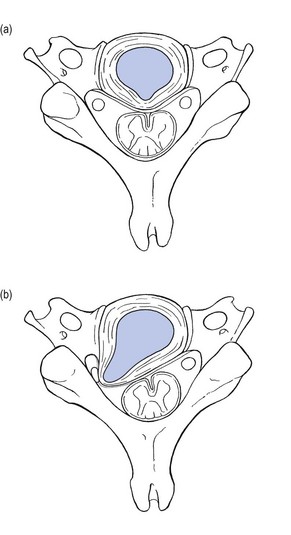
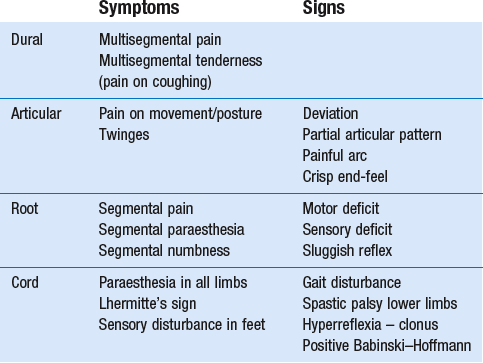
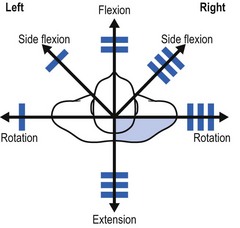
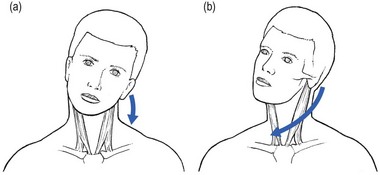
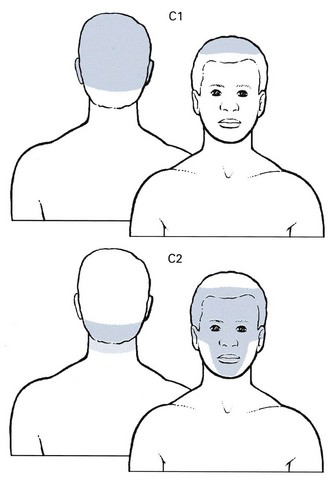
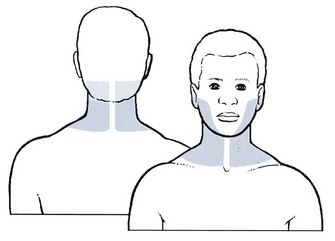
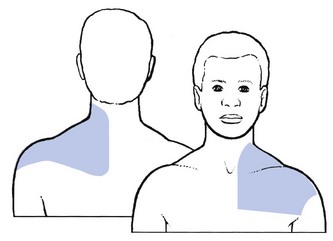
8 Mechanical disorders of the cervical spine affect the structures of the locomotor system. They are often related to the consequences of the ageing spine. Degenerative changes at the level of the intervertebral discs may lead to disc displacements and also to anatomical and biomechanical changes in ligaments, capsules, nervous tissue and vascular structures. In addition to this degeneration being responsible for the development of certain disorders, injuries and overuse may also lead to soft tissue lesions in the region of the neck (Box 8.1). Degenerative changes in the cervical spine are part of the normal ageing process and are almost ubiquitous in older people.1,2 Very often they remain asymptomatic.3,4 Therefore diagnoses such as ‘degeneration’, ‘arthrosis’, ‘osteophytosis’, ‘spondylosis’ or ‘spondylarthrosis’ based on incidental radiological findings are still too easily made. Throughout the literature, a discrepancy between the discovery of structural changes and the presence of symptoms is a consistent finding.5 It has been shown that, in the first two decades of life, lateral tears occur in the annulus fibrosus. They tend to develop joint-like structures – the uncovertebral joints – that then begin to undergo transformation.6 In the second and third decades, the lateral tears enlarge towards the medial part of the disc, often ending in a complete transverse splitting of the disc into equal halves. These anatomical changes cause instability of the disc and favour the possibility of cartilaginous displacements, either of the annulus fibrosus or of the nucleus pulposus (see below: disc displacements). See Chapters 31 and 32 for an extensive explanation of the function and behaviour of the lumbar disc, which is highly comparable to the situation in the cervical spine. The prevalence of cervical facet joint degeneration is very high in individuals aged 50 years and more, with a tendency to increase in severity with age. Diminution of the height of the disc and the subsequent reversal from lordosis to kyphosis result in a greater transmission of shearing forces to the facet joints. They start to bear weight and this furthers the degenerative process. This is characterized by fibrillation and erosion of the articular cartilage, partial or complete denudation of the cartilage, and new bone formation.7 Later in life, subperiosteal osteophytes with periarticular fibrosis develop, resulting in a gross decrease in mobility.8 All levels of the middle and lower cervical spine are affected to almost the same degree, whereas in the lumbar spine there is an increase in degeneration towards the lower levels.9 Circular disc displacement, as is seen when the disc has degenerated entirely, may further the development of osteophytic outcrops on all sides, and thus also into the spinal canal, threatening the spinal cord.10 Once the bony parts formed by the uncovertebral joints touch each other, further loss of height can only happen anteriorly. Because of the decrease in height in the anterior column of the cervical spine, cervical lordosis may diminish and even disappear, resulting in the typical position of the degenerated neck – the chin projected forwards. Retrolisthesis in the mid-cervical area (C3–C6) is a common finding in spondylarthrosis. Also, buckling of an enlarged ligamentum flavum narrows the spinal canal, especially during extension of the neck.11,12 The association of diminished intervertebral space, osteophyte formation at both the uncovertebral and zygapophyseal joints, and hypertrophy of the facet joint capsules causes diminution of the intervertebral foramen and eventual neural foraminal encroachment.13 Further diminution of the foraminal space is caused by the backwards slip of the upper vertebra during extension.14 Degenerative changes of the cervical spine are common in both symptomatic and asymptomatic adults. At the age of 50, spondylosis is visible on plain X-rays in more than 50% of asymptomatic people.15 A magnetic resonance imaging (MRI) study on 500 asymptomatic subjects could detect disc degeneration in 17% of discs in men and in 12% of those of women in their twenties, and 86% and 89% of discs