first acute episode, describing it as a sense of giving way during a planting and twisting motion. Less commonly, direct trauma to the medial knee can also cause patellar instability. Patients may note an initial hemarthrosis and tenderness along the course of the MPFL. Those with recurrent instability after the initial trauma may have associated anterior knee pain or mechanical symptoms from chondral injuries and loose bodies. Any previous treatment or procedure for their symptoms should be noted. Instability after a previous lateral retinacular release may indicate medial patellar instability, which should be noted in the examination.
Physical Examination
Physical examination begins with the patient in a standing position as the clinician notes any abnormalities in alignment, including genu varum or valgum, increased femoral anteversion, and excessive pronation of the foot. The examination continues with the patient sitting on the edge of the examination table: observation of patellar tracking in active extension may reveal a positive J sign, made apparent by lateral translation of the patella as it exits the trochlear sulcus while the knee approaches full extension. With the patient in the supine position, the patient’s Q angle is noted by measuring the angle between two lines: one from the anterior superior iliac spine to the center of the patella and one from the tibial tubercle to the center of the patella. The Q angle is usually difficult to measure and is typically greatest at 90 degrees of knee flexion. Angles of more than 15 degrees in males and 20 degrees in females suggest malalignment. Any hypoplasia of the vastus medialis obliquus or quadriceps should be noted. As always, a thorough ligamentous examination is obtained, with care taken to rule out concomitant injury. In particular, the knee should be assessed for injuries to the medial collateral and anterior cruciate ligaments because they may have a similar mechanism of injury.
Several tests are used specifically to assess patellar instability. With the knee in extension, the glide test is used to assess patellar mobility and medial structure laxity. This test is performed by manually displacing the patella laterally (Fig. 16.1). Excursion is measured in patellar quadrants, which are described as one quarter of the width of the patella. Normal lateral translation is quantified by comparing the test to the normal contralateral patella. In patients with bilateral patellar instability, it may be difficult to assess what degree of translation is pathological or normal. The apprehension sign is assessed by displacing the patella laterally with the knee at 20 to 30 degrees of flexion. A sense of apprehension in the patient with this motion is often
indicative of patellar instability. Finally, the tilt test is used to assess for tightness of the lateral structures. This examination involves lifting the lateral border of the patella. If the clinician is unable to elevate the lateral border of the patella above the horizontal plane, this test is considered positive and may be an indication for lateral retinacular release. Any medial patellar instability and associated medial apprehension should be ruled out during the physical examination.
indicative of patellar instability. Finally, the tilt test is used to assess for tightness of the lateral structures. This examination involves lifting the lateral border of the patella. If the clinician is unable to elevate the lateral border of the patella above the horizontal plane, this test is considered positive and may be an indication for lateral retinacular release. Any medial patellar instability and associated medial apprehension should be ruled out during the physical examination.
Radiographic Imaging
Adequate imaging studies are critical in detecting anatomic abnormalities that may contribute to patellar instability. They may also help in identifying any associated injuries. Standard radiographs include anteroposterior, lateral, and sunrise views of the knee at 30 to 45 degrees of flexion. The lateral radiograph should be noted for any signs of patella alta or trochlear dysplasia. The crossing sign, seen on the lateral view of the knee, is present when the line of the anterior femoral condyles crosses that of the trochlear groove, indicating a dysplastic trochlea. Radiographs may also show the presence of loose bodies from chondral injury or calcification along the medial border of the patella, indicative of MPFL injury.
Computed Tomographic Imaging
Computed tomography can also be used to assess the bony abnormalities associated with patellar instability. Precise measurements of the degree of patellar tilt, the height of the lateral trochlear ridge, and the degree of patellar subluxation are possible with computed tomographic imaging. The degree of subluxation is assessed by the congruence angle on the axial view, which is measured by the difference in angle between the line bisecting the femoral sulcus and the line drawn from the center of the sulcus to the patellar apex. Angles lateral to the bisecting line are considered positive, and medial angles are considered negative. Tubercle malalignment can also be measured on axial views with the tibial tuberosity trochlear groove distance; measurements of more than 15 mm are considered to be abnormal and indicate malalignment.
Magnetic Resonance Imaging
Magnetic resonance imaging can provide information regarding anatomic alignment, but it is most valuable in visualizing soft tissue and cartilage injuries. Magnetic resonance imaging can show the details of MPFL injury with regard to the type and location of the tear (11). It is also used to identify the presence of chondral lesions or concomitant ligamentous injury, which is particularly helpful in planning for concurrent procedures.
Potential Intraoperative Findings
When planning for MPFL reconstruction, the clinician should anticipate that additional or alternative intervention(s) may be required based on the intraoperative evaluation. For example, contractures of the lateral patellar soft tissues may require a lateral release, and the presence of chondral lesions found during diagnostic arthroscopy may necessitate débridement and possible microfracture. On the other hand, high-grade chondral lesions that require unloading may prompt the need for a distal realignment procedure instead of MPFL reconstruction. The potential need for these procedures should be adequately addressed in the preoperative consent and planning process.
