CHAPTER 23 Massive, Irreparable Rotator Cuff Tears
Rotator cuff disease is one of the most common reasons why patients seek medical attention. The prevalence of full-thickness tears increases substantially with age, and many of these tears go undetected because of a lack of symptoms. Tempelhof and colleagues1 have evaluated 411 asymptomatic adult shoulders ultrasonographically in patients older than 50 years. There were 96 (23.4%) full-thickness tears with an increased prevalence and tear size each decade (age, prevalence: 50-59, 13%; 60-69, 20%; 70-79, 31%; older than 80, 51%). In a similar study, Yamaguchi and associates2 performed bilateral ultrasound on 588 patients who presented with unilateral shoulder pain. There were 376 full-thickness tears discovered, 83 (22%) of which were asymptomatic. The authors reported an approximately 10-year difference between three subgroups of patients; the average age was 48.7 years for patients with no rotator cuff tear, 58.7 years for those with a unilateral tear, and 67.8 years for those with a bilateral tear. Patients who have asymptomatic full-thickness rotator cuff tears represent a population at risk because the natural history of these tears is that they progress and can result in eventual disability because of limited treatment options for those patients whose tears progress beyond a state of repair.
When a patient presents with a symptomatic, full-thickness rotator cuff tear, it is difficult to argue against repair as the optimal treatment for those patients who are willing and able to undergo surgery and the required postoperative rehabilitation. However, there are patients whose tears are irreparable, thereby presenting a difficult challenge to the treating orthopedic surgeon. Rockwood and coworkers3 have reported an 83% patient satisfaction rate in 53 shoulders at an average of 6.3 years after open subacromial decompression and débridement of irreparable rotator cuff tears. The authors cited prior studies that demonstrated durable results in patients whose rotator cuff repairs failed, but who also underwent subacromial decompression. It was concluded that the improvements noted may, therefore, be caused by subacromial decompression and débridement of the torn cuff. Since the publication of their results, several studies4–7 have demonstrated lasting pain relief but variable functional gains from débridement and subacromial decompression, whether performed as an open repair or arthroscopically. Many of these studies compared cuff repair with decompression and débridement, and patients who underwent successful repair fared better in the long term. Certainly, rotator cuff repair should be attempted when possible, but irreparable lesions of the rotator cuff are a separate entity and the treatment, rehabilitation, and goals of therapy should be as well.
ANATOMY AND PATHOANATOMY
Irreparable Cuff
The rotator cuff consists of four muscles—subscapularis, supraspinatus, infraspinatus, and teres minor—whose tendons coalesce to envelop the humeral head at the anatomic neck. This design enables the rotator cuff to function as a unit to stabilize the humeral head in the center of the glenoid cavity throughout the full range of shoulder motion. Full-thickness rotator cuff tears have been classified according to cause, age of the tear, size, shape, number of tendons, and topography or trophicity.8 For the purpose of this chapter, focus will remain on tears that are massive and irreparable; these are tears that are chronic (longer than12 months), involve two or more tendons (more than 5cm in maximum dimension), are retracted to the glenoid margin, and/or demonstrate poor muscle trophicity on computed tomography (CT) or magnetic resonance imaging (MRI).
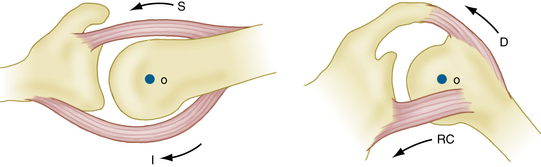
The symptoms most often associated with irreparable rotator cuff tears are pain and functional limitation. Pain can be the result of mechanical, biologic, and/or neurologic factors,9,10 any of which can mask a functional rotator cuff tear. Burkhart9 has described five essential biomechanical criteria that must be met for a tear to retain function (Table 23-1). Perhaps the most crucial of these is the integrity of the force couples about the glenohumeral joint. The remaining four criteria are a function of tear size, tear location, and degenerative condition of the tendon, all of which are important but may be considered in direct relation to the integrity (or lack thereof) of the glenohumeral force couples. Force couples exist in the coronal and transverse planes, and represent the contribution of the rotator cuff to dynamic glenohumeral joint stability during active flexion and abduction (Fig. 23-1). For review, a force couple is defined as two equal but oppositely directed forces that act simultaneously on opposite sides of an axis of rotation. Translational forces are cancelled out, linear motion is eliminated, and torque is produced. Inman and colleagues11 have described the coronal plane force couple, which provides superior-inferior stability by depressing the humeral head as resistance against the upward force of the deltoid during active abduction. Loss of the coronal plane force couple results in superior head migration, but not necessarily loss of daily function. The transverse force couple12 is composed of the subscapularis anteriorly and the infraspinatus–teres minor posteriorly, and provides anteroposterior glenohumeral stability throughout active abduction. Disruption of the anterior or posterior contribution of the transverse force couple results in loss of concavity compression, a pathologic increase in translation or subluxation of the humeral head toward the cuff deficiency, and decreased active abduction.13 As such, these patients will often complain of pain and loss of function.