in both men and women over 60 years of age. Posterior disc protrusion with demonstrable compression of the spinal cord was observed in 7.6% of subjects over 50 years of age.16,1 The clinical question is whether the patient’s symptoms are caused by the changes that are seen on imaging. Unfortunately, even the most sophisticated imaging studies do not show pain, but only structural abnormalities that may or may not be the cause of the patient’s symptoms.4,17 Symptomatic disc displacements in the cervical spine are more common than is generally believed. They can occur at any age from childhood onwards but present with different clinical syndromes, depending on the age group.18 Cartilaginous displacements are most frequent at the C6–C7 and C5–C6 joints. They are occasionally found at the C4–C5 or C7–T1 joints, and rarely at the C2–C3 or C3–C4 joints.19 Nuclear prolapses are very uncommon, except in young people. It was to Cyriax’s credit that he recognized the clinical pictures associated with disc displacements and made an inventory of symptoms and signs. A distinction can be made between posterocentral and posterolateral displacements resulting respectively in discodural and discoradicular interactions. It is important to remember that diagnoses are made on clinical grounds, following the patient’s history and the functional examination. Technical investigations that rely only on anatomical findings lead very easily to misinterpretation.17 They can sometimes be used to confirm a diagnosis, rather than to make one. Discs may displace in two ways: either they move posteriorly to compress dura and/or cord, or they move posterolaterally to compress the nerve root. Posterior migration of disc tissue beyond the posterior limits of the intervertebral joint space causes pressure on the posterior longitudinal ligament and, via the ligament, on the anterior part of the dura mater. This produces multisegmental pain with dural reference, mostly in the trapezius and scapular area but possibly towards the head and/or pectoral area (see Ch. 7). The pain is the result of a discodural interaction: irritation of the anterior structures in the spinal canal is responsible for the dural symptoms. Pure posterocentral compression gives rise to pain felt centrally and/or bilaterally. Compression just laterally from the midline will result in pain that is felt unilaterally but is still multisegmental. The internal derangement in the intervertebral joint provokes articular signs demonstrable on functional examination. Disc displacements also behave according to their actual status of degeneration. Cyriax described seven stages of disc lesions, each one typical of a certain age group and characterized by a typical history (Fig. 8.1).20 It is believed that disc degeneration and disc displacements are of themselves painless events. It is only when pain-sensitive structures in the neighbourhood pick up on the disc abnormality and translate mechanical pressure and inflammatory changes into pain that signs and symptoms originate. The reader is referred to Chapter 33 – the ‘dural concept’ – for a thorough description of this dural hypothesis. When a fragment of disc (at any level) protrudes posterocentrally, it may compress the dura mater either in the midline, which results in central or bilateral pain, or slightly to one side, leading to pain felt unilaterally. The dura mater, being a multisegmentally innervated tissue, translates this compression into multisegmental pain (see Ch. 1). Pain reference from the cervical dural mater may thus spread up to the head and down to the mid-thoracic region, and may be felt anywhere in this area (Fig. 8.2). However, the pain is most commonly experienced in the region of neck, trapezius and scapula (Fig. 8.3a). Occasionally it is felt in the clavipectoral area or in the axilla (Fig. 8.3b). Patients often mention a tender spot, usually somewhere at the superior border of the trapezius, which they identify as the source of their pain. On palpation the examiner indeed finds localized tenderness. However, during the examination, movements designed to test the trapezius muscle are found to be negative. Furthermore, the tender spot may shift during neck manipulation and disappears when a full and painless range is obtained. This confirms that the tenderness is clearly a referred phenomenon (see Ch. 1) without localizing or diagnostic value. This multisegmental tenderness is one of the dural