SURGICAL PROCEDURE
Preparation
The patient is placed in a supine position on the operating room table. Anesthesia is administered using general or regional techniques. Prophylactic intravenous antibiotics are given before the incision is made. A thorough examination of the operative and contralateral knees is performed. Standard evaluations include range of motion (ROM) testing and the Lachman test, posterior drawer test, and assessments of varus and valgus stability. The patellofemoral examination involves the assessment of patellar stability with the glide test and the tilt test to determine lateral retinacular tightness (Fig. 16.1).
A thromboembolic deterrent stocking is applied to the nonoperative leg. A tourniquet is then applied to the operative proximal thigh, and a vertical post is placed distal to the tourniquet. The leg is then prepped and draped with sterile, impervious drapes.
Diagnostic Arthroscopy
Diagnostic arthroscopy is performed via the standard superolateral, inferomedial, and inferolateral portals. The suprapatellar pouch and medial and lateral parapatellar gutters are closely observed for loose bodies. Evaluation of the patellofemoral joint should include the visualization of patellar tracking during ROM of the knee, with special attention directed to observing the shape of the trochlea and condition of the patellar facets and trochlear ridges. Any chondral damage is noted, with débridement and microfracture performed as needed. If a high-grade chondral lesion involving the inferior pole or lateral facet of the patella is found, the surgeon may, at this time, choose to proceed with a tuberosity osteotomy instead. The complete diagnostic evaluation includes assessment of the anterior and posterior cruciate ligaments, medial and lateral compartments, as well as the posteromedial and posterolateral compartments through the femoral notch.
Landmarks and Graft Harvest
The leg is exsanguinated with an Esmarch bandage, and the tourniquet is inflated. The bony landmarks of the patella and patellar tendon, the medial femoral epicondyle and adductor tubercle, as well as the site of the pes insertion (Fig. 16.2) are marked on the skin surface. A short oblique incision is made over the pes anserine insertion to expose the subcutaneous tissue. Blunt dissection is used to expose and identify the sartorial fascia, and any vessels that cross the field are cauterized. The sartorial fascia is incised and everted, exposing the gracilis and semitendinosus tendons (Fig. 16.3). The semitendinosus tendon is released distally and tagged for harvesting. The fascial band from the semitendinosus to the medial head of the gastrocnemius (˜7 cm proximal to the pes insertion) is released, and the graft is harvested using an open-ended pig-tail tendon stripper. The gracilis tendon may also be used in place of the semitendinosus tendon as an alternative graft for this procedure.
Graft Preparation
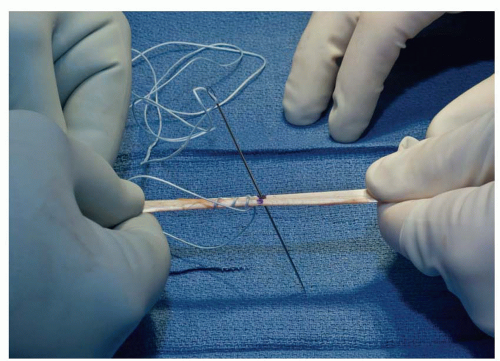
The semitendinosus tendon graft is prepared by removing the muscle and soft tissue debris from the graft. The tendon is then doubled and measured in length (Fig. 16.4). Alternatively, with a large semitendinosus graft, a single strand may also be used here. A 2 FiberLoop (Arthrex, Inc., Naples, Florida) is woven through the semitendinosus tendon graft (Fig. 16.5), with the sutures exiting the midportion of the graft (Fig. 16.6).
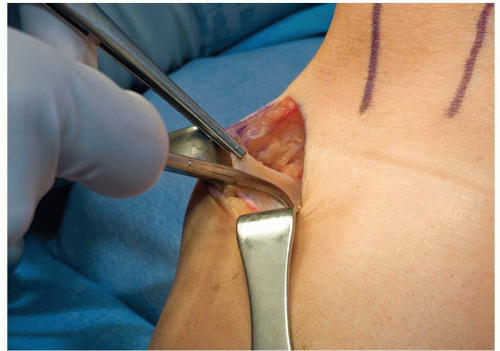 FIGURE 16.3 The sartorial fascia is incised and everted, exposing the gracilis and semitendinosus tendons. |
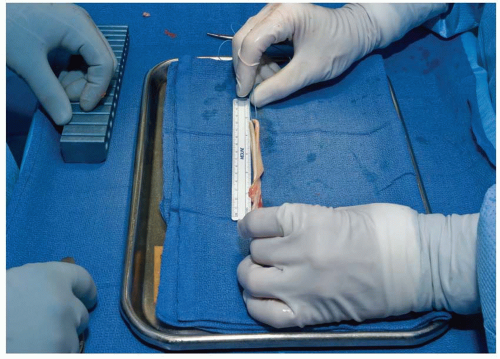 FIGURE 16.4 After removing the soft tissue debris from the graft, the tendon is doubled and measured in length. |
 Get Clinical Tree app for offline access 
|










