Manipulation, Massage, and Traction
J. Michael Wieting
Michael T. Andary
Todd G. Holmes
Adam Cugalj
Neal Cross
Gregory Thompson
Manipulation, massage, and traction have been used in various forms for several thousand years throughout the world. Each includes treatments for the relief of painful conditions—sometimes with noticeable immediate effects—that are sought by an ever-increasing number of people; as an example, manual medicine procedures, including manipulation, are very much in demand by patients, of whom a reported 12 to 17 million Americans alone, who seek, receive (over 90 million manipulations alone) and are very satisfied with them on an annual basis (1,2). Despite consistent high demand for these treatments, evidence of the effectiveness of some of the techniques comprising them has been difficult to obtain and complete acceptance within the medical community has, to date, been mixed.
Some argue that patients who improve and report feeling better with these treatments may have done so anyway and that serious complications (which are rare and usually due to either an unqualified practitioner or the performance of an inappropriate maneuver) sometimes occur; that treatments are aimed at the pocketbook and not the pain; and that claims of success are sometimes unproven (3). The Agency for Health Care Policy Research (AHCPR) (4) recommendations that include manipulation, for example, as an option in acute low back pain management have done little to resolve these differences (5).
What has led to this apparently dichotomous thinking? One factor may be that some traction, manipulation, and massage techniques have an as yet uncertain mechanism of action. In addition, they are treatments that can be performed by nonphysicians. A treatment appears less scientific and perhaps less efficacious if it can be obtained from nonphysician, even nonlicensed, practitioners. A more acceptable rationale for rejecting these treatments may be the paucity of scientific proof of benefit.
The use of any treatment should be limited to those conditions that can reasonably be expected to improve with the physiologic effects of that treatment. The macroscopic effects of traction and massage have been partially elucidated and offer some degree of guidance regarding indications. This is not yet the case for manipulation, although evidence is growing. In the remainder of this chapter we will discuss what information is available regarding the use and efficacy of these treatments and attempt to provide the physiatrist with a basis for understanding their use and role in the treatment paradigm.
MANIPULATION
Introduction
Although manipulation has been widely practiced in almost all countries of the world since at least the time of Hippocrates (6), the subject often evokes strong emotional responses among health care professionals, particularly in the United States and Great Britain. Since the 1890s, when manipulation became a cornerstone of the therapeutic approach of the Osteopathic and Chiropractic Schools of Medicine, the subject has caused debate among practitioners.
Manual treatments are among the most common procedures utilized on a daily basis across the globe; they are performed by physicians, physical therapists, chiropractors, nurses, athletic trainers, naturopaths, massage therapists, lay practitioners, and others. Early references to manual medicine can be found in the writings of Hippocrates, as mentioned above, and in ancient Egyptian hieroglyphics and early Chinese medical literature (7). In the United States, the roots of manual medicine can be traced to Andrew Taylor Still, M.D., and his contemporary, Daniel David Palmer. The former started his American School of Osteopathy in Kirksville, Missouri, in 1892, the latter opened the first chiropractic college in Iowa in 1895 (8). Today, manipulative treatments continue to be developed and researched nationally and internationally by an ever-growing cadre of practitioners.
This section provides a brief review of manipulation, describes some of the forms of treatment, and discusses the use of manipulation and its prescription, with a focus on physiatry, and physiatric application of manual medicine. The techniques described will be neither osteopathic, nor chiropractic, per se, but rather a combination of terminology and treatments a physiatrist is most likely to encounter.
The purpose of this section is to introduce manipulation and discuss its applicability to physiatry and to present some general guidelines for appropriate prescription. The evidence base for these treatments will be referenced where applicable and available, but we will neither attempt to settle ongoing disputes concerning the efficacy of manipulation nor comprehensively cover all forms of manual treatment or diagnosis.
Definition
The definition of manipulation is controversial, but a consensus definition is that it is “the use of the hands in a patient’s management process using instructions and maneuvers to achieve
maximal painless movement of the musculoskeletal system and postural balance” (8). More specifically, spinal manipulation is a mechanical treatment applied to a specific vertebra or vertebral region, including the sacroiliac region and the rib cage, by a physician or therapist with the primary goal of restoration of lost vertebral motion. Nonthrust techniques (“mobilization” to a physical therapist) are encompassed by this narrower definition. Active exercise, self-applied forces, or self-induced motion, although occasionally effective in the restoration of vertebral mobility, are not included. Massage, which is applied only to soft tissue, and traction, which is nonspecific to a vertebral region, are excluded by this definition, although the reader will recognize that some overlap among manipulation, traction, and massage occurs. The interested reader will find a detailed history of manipulation in a number of sources (6,9,10).