symptoms and results from dural compression at any level. Dural signs are not found on examination. Although neck flexion stretches the dura mater, the pain very often experienced during this movement must be regarded as an articular sign rather than a dural one. Neck flexion can only be regarded as being a dural test if it stretches the dura from a distance, which is not the case here. There is also no equivalent to the straight-leg raising test in the lumbar examination where a simple movement (hip flexion with an extended knee) allows differentiation between dural pain, root pain and muscular tightness. Some nerve roots (C4–C6) are tethered to the gutter of their respective transverse process,21 but apparently not to the foramen.22 Some authors have developed and discussed ‘upper limb tension tests’ (ULTT) as a valuable examination procedure for patients with neck problems with or without radiation down the upper limb.23,24 The aim would be to create stress, transmitted to the structures in the spinal canal via the peripheral nerves (median–radial–ulnar). The peripheral nerves in the upper limb however, have, unlike those in the lower limb, a more complex course. It is therefore more difficult to carry out ‘pure’ movements and, although these tests stress the neurological tissues, they also stress some contractile and inert tissues in neck, shoulder girdle and arm. Because of their low specificity, 25–27 they are not integrated into the standard functional examination of the cervical spine. On examination, a partial articular pattern of internal derangement is found: some active movements are painful and limited or cause pain at the end of range, while others are negative or clearly less positive. The asymmetrical pattern that occurs may vary from very subtle, with hardly any limitation, to very pronounced with some movements completely blocked, forcing the head in a deviated position. A minimal partial articular pattern (Fig. 8.4a) emerges when the internal derangement is minor and the discodural interaction slight. It is hypothesized that pronounced signs result from a severe discodural interaction (Fig. 8.4b). Passive movements usually hurt more than active ones, though cases may be encountered in which passive movements ease the pain. Resisted movements are negative, except perhaps resisted flexion. The latter may slightly increase the pain in more acute cases, presumably as a result of the consequent compression strain on the affected joint. When neck flexion elicits pain in the upper thoracic area, further examination of neck, shoulder girdle and thorax must differentiate between a cervical lesion with pain reference to the upper thorax and a lesion in the shoulder girdle or upper thoracic spine. The movement is an articular sign for the cervical spine but is also regarded as a dural sign for the thoracic spine. During neck flexion the dura mater is stretched and drawn forward against an eventual upper thoracic protrusion (see Ch. 25). By analogy with the lumbar spine, where backache may evolve into sciatica, cervicoscapular pain may be replaced by brachial pain. The original multisegmental cervicoscapular pain disappears and severe and strictly segmental pain down the arm supervenes. The examiner must be aware that patients sometimes omit to mention the original pain in the trapezius or scapular area but concentrate only on the severe symptoms at presentation. This change in pain localization is the result of the disc moving laterally (Fig. 8.5). Pressure on the dura mater ceases when the dural sleeve of the nerve root becomes compressed and radicular pain appears. Increasing compression of the nerve root is translated into increasing symptoms and signs. Paraesthesia and/or numbness point towards involvement of the nerve root fibres and are usually felt in the distal part of the corresponding dermatome. Additional tests to provoke radicular pain can be added. During the Spurling test, the patient side-flexes the head to the affected side first, followed by the unaffected side. Meanwhile the examiner presses straight down on the head.28 A test result is classified as positive if pain radiates into the arm towards which the head is side-flexed during compression. Alternatively the head is rotated and side-flexed to the same side during compression.29 This is called the ‘maximal cervical compression test’. Great care is needed while performing this test as it also compresses the vertebral