TABLE 23-1 Biomechanical Criteria of Functional Rotator Cuff Tear
| Grade | Description |
|---|---|
| 1 | Force couples must be intact in the coronal and transverse planes. |
| 2 | A stable-fulcrum kinematic pattern must exist. |
| 3 | The shoulder’s suspension bridge must be intact. |
| 4 | The tear must occur through a minimal surface area. |
| 5 | The tear must possess edge stability. |
From Burkhart SS. Reconciling the paradox of rotator cuff repair versus débridement: a unified biomechanical rationale for the treatment of rotator cuff tears. Arthroscopy. 1994;10:4-19.
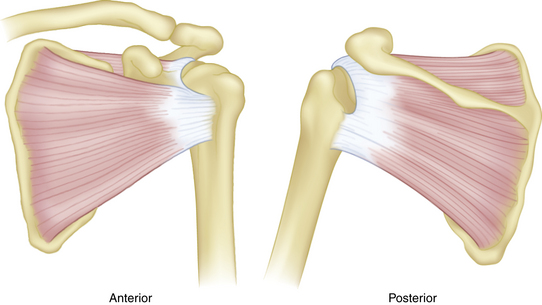
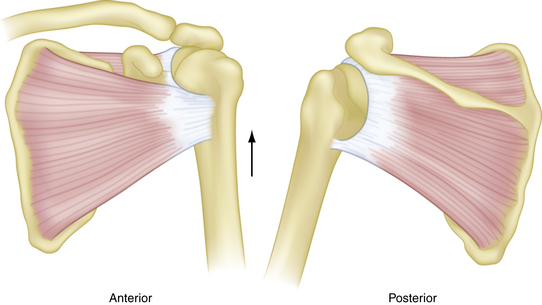
The importance of tear size and location on the transverse force couple, and the subsequent effects on function were further demonstrated by Burkhart in a fluoroscopic evaluation of 14 patients with massive rotator cuff tears.14 His observations have led to the description of three kinematic patterns (Figs. 23-2 to 23-4): type I, stable fulcrum; type II, unstable fulcrum; and type III, captured fulcrum. In essence, functional tears retain a critical portion of the anterior (subscapularis) and posterior (infraspinatus–teres minor) limbs of the transverse force couple, and the tear does not extend below the equator of the humeral head.
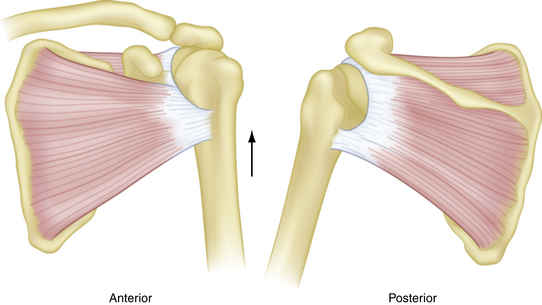
FIGURE 23-4 Captured fulcrum kinematics. A complete tear of the supraspinatus with extension anteriorly and posteriorly disrupts the coronal plane force couple to allow proximal humeral head migration. Patients may still be able to elevate the extremity if deltoid strength is sufficient.
(From Burkhart SS. Fluoroscopic comparison of kinematic patterns in massive rotator cuff tears. Clin Orthop Relat Res. 1992;(284):144-152.)
The integrity of the transverse force couple does not always correlate with patient function. Kelly and associates15 have performed electromyography on normal controls, and compared their muscle firing patterns with those of patients who had symptomatic and asymptomatic combined tears of the supraspinatus and infraspinatus tendons. None of the subjects had glenohumeral or acromioclavicular degenerative changes. Symptomatic and asymptomatic rotator cuff tears demonstrated increased muscle firing patterns compared with controls. Asymptomatic patients had increased firing in the intact subscapularis, whereas symptomatic patients demonstrated increased firing of the torn supraspinatus and infraspinatus musculature, with compensatory periscapular muscle recruitment and overall symptomatic shoulder dysfunction. It was unclear why patients who had similar tear patterns demonstrated different muscle firing patterns.
