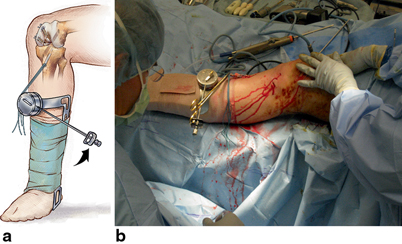
Fig. 21.1
The graft-tensioning boot consists of a frame that has a ratcheted torque wrench attached to the frame. The device fits over the surgical foot and leg. (From Fanelli 2013 [1]. Reprinted with permission)

Fig. 21.2
The graft-tensioning device is used to pretension the prepared allograft or autograft tissue prior to implantation. After completion of graft preparation, the allograft or autograft tissue is placed on the tensioning boot, and tension is gradually applied to pretension the graft tissue prior to implantation. The graft is wrapped in a damp sponge, and the tensioning boot graft assembly is protected on the back table until it is time to implant the allograft or autograft tissue. (From Fanelli 2013 [1]. Reprinted with permission)

Fig. 21.3
During the surgical procedure, the sterile tensioning boot is fitted over the surgical extremity foot and shin areas, and attached to the surgical leg with a sterile bandage. (From Fanelli 2013 [1]. Reprinted with permission)
Combined PCL ACL Reconstruction Surgical Technique Using Mechanical Graft Tensioning
My surgical technique for PCL reconstruction, and combined PCL ACL medial and lateral side reconstruction is presented in Chaps. 9 and 15 of this textbook. This chapter specifically addresses the surgical technique for posterior and ACL reconstruction using the Biomet graft-tensioning boot.
The patient is placed on the operating room table in the supine position, and after satisfactory induction of anesthesia, the operative and nonoperative lower extremities are carefully examined [1–11]. A tourniquet is applied to the upper thigh of the operative extremity, and that extremity is prepped and draped in a sterile fashion. The well leg is supported by the fully extended operating room table that also supports the surgical leg during medial and lateral side surgery. A lateral post is used to control the surgical extremity. An arthroscopic leg holder is not used. Pre- and postoperative antibiotics are given, and antibiotics are routinely used to help prevent infection in these time consuming, difficult, and complex cases. Allograft tissue is prepared prior to bringing the patient into the operating room. Autograft tissue is harvested prior to beginning the arthroscopic portion of the procedure.
The arthroscopic instruments are inserted with the inflow through the superolateral patellar portal. Instrumentation and visualization are positioned through inferomedial and inferolateral patellar portals, and can be interchanged as necessary. Additional portals are established as necessary. Exploration of the joint consists of evaluation of the patellofemoral joint, the medial and lateral compartments, medial and lateral menisci, and the intercondylar notch. The residual stumps of both the anterior and PCL are debrided; however, the posterior and ACL anatomic insertion sites are preserved to serve as tunnel reference points. The notchplasty for the ACL portion of the procedure is performed at this time.
An extra capsular extra-articular posteromedial safety incision is made by creating an incision approximately 1.5–2 cm long starting at the posteromedial border of the tibia approximately 1 in. below the level of the joint line and extending distally. Dissection is carried down to the crural fascia, which is incised longitudinally. An interval is developed between the medial head of the gastrocnemius muscle and the nerves and vessels posterior to the surgeon’s finger, and the capsule of the knee joint anterior to the surgeon’s finger. The posteromedial safety incision enables the surgeon to protect the neurovascular structures, confirm the accuracy of the PCL tibial tunnel, and to facilitate the flow of the surgical procedure.
The curved over-the-top PCL instruments (Biomet Sports Medicine, Warsaw, Indiana) are used to sequentially lyse adhesions in the posterior aspect of the knee, and elevate the capsule from the posterior tibial ridge. This allows the accurate placement of the PCL/ACL drill guide, and correct placement of the tibial tunnel.
The arm of the PCL /ACL guide (Biomet Sports Medicine, Warsaw, Indiana) is inserted through the inferior medial patellar portal. The tip of the guide is positioned at the inferior lateral aspect of the PCL anatomic insertion site. This is below the tibial ridge posterior and in the lateral aspect of the PCL anatomic insertion site. The bullet portion of the guide contacts the anteromedial surface of the proximal tibia at a point midway between the posteromedial border of the tibia, and the tibial crest anterior at or just below the level of the tibial tubercle. This will provide an angle of graft orientation such that the graft will turn two very smooth 45° angles on the posterior aspect of the tibia. The tip of the guide in the posterior aspect of the tibia is confirmed with the surgeon’s finger through the extra capsular extra-articular posteromedial safety incision. Intraoperative anteroposterior (AP) and lateral X-ray may also be used; however, I do not routinely use intraoperative X-ray. When the PCL/ACL guide is positioned in the desired area, a blunt spade-tipped guide wire is drilled from anterior to posterior. The surgeon’s finger confirms the position of the guide wire through the posterior medial safety incision.
The appropriately sized standard cannulated reamer is used to create the tibial tunnel. The surgeon’s finger through the extra capsular extra-articular posteromedial incision is monitoring the position of the guide wire. When the drill is engaged in bone, the guide wire is reversed, blunt end pointing posterior, for additional patient safety. The drill is advanced until it comes to the posterior cortex of the tibia. The chuck is disengaged from the drill, and completion of the tibial tunnel is performed by hand.