artery. Most patients wake in the morning with a stiff neck. Pain and stiffness increase as soon as they adopt an upright position. Any attempt to move the neck results in unilateral pain, radiating to trapezius and/or upper scapular area. Occasionally the symptoms come on suddenly as the result of a certain movement (e.g. bending over a washbasin), trivial trauma (e.g. a blow to the head30) or coughing. On examination, gross and obvious articular signs are found: a striking and extremely painful limitation of one rotation and one lateral flexion towards the same side, usually the painful side. Often no movement is possible in either of these directions (Fig. 8.6). The other movements are much less painful and are scarcely limited, except possibly extension. The end-feel is empty or one of severe muscle guarding. The pattern of limitation is diagnostic. Acute torticollis is the most striking example of a partial articular pattern, which indicates that part of the joint is blocked by an intra-articular displacement. In most instances the displacement is nuclear: the nucleus has oozed out slowly during the night, while the patient has being lying for some hours with the neck in side flexion or rotation. The dura mater becomes compressed and irritated, which causes the cervicoscapular pain. A sudden onset suggests an annular displacement. It usually occurs in patients over 30. This mechanism was hypothesized by Cyriax more than 50 years ago and was recently proven by two MRI studies. Maigne et al performed MRI in a 15-year-old male adolescent, a few hours after the onset of torticollis. Increased signal intensity compatible with a fluid collection was seen in the right uncovertebral region at C2–C3, causing excessive lateral pressure and pushing C2 outwards. A new MRI taken 3 weeks after resolution of symptoms was unremarkable.31 Another MRI study performed by Gubin et al in ten children and adolescents with acute torticollis showed similar findings: high-intensity zones were seen near uncovertebral zones C2–C3 or C3–C4. The zones were always on the side where the patients felt pain and disappeared spontaneously after a few days.32 The characteristics of acute unilateral torticollis are listed in Box 8.2. Torticollis in infancy and childhood Osseous lesions are mostly anomalies of the atlas,33 such as hemiatlas, partial atlantic aplasia34 or partial atlanto-occipital fusion,35 and Klippel–Feil syndrome. Klippel–Feil syndrome is congenital fusion of two or more cervical vertebrae. The classic clinical triad is: lower neckline, short neck, and restriction of head and neck movements.36 In patients with moderate involvement, this classic triad may not be seen and sometimes there is only some scoliosis deformity or moderate torticollis.37 Congenital muscular torticollis (CMT) is caused by shortening of the sternocleidomastoid muscle. This leads the head to bend toward the affected side and the chin to turn to the opposite side, the so-called cock robin position of the neck. CMT is the third most common congenital musculoskeletal anomaly after dislocation of the hip and clubfoot,38 with a reported incidence of 0.3–1.9%.39 Various theories have been proposed but the true aetiology of torticollis remains uncertain.40 As a result of fibrotic changes of the sternocleidomastoid muscle, the unilateral contracture may subsequently result in plagiocephaly, skull and facial asymmetry.41 When diagnosed early, CMT can be managed conservatively and seldom requires surgery.42 In fact, a simple stretching programme leads to spontaneous resolution in most patients.43 In children older than 1 year, corrective surgery has both cosmetic and functional benefits, the best outcomes being obtained between the ages of 1 and 4. After the age of 5, the form and efficacy of treatment are controversial.44 Acquired torticollis in children should always be taken seriously, as it may result from a number of underlying causes, some of which are severe and life-threatening. Spontaneous subluxation of the atlantoaxial joint following peripharyngeal inflammation is known as Grisel’s syndrome. Children between 5 and 12 years are most frequently affected. However, the condition has been reported in patients ranging from infancy to the seventh decade of life.45 Torticollis may occur shortly after the onset of the underlying infection or it may follow mild trauma to the neck. The syndrome has been reported in association with rhinopharyngitis,46 