Biceps Tendon
The long head of the biceps tendon, described as the fifth tendon of the rotator cuff,16 is thought to contribute to shoulder flexion and abduction and provide glenohumeral joint stability during rotation. Warner and McMahon17 have provided radiographic evidence of the superior stabilizing effect of the biceps tendon. On the other hand, Yamaguchi and coworkers18 have performed an electromyographic evaluation of biceps activity during 10 basic shoulder motions and reported very little biceps activity. Although its functional contributions may be debatable, lesions of the biceps tendon often coexist with massive rotator cuff tears and can be a significant source of pain. Walch and colleagues19 and Boileau and associates 20 have reported reliable pain relief and improved function after arthroscopic biceps tenodesis or tenotomy in patients who had irreparable massive rotator cuff tears with an intact teres minor, no pseudoparalysis, and no severe rotator cuff arthropathy.
Other Pathologic Entities
There are other pain generators that can cause functional limitations and should be evaluated clinically to determine whether they play a role in the patient’s symptoms. The acromioclavicular (AC) joint begins to degenerate during early adulthood, and is a common source of pain in patients who have rotator cuff disease. Arthroscopic resection of the distal clavicle, without destabilizing the AC joint, is a reliable method to relieve pain sufficiently to restore a degree of function.21 Subacromial bursitis is associated with increased expression of substance P in the primary afferent nerves of the bursal tissue, and is associated with chronic pain. Glenohumeral arthritis can stimulate local or proliferative synovitis, which is another potential source of pain.
CLINICAL EVALUATION
History
Patient age has important implications about the quality of the cuff tissue and the size of the tear. Older patients often present with painful, chronic, atrophic large or massive rotator cuff tears and a progressive loss of shoulder function. Cuff tissue in these patients may be less amenable to repair. Younger patients will more often describe an acute event that precipitated symptoms of pain and functional loss, and their tissues will most likely be healthier and more likely to heal. These probabilities are based on two broad categories of patients and it is important not to focus solely on age. Hattrup22 is often referenced for qualifying 65 years of age as the point at which results of rotator cuff repair decline. He reported 77% excellent results in patients older than 65 years and 89% excellent results in patients younger than 65 years after open repair of rotator cuff tears of all sizes. In this study, as patients aged, tear size increased and results declined. However, pain relief and patient satisfaction were high in both groups. Hence, these results do not make a solid argument against repair based solely on patient age.
The duration of symptoms also provides a clue to the quality of the cuff tissue, amount of retraction, and overall reparability of the tendons. Lam and Mok23 have reported 44% good or excellent and 23% poor results after open repair of massive (more than 5 cm) rotator cuff tears in 69 patients who were 65 years or older (mean, 75 years). Preoperative symptoms for longer than 34 months predicted poor outcome, with 100% sensitivity, 98% specificity, and 94% positive predictive value. Female gender and medical comorbidities (American Society of Anesthesiologists [ASA] grade higher than III) were also associated with poor outcomes. Women accounted for 23 of 24 patients whose cuff tissue was graded as poor intraoperatively, with subsequent inability to adequately repair the torn tendon to bone in 16 of these patients. There was no discussion of ASA severity in relation to patient gender, and age was not independently related to poor outcomes.
Corticosteroid injections are used by many surgeons as a component of nonoperative treatment in subacromial impingement. However, the risks of this treatment may eventually outweigh any potential benefits. Watson24 has demonstrated that increasing numbers of injections lead to softening of the cuff tissue, larger tears, and poorer results. In this study, however, it was the older patients who had received more injections, had larger tears, and demonstrated worse cuff tissue. These factors may represent the natural history of the disease as much as the impact from the number of injections received. The study concluded by recommending that a decision regarding repair should be made early, before patients received the critical number of four injections.
It is crucial to know whether patients have had previous surgery (or surgeries) on the affected shoulder. The results of revision rotator cuff repair decline when there is deltoid detachment, an aggressive prior acromionectomy, poor quality cuff tissue, enlargement of the tear, and/or retraction. Obtaining a copy of the operative report can provide abundant information to help plan the next step in treatment. Deep infection after rotator cuff repair occurs in up to 1.9% of patients,25 with Propionibacterium acnes as the most common pathogen. Infection with P. acnes can be an indolent, subclinical source of pain, and must be ruled out as a cause of failure. Other important factors to address in the history are the patient’s functional status, goals of treatment, and hand dominance. An older sedentary patient whose primary complaint is pain in their nondominant arm may not wish to undergo rotator cuff repair or other reconstructive procedure, even if he or she is a candidate for a more aggressive approach.