The PCL single- or double-bundle femoral tunnels are made from inside out using the double-bundle aimers, or an endoscopic reamer can be used as an aiming device (Biomet Sports Medicine, Warsaw, Indiana). The appropriately sized double-bundle aimer or endoscopic reamer is inserted through a low anterior lateral patellar arthroscopic portal to create the PCL anterior lateral bundle femoral tunnel. The double-bundle aimer or endoscopic reamer is positioned directly on the footprint of the femoral anterior lateral bundle PCL insertion site. The appropriately sized guide wire is drilled through the aimer or endoscopic reamer, through the bone, and out a small skin incision. Care is taken to prevent any compromise of the articular surface. The double-bundle aimer is removed, and the endoscopic reamer is used to drill the anterior lateral PCL femoral tunnel from inside to outside. When the surgeon chooses to perform a double-bundle double-femoral tunnel PCL reconstruction , the same process is repeated for the posterior medial bundle of the PCL. Care must be taken to ensure that there will be an adequate bone bridge (approximately 5 mm) between the two femoral tunnels prior to drilling. This is accomplished using the calibrated probe, and direct arthroscopic visualization of the PCL femoral anatomic insertion sites.
My preferred surgical technique of PCL femoral tunnel creation from inside to outside is for two reasons. There is a greater distance and margin of safety between the PCL femoral tunnels and the medial femoral condyle articular surface using the inside-to-outside method. In addition, a more accurate placement of the PCL femoral tunnels is possible, in my opinion, because I can place the double-bundle aimer or endoscopic reamer on the anatomic footprint of the anterior lateral or posterior medial PCL insertion site under direct visualization.
A Magellan suture retriever (Biomet Sports Medicine, Warsaw, Indiana) is introduced through the tibial tunnel into the joint, and retrieved through the femoral tunnel. The traction sutures of the graft material are attached to the loop of the Magellan suture retriever, and the graft is pulled into position. The graft material is secured on the femoral side using a bioabsorbable interference screw for primary aperture opening fixation, and a polyethylene ligament fixation button for backup fixation.
With the knee in approximately 90° of flexion, the ACL tibial tunnel is created using a drill guide. My preferred method of ACL reconstruction is the transtibial femoral tunnel endoscopic surgical technique. The arm of the drill guide enters the knee joint through the inferior medial patellar portal. The bullet of the drill guide contacts the anterior medial proximal tibia externally at a point midway between the posterior medial border of the tibia, and the anterior tibial crest just above the level of the tibial tubercle. A 1-cm or greater bone bridge exists between the PCL and ACL tibial tunnels. The guide wire is drilled through the guide and positioned so that after creating the ACL tibial tunnel, the graft will approximate the tibial anatomic insertion site of the ACL. A standard cannulated reamer is used to create the tibial tunnel.
With the knee in approximately 90–100° of flexion, an over-the-top femoral aimer is introduced through the tibial tunnel, and used to position a guide wire on the medial wall of the lateral femoral condyle to create a femoral tunnel approximating the anatomic insertion site of the anterior cruciate ligament. The ACL graft is positioned and fixation is achieved on the femoral side using a bioabsorbable interference screw, and cortical suspensory backup fixation with a polyethylene ligament fixation button. Additional drawings and photographs of this surgical technique are presented in Chap. 20 [9].
The Cyclic Dynamic Method of Cruciate Graft Tensioning
The cyclic dynamic method of graft tensioning using the Biomet graft-tensioning boot is used to tension the posterior and ACL grafts. During this surgical technique, the PCL and/or ACL grafts are secured on the femoral side first with the surgeon’s preferred fixation method. The technique described is a tibial-sided tensioning method. I routinely use polyethylene ligament fixation buttons for cortical suspensory fixation, and aperture interference fixation with bioabsorbable interference screws for femoral side PCL and ACL fixation. In combined PCL ACL reconstructions, the PCL graft is tensioned first, followed by final PCL graft(s) tibial fixation. The ACL graft tensioning and fixation follows that of the PCL.
With the tensioning boot applied to the foot and leg of the surgical extremity, tension is placed on the PCL graft(s) distally using the Biomet graft-tensioning boot (Biomet Sports Medicine, Warsaw, Indiana) (Fig. 21.4). Tension is gradually applied with the knee in 0° of flexion (full extension) reducing the tibia on the femur. This restores the anatomic tibial step-off. Although there are numbers on the torque wrench dial, these numbers are not used to set the tension. The numbers on the torque wrench serve as a reference point during the cycling process, and readjustment process, and are not indicators of final tension in the graft. The tension is determined by reduction of the tibia on the femur in 0° of knee flexion (full extension), the restoration of the anatomic tibial step-offs, a negative posterior drawer on intraoperative examination of the knee, and full range of motion of the knee. The knee is cycled through a full range of motion multiple times to allow pretensioning and settling of the graft. The process is repeated until there is no further change on the torque setting on the graft tensioner with the knee at 0° of flexion (full extension). When there are no further changes or adjustments necessary in the tension applied to the graft, the knee is placed in 70–90° of flexion, and fixation is achieved on the tibial side of the PCL graft with a bioabsorbable interference screw for interference fit fixation, and backup cortical suspensory fixation with a bicortical screw and spiked ligament washer or polyethylene ligament fixation button (Fig. 21.5).