cervical osteomyelitis, rheumatic conditions, and following surgical procedures such as tonsillectomy or adenoidectomy,47 choanal atresia repair and mastoidectomy. It is hypothesized that distension and abnormal laxity of the ligaments surrounding the atlantoaxial articulation result from direct spread of inflammation from the pharynx and nasopharynx.48 This leads to C1–C2 instability with subluxation and (sometimes) devastating neurological sequelae (between 10 and 15% of patients have neurological signs or symptoms, with serious consequences including quadriplegia and sudden death49). The condition begins with a spasm of the irritated sternocleidomastoid muscle. This contraction leads to a typical position of the head, which is easily differentiated from the position in acute discogenic torticollis. In a disc lesion, the deviation is purely in lateral flexion or flexion or a combination of both. When a spasm of the sternocleidomastoid muscle is responsible, the neck is held in flexion, side flexion towards and rotation away from the painful side (signe du merle or ‘blackbird’s sign’) (Fig. 8.7).50 Benign paroxysmal torticollis is a relatively uncommon, self-limiting condition occurring during infancy. It resolves by the age of 2–3 years. Periodic episodes of torticollis may randomly alternate from side to side and be associated with vegetative symptoms. The aetiology is unknown and no treatment is effective.51 Spasmodic torticollis or cervical dystonia is the most frequently occurring focal dystonia, with an incidence of 8.9 per 100 000 people.52 Dystonia is defined as sustained, involuntary muscle contractions, which often cause twisting or repetitive movements or abnormal postures. The origin of the symptoms is still unclear. The condition often results in cervical pain and disability as well as impairments affecting postural control.53 Therapy of spasmodic torticollis includes behaviour modification, such as training the patient to readjust the position of the head, and biofeedback, hypnosis and anticholinergic drugs.54 When these procedures are not successful, local application of botulinum toxin A offers a highly effective treatment technique. Botulinum toxin A is injected into the overactive, dystonic cervical musculature to provide a graded, reversible denervation of the neuromuscular junction by preventing the release of acetylcholine from the presynaptic axon of the motor end plate. Botulinum treatment showed success rates ranging from approximately 60 to 90%.55,56 Surgical intervention is used when a patient has not responded to other interventions. Although a variety of surgical techniques have been studied, the most commonly used approach is selective peripheral denervation.57 The presence of a compensatory thoracic curve following cervical scoliosis indicates the possibility of adolescent scoliosis, unilateral cervical rib, Klippel–Feil deformity58 or previous thoracoplasty. Treatment is by manipulation. The technique is adapted according to the clinical picture. Acute torticollis in patients under 30 often behaves in a nuclear manner; these patients should be treated with ‘nuclear’ techniques – progressive sustained rotation and/or lateral flexion, whereby an attempt is made to push the displaced nuclear material slowly back. The less common annular cases should be treated with the usual ‘annular’ manipulation techniques (see Ch. 11). A mild partial articular pattern is found (Fig. 8.8). As a rule, two, three or four movements out of the six are painful, and four, three or two prove painless. Passive movements are usually more painful than active ones. There may be minor limitation, or a painful arc is found. The end-feel is rather crisp, indicating the muscle guarding typical of a disc lesion, but it is not uncommon to find a normal, capsular end-feel. Root and cord signs are absent. It is not easy to determine the level at which the protrusion lies, because any disc at any level gives rise to the same symptoms (multisegmental pain) and signs (partial articular pattern). Oscillatory techniques on a sitting or prone lying patient or anteroposterior gliding movements with the patient lying supine may sometimes provoke the pain and give an idea as to the level but this cannot always be relied upon. The differential diagnosis includes lesions in the shoulder girdle (e.g. posterior sternoclavicular syndrome, see online chapter Interpretation of the clinical examination of