maximal painless movement of the musculoskeletal system and postural balance” (8). More specifically, spinal manipulation is a mechanical treatment applied to a specific vertebra or vertebral region, including the sacroiliac region and the rib cage, by a physician or therapist with the primary goal of restoration of lost vertebral motion. Nonthrust techniques (“mobilization” to a physical therapist) are encompassed by this narrower definition. Active exercise, self-applied forces, or self-induced motion, although occasionally effective in the restoration of vertebral mobility, are not included. Massage, which is applied only to soft tissue, and traction, which is nonspecific to a vertebral region, are excluded by this definition, although the reader will recognize that some overlap among manipulation, traction, and massage occurs. The interested reader will find a detailed history of manipulation in a number of sources (6,9,10).
While the majority of manipulative treatments performed in the United States are aimed at the cervical and lumbosacral regions to treat musculoskeletal symptoms, manipulation can be performed on any part or region of the body. It is generally directed at restoration of normal motion and elimination of pain secondary to disturbed biomechanics. It is an application of forces to the muscles, tendons, ligaments, joints and capsules, bones and cartilage of the vertebral column, or other tissues, with a primary aim to restore the body to a state of homeostasis (11). Although often taught in a regimented way, the application of manual treatment should not be formulaic or protocol driven, but, rather, customized to the individual patient and based on a careful and thorough history and physical examination. Assessment involves the examination of the restriction of motion and the asymmetry of the joints in a given area of the body, as well as that in contiguous and adjoining regions. Generally, one tests for areas of tissue texture changes, pain in or sensitivity of the area, or a change in the quality of motion within a body region.
From a biomechanical perspective, an area of structural hypermobility or hypomobility, such as in adjacent vertebrae or other skeletal or muscular structures, is most often a consequence of a problem elsewhere in the body. When a certain degree of motion is expected in one area and it is deficient, another region then typically compensates for this with its usual motion, plus at least a few degrees more. If, for example, a stroke patient with hemiplegia presents with low back pain, one can treat the restrictions and dysfunction found in the lumbar spine and, if present, in the pelvis as well. These treatments may give the patient substantial relief of lumbar pain, but the pain and dysfunction will soon return if there is an overlooked causative restriction elsewhere. Consider, as an example, the patient’s lower limb weakness; the altered mechanics of the patient’s gait alone will affect both sides and compromise both pelvic and lumbar motion. Manipulation alone would be inappropriate as the neurologic deficit is not amenable to this form of treatment. Using manipulation to treat the dysfunction of the lumbar spine and other areas, in combination with physical therapy, assistive devices, and other appropriate physiatric care, may optimize this patient’s functional recovery and lessen the severity of the low back and pelvic symptoms.
The majority of the studies and review articles pertaining to manipulation have focused on the application of these treatments to the cervical and lumbar spine and on the use of thrusting techniques in particular. It is important to realize that there are many other types of manipulative techniques and which one is chosen should be based on a thorough examination of the patient and the musculoskeletal lesion to be treated. It is essential to find the cause of the illness or dysfunction if the most efficacious treatment or combination of treatments is to be chosen and applied.
Techniques of Manipulative Treatment
In the following introductions to the most common techniques of manipulation used in the United States, discussion is limited to those that the physiatrist is most likely to encounter early in the investigation of manipulative care.
The concept of direct and indirect treatment is ubiquitous in the literature regarding manipulative technique. As previously mentioned, an accurate and thorough examination and localization of musculoskeletal dysfunction are essential. Before initiating treatment, any restriction in range of motion, either gross or subtle, should be detected during passive motion testing. This restriction is commonly termed a barrier (this is fully explained below). Direct treatments engage the barrier and focus mechanical forces into the motion restriction to eliminate it. In contrast, indirect treatments avoid the barrier and instead focus treatment within the joint range that allows the most fluid motion in order to expand normal range by neuroreflexive means.
