Massive Bone Loss about the Elbow
Bernard F. Morrey
Joaquin Sanchez-Sotelo
Because the elbow is a subcutaneous joint and vulnerable to trauma and infection and less so malignant conditions, massive loss of bone and soft tissue about the elbow is relatively common and constitutes a devastating problem (1). This probably represents the most challenging of all interventions about the elbow. The salvage treatment is either implant or nonimplant salvage (2,3,4,5).
INDICATIONS
Bone loss proximal to the olecranon fossa or distal to the coronoid
Motivated patient
CONTRAINDICATIONS
Active or acute sepsis
Prior sepsis with potential to be subacute (exclude with staged procedure)
Absence of neural function of the hand
Absence of potential to flex the elbow if reconstructed
Deficiency of soft tissue coverage, until adequately addressed, if possible
Inability of patient to cooperate
IMPLANT SALVAGE OPTIONS
The implant salvage option may be either a prosthetic or an allograft replacement. In fact, the most efficient way of managing massive bone loss at the elbow is an allograft prosthetic composite (APC). In recent years, we have refined our thought process and clinical experience and feel as though reliable APC options are now available even for the most devastating circumstances (5).
NONPROSTHETIC MANAGEMENT
The basic approach to nonprosthetic management is that of stabilizing the forearm referable to the humerus. This is often done in the acute setting using an external fixator with the intent to achieve a resection arthroplasty that may have some stability due to the scar tissue. This is usually indicated in instances of gross or refractory infection but the outcome is highly unpredictable and thus is truly the final salvage option (6).
RECONSTRUCTION OPTIONS
There are four forms of functional reconstruction: osteoarticular allograft, allograft augmentation, impaction grafting, and allograft prosthetic composite. We regularly employ two methods of reconstructing massive bone loss at the elbow: allograft augmentation, that is, the use of struts and APC. Impaction cancellous grafting is used when there is adequate circumferential albeit expanded, cortex available and is not discussed here (1,7).
Osteoarticular Allograft
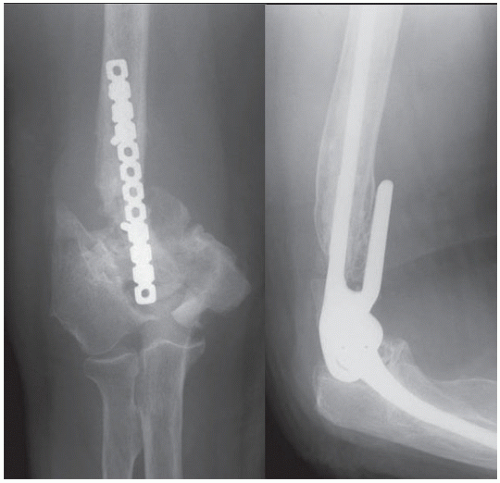
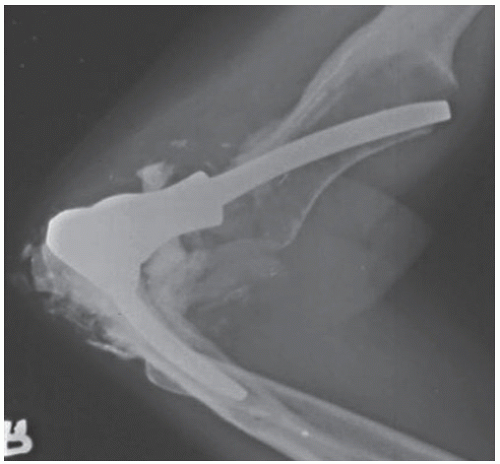
Osteoarticular allograft reconstruction of the elbow has not proven effective long-term due to the inevitable development of neuropathic degeneration (2) (Fig. 35.1).
Allograft Augmentation
INDICATIONS
When the loss of bone is relatively mild or not so great as to preclude secure fixation of the implant into host bone
To stabilize the flange of the prosthetic implant
At the ulna in order to reconstruct an absent olecranon and to improve the extension strength of the triceps mechanism
To bridge osseous defects that may have occurred at the time of implant revision
These have a very good rate of incorporation (8,9,10). Regardless, secure implant fixation into host bone is expected and required (Fig. 35.2).
INDICATIONS
The most common underlying problems are a septic or nonseptic failed implant or a posttraumatic situation.
Circumferential (loss of distal humerus, loss of proximal ulna, loss of both distal humerus and proximal ulna)
Inability to stabilize with strut or impaction grafting
Motivated patient
Extremity required for function
Significant pain
Gross instability
CONTRAINDICATIONS
Recent sepsis.
Nonfunctional hand.
Lack of motor power to flex the elbow.
Note: Loss of extension power can be compensated by gravity and is not an absolute contraindication.
Simpler solutions exist (i.e. direct recementation and use of struts) (Fig. 35.4).
STRUT RECONSTRUCTION
Technique
Patient positioning The patient is supine on the table. The arm is brought across the chest (Fig. 35.5A).
Incision
A posterior skin incision is employed in the majority of instances. As this is often a salvage procedure, prior incisions are followed.
Typically wide and thick subcutaneous tissue flaps are raised both medially and laterally but only to the extent needed for the reconstruction (Fig. 35.5B).
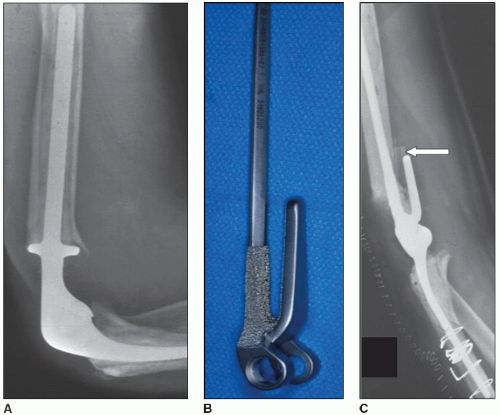 FIGURE 35.4 Failed custom device with loss of distal humeral bone (A). Easily reconstructed with recementation of a long flanged device with an anterior strut (arrow) (B,C). |
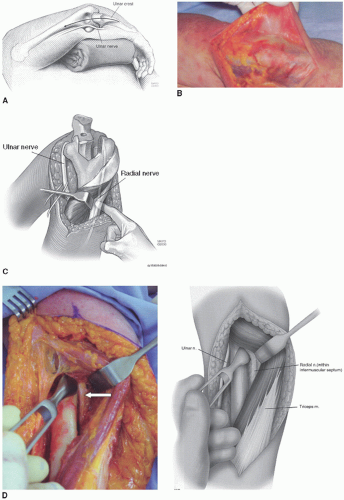 FIGURE 35.5 A:
Get Clinical Tree app for offline access
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree


|