the shoulder girdle), in the upper thoracic area (see Ch. 26), internal disorders (e.g. in the heart, lungs or diaphragm, see Ch. 28) and neurological conditions (e.g. long thoracic or spinal accessory neuritis, see online chapter Nerve lesions and entrapment neuropathies of the upper limb). Unilateral pain in the cervicoscapular area is highly suitable for manipulation. Usually a few sessions suffice to restore a full and painless range of movement. The patient must be informed that the disc may move again, however, and that recurrences are not uncommon. Each new attack should be treated in a similar way. However, when there is a tendency to recurrence, prophylactic measures should be taken (i.e. position at work, sleeping position, collar, exercises – see Ch. 13). See Box 8.3 for a summary of unilateral pain in the neck, trapezius or scapular area. Root pain as the result of a disc protrusion pressing on the dural investment of a cervical nerve root is quite common. It has an incidence rate of 1/1000 per year with a peak age between 45 and 54. The lesion very seldom occurs in adolescence. In younger patients suffering from cervical root pain, other disorders must be excluded before a disc lesion is considered. Over the age of 60, root pain caused by a discoradicular interaction is also rare, whereas an osteophytic or metastatic compression becomes more likely (Box 8.4).59 As a rule, the patient has had a history of recurrent bouts of unilateral cervicoscapular pain over the past years. The present symptoms start with the usual scapular pain, but this time they do not resolve spontaneously. On the contrary, one day the scapular pain may have become much worse and strictly unilateral, subsequently shifting to shoulder and arm (Box 8.5). The scapular pain then disappears or diminishes to a degree that it is no longer worthy of mention, whereas pain in the arm increases and remains severe for 1–2 months. The ache is sharp and permanent, and prevents the patient from sleeping. Sometimes the patient can only achieve rest by bringing the arm above the head – a position that relieves tension on the roots but also widens the intervertebral foramen and diminishes the pressure.60,61 This sign is highly suggestive of a discoradicular conflict, but is unlikely to be present in radiculopathy caused by spondylosis.62 The arm pain may be accompanied by pins and needles in some fingers, later followed by numbness. In order to make the differential diagnosis with other lesions that provoke paraesthesia, it is vital to collect more information about its behaviour: how far proximally does the paraesthesia spread, which fingers and what parts of them are involved, and when precisely are the pins and needles felt? A typical feature is that the paraesthesia has neither edge nor aspect within the fingers. Stroking the skin may provoke or increase pins and needles but moving the digits has no influence. Paraesthesia comes and goes, day or night, in an erratic fashion, appears without any definite reason and does not last for more than an hour at a time. In difficult cases, diagnostic traction may help: if the paraesthesia disappears during manual traction at the head and comes back when traction is released, the cause is clearly cervical.63 In most cases pain and paraesthesia disappear spontaneously, 6–10 weeks after the onset of the brachial pain. It may take months for the numbness to disappear completely. The patient is asked about the precise location of the pain, which will enable the examiner to determine the dermatome and affected root. However, it is important to mention that the localization of the arm pain is not always a reliable localizing sign. Due to the high incidence of intradural connections between the dorsal rootlets of C5, C6 and C7 segments, there can be overlap between dermatomes, with one dermatome encompassing one or two adjacent segments.64,65 It may therefore be possible for an individual to have a dermatomal distribution that fails to match the classic pattern precisely. A better pointer to the level of compression is paraesthesia, and therefore, if the patient mentions pins and needles, more details should be sought about their localization. Articular signs may be present but are not paramount. Usually only a slight partial articular pattern of internal derangement is seen; as the protrusion lies more outside the joint and the articular movements no longer interfere with it, articular signs