Thrust Techniques
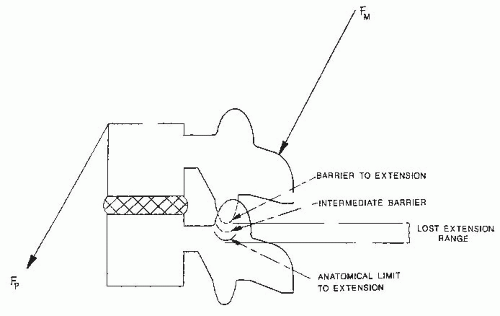
Other terms for thrust techniques (9,10) include impulse, which is of European origin (9), high velocity/low amplitude, adjustment, and spinal manipulative therapy (SMT), which are of chiropractic origin. In most approaches, the operator diagnoses the dysfunctional vertebral segment by identification of position or motion abnormalities or by related tissue changes, including tenderness to palpation or induced motion. He or she then rotates, side-bends, and flexes or extends the vertebral segments below it, thereby engaging or “locking” the facet joints so that further motion is limited to the vertebra in question. This vertebra is then passively moved to its limit of motion (i.e., its barrier) to remove all slack motion. A small force localized to the joint in question and in the direction of the restricted motion is applied to hold this position. Finally, a brief (9,10,12) controlled thrust is applied to the involved vertebra in the restricted direction, and a small motion, flexion, extension, rotation, or side bending, occurs as the vertebra traverses the barrier (Fig. 64-1). Often an audible “pop” or “click” is produced. The source of this sound has been attributed to cavitation (13) and nitrogen release in the synovial facet joint. Its presence infers that a mechanical process has occurred over a much shorter time than for inaudible events, such as reflex muscle contraction. This further suggests that audible thrusting procedures have a different mechanism of action and possibly different level of efficacy compared with
other manipulative procedures. It is arguable whether there is clinical relevance to this sound (9,10,11). All thrust techniques can potentially do harm if forces are not well localized and/or misdirected along axes which do not correspond to correction of the dysfunctional segment at the vertebra or vertebral region involved. Again, precision of localization and placing the joint or segment into its restrictive motion barrier so that the physician has maximal control of force applied and uses only the force sufficient to create or restore motion is desired to thereby complete the treatment (14). Ideally, one should use the minimal force over the shortest distance possible to achieve the desired results.
other manipulative procedures. It is arguable whether there is clinical relevance to this sound (9,10,11). All thrust techniques can potentially do harm if forces are not well localized and/or misdirected along axes which do not correspond to correction of the dysfunctional segment at the vertebra or vertebral region involved. Again, precision of localization and placing the joint or segment into its restrictive motion barrier so that the physician has maximal control of force applied and uses only the force sufficient to create or restore motion is desired to thereby complete the treatment (14). Ideally, one should use the minimal force over the shortest distance possible to achieve the desired results.
Articulatory Technique
The articulatory technique (9,10,15), also referred to as mobilization in Europe and low velocity/high amplitude in the United States, is very similar to oscillatory (16) techniques performed in Australia. The vertebral joint is passively moved within the reduced range defined by its resting position and the dysfunctional limit of motion. The extent of motion and its endpoint are varied, but ultimately the endpoint and dysfunctional barrier become the same, and the barrier is teased with repeated motion. Ideally, the quality or feel of the induced motion and the quantity of force and excursion are normalized by this procedure. Occasionally, a small amount of additional force takes the vertebra through its barrier or restriction, and this technique may then appear like a thrust. Other variables include frequency of repetition, duration of “hold time” at the extremes, and the rate, rhythm, and amplitude of oscillation (depending on underlying tissue texture) (16).
Positional Techniques
The underlying principle in counterstrain and functional technique is that hypomobility is caused by an inappropriately firing muscle, that is, active tissue, rather than a shortened passive tissue such as capsule, myofascial, or ligament. Thrust, articulation, and muscle energy techniques all employ forces that might be expected to lengthen shortened passive tissues, whereas the positional techniques attempt to change an inappropriate engram, or central pattern, of vertebral muscle behavior, similar to what is done in rehabilitation of head injury and tendon transplants.
Counterstrain
Counterstrain (9,16,17) is an indirect myofascial technique developed by Jones (18) that shares with functional technique (discussed later) the emphasis on relative positioning of a joint or body part as an essential component of the treatment. This technique involves placing the joint or body part into its position of maximal “ease” or comfort, relaxing myofascial or ligamentous soft tissues. This allows inappropriately shortened muscles to “reset” their spindles, which then are thought to normalize their proprioceptive input to the spinal cord. Generally, the restricting muscle is overly shortened by this positioning (counterstrain), and its antagonist muscle is gently overstretched (strained) in the process. The treatment position is found by palpatory pressure and minimizing the pain at an associated counterstrain “tender point” to less than 80% of its initial degree of tenderness (15,17,19). This position is then maintained and held for 90 seconds for vertebra and other points, except for ribs which are held for 120 seconds (19). On occasion, small “fine-tuning” passive repositioning movements with feedback from the patient may be needed. Because tenderness is a part of this feedback system, the patient must respond to the questions of the practitioner regarding their degree of pain or “tenderness” at the noted point(s). The patient is then slowly returned to the neutral position, usually in one plane of motion at a time, to prevent resumption of the inappropriate muscle firing. Structural reassessment is then repeated.