are less important than root signs. Some active and passive movements may provoke or increase pain in the scapular area. The end-feel is crisp. It is possible, although not at all common, for neck movements to influence the pain and/or the pins and needles down the arm. The Spurling manœuvre (a downwards pressure on an extended and rotated neck) may also elicit radicular pain and paraesthesia.28 Resisted movements of the head are negative. Weakness indicates which nerve root has become compressed. The degree of motor deficit can be very subtle. The examiner should therefore compare both sides carefully.65 Gross weakness (3+ or 4) is a warning sign, indicating that the lesion is very probably non-discogenic in nature. Cutaneous analgesia is sought at the fingers and the reflexes are tested. An uncomplicated discoradicular interaction does not cause cord signs. The nerve roots most frequently compressed by a disc are, in order of frequency, C7 (56–70%), C6 (19–25%), C5 (2–14%) and C8 (4–10%).66 Each nerve root lesion, whatever its cause may be, gives rise to pain felt in the skin area corresponding with the segment to which the nerve root belongs. The pain is the result of involvement of the dural sheath surrounding the nerve fibres. When the nerve parenchyma becomes affected too, paraesthesia will be felt down the nerve distribution in the arm. However, variations in the nerve distribution may occur,67–69 and pain and paraesthesia may be felt in areas which do not totally correspond to one specific dermatome. More involvement of the nerve fibres causes weakness of the muscles belonging to the same segment and cutaneous analgesia in some (mostly the distal) part of the dermatome. One should bear in mind that other (non-neural) soft tissue lesions may lead to exactly the same segmental pain.70 Therefore resisted tests, undertaken to examine nerve root conduction, also serve to test for alternative causes of pain down the limb. The absence of discs at the first two cervical levels implies that nerve root compression by discs cannot occur. Reference of pain to the C1 or C2 dermatomes (headache; Fig. 8.9) does not always mean that C1 or C2 nerve roots are involved; the pain may be multisegmental and the result of compression of the lower cervical dura by a posterocentral disc protrusion.71,72 The C2 spinal nerve has a close proximity to the lateral capsule of the atlantoaxial (C1–2) zygapophyseal joint and innervates the atlantoaxial and C2–3 zygapophyseal joints; therefore, trauma to or pathologic changes around these joints can be a source of referred headache. This occurs especially in elderly patients with gross unilateral arthrosis of the atlantoaxial joint. It causes unilateral deep or dull pain that usually radiates from the occipital to parietal, temporal, frontal and periorbital regions. Ipsilateral eye lacrimation and conjunctival injection are common associated signs.73 Clinical examination shows a marked full articular pattern in which rotation is especially limited. Compression of the third cervical nerve root by a posterolateral disc displacement is very rare. Pain is felt at the lateral aspect of the neck and is referred to the occipital and temporal regions and the posterior part of the cheek. Pins and needles or numbness may be present (Fig. 8.10). Weakness is clinically not detectable. Cutaneous analgesia is uncommon, but if it occurs, it occupies any part of the lateral aspect of the neck. Most C3 pain stems from the C2–3 zygapophyseal joint. This joint and the third occipital nerve appear most vulnerable to trauma from acceleration–deceleration (‘whiplash’) injuries of the neck.74 Pain in this region may also result from pressure on the dura mater at any level and is then multisegmental. Heart disease may also give rise to reference of pain in the C3 dermatome. Another possibility is a trigeminal neuritis, which is characterized by paroxysms of severe, lancinating, electric bouts of pain restricted to the distribution of the trigeminal nerve.75 Discogenic lesions of the fourth cervical nerve root are rare. Pain spreads from the lower half of the neck towards the point of the shoulder (Fig. 8.11). Paraesthesia seems not to occur at this level. In theory, weakness of the trapezius muscle should be found but in practice muscular weakness is not detectable. A horizontal band of cutaneous analgesia may be found along the spine of the scapula, the mid-deltoid area and the clavicle.
Mechanical disorders
Degeneration and anatomical changes
Ageing of the cervical spine
Ageing of the cervical disc
Consequences of disc ageing for surrounding structures
Effects on the facet joints
Effects on the spinal canal
Effects on the intervertebral foramen
Radiological changes
Pathology
Disorders of the disc: disc displacements
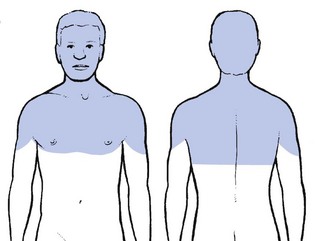
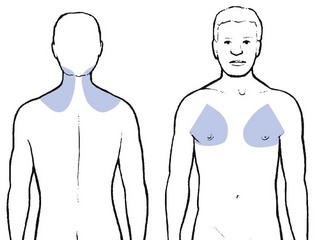
Posterocentral displacement
Posterolateral displacement
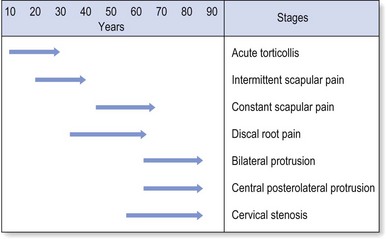
Stages of disc displacement
Findings on examination
Dural symptoms
Dural signs
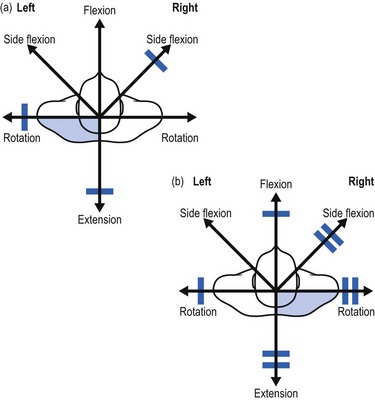
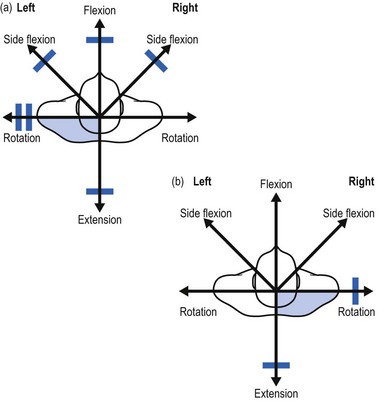
Articular symptoms and signs
Root symptoms and signs
Common syndromes
Acute torticollis: unilateral pain with asymmetrical picture
History
Examination
Diagnosis
Differential diagnosis
Treatment
Unilateral cervicoscapular pain
Examination
Differential diagnosis
Treatment
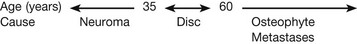
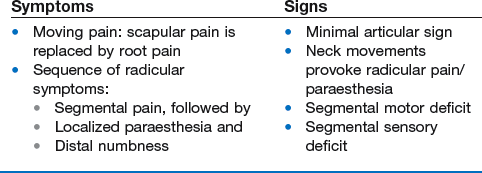
Unilateral root pain
History
Examination
Different root syndromes and their differential diagnosis