The tender points of counterstrain do not coincide with the trigger points of Travell (252) or the similarly named tender points associated with fibromyalgia. Those of
counterstrain are usually small, discrete, fibrotic areas thought to be manifestations of distant arthrodial or myofascial restriction (9); they are not paired but may be associated with the other features of fibromyalgia such as stiffness, fatigue, and sleep disorders. They are distributed throughout the body in reproducible locations depending on the nature and location of the associated biomechanical dysfunctions. They are similar to those found in fibromyalgia in that they cause local pain when palpated rather than in a distant referral pattern. Counterstrain is considered to be gentle, safe, effective, and atraumatic; because of this, it is considered to be useful in elderly and hospitalized patients, in children, and in patients with fear of pain. This technique is easy to perform and relatively forgiving. It is easily incorporated into a home exercise program as well.
counterstrain are usually small, discrete, fibrotic areas thought to be manifestations of distant arthrodial or myofascial restriction (9); they are not paired but may be associated with the other features of fibromyalgia such as stiffness, fatigue, and sleep disorders. They are distributed throughout the body in reproducible locations depending on the nature and location of the associated biomechanical dysfunctions. They are similar to those found in fibromyalgia in that they cause local pain when palpated rather than in a distant referral pattern. Counterstrain is considered to be gentle, safe, effective, and atraumatic; because of this, it is considered to be useful in elderly and hospitalized patients, in children, and in patients with fear of pain. This technique is easy to perform and relatively forgiving. It is easily incorporated into a home exercise program as well.
Functional Techniques
Functional techniques (9,12,20), developed in the 1940s and 1950s, share with counterstrain a methodology oriented to reducing inappropriate afferent impulses from nociceptors and mechanoreceptors (and the resultant efferent a motor activity to the skeletal muscle) by placing the joint or body part into a position of maximum ease (11). Unlike counterstrain, the position is found and monitored by the practitioner sensing increased tissue tension to small, induced motions. The patient provides “respiratory assistance” as he/she inhales and exhales to varying degrees to facilitate the release of the involved soft tissues.
Practitioners feel that passive positioning to maximum ease allows the firing pattern of the aberrant muscles to reset such that they are normalized in a neutral position. This approach, unlike counterstrain, does not make use of tender points and is, in principle, more objective because only the practitioner’s palpation determines the positions of balance. Functional techniques (nontraumatic and repeatable) are useful in both acute and chronic conditions.
Muscle Energy
This nonthrusting technique (9,10,21,22) is also called isometrics and, by some Europeans, like articulatory technique, mobilization. Similar to proprioceptive neuromuscular facilitation (PNF), it uses stretch reflexes and isometric contractions to relax the target muscle (23, 24, 25). The muscle energy technique requires the operator to position the patient into the motion restriction barrier and take up slack as in direct thrust techniques. Instead of an impulse against the restriction, however, the practitioner instructs the patient to exert a small isometric force away from the barrier. Simultaneously, the practitioner provides equal resistance, preventing active motion. The patient holds the isometric contraction 5 to 10 seconds. After the patient relaxes, the affected joint can passively move further beyond the original restriction to a new barrier. The contract-relax effort is often repeated several times, engaging successive barriers with sequentially improved motion.
Soft-Tissue Techniques
The soft-tissue approach uses mechanical stretch of the skin, muscle, and fascia to increase their motion. Lateral stretch (or “bow-stringing”), linear stretch, and deep inhibitory pressure are the most common procedures. This approach is useful in virtually all patients, often as a first step in treatment involving multiple manipulative approaches. Encouraging overall circulation and enhancing venous and lymphatic flow are central to these techniques (9). The overall purpose of soft-tissue technique is to relieve superficial muscle and fascial tension.
Myofascial Release
The myofascial release approach (9,26, 27, 28) to manipulation overlaps somewhat with massage and, conceivably, with traction. It can be directed at hypomobility of a vertebra, of a vertebral segment (as in spinal manipulation), or of the entire body, in which case it resembles some massage techniques. It can be indirect, whereby a restricted area is placed into a position of little resistance until relaxation occurs, or direct, in which case the affected area is placed against the restriction barrier with constant force until a fascial release occurs. Conceptually, in this approach, all the myofascia in the body are interconnected, and when one area is tight or restricted, diminished movement results locally and in more distant areas.
Practitioners continually palpate to assess tissue response and adjust the applied forces of stretch, traction, pressure, or twist they are using, until the affected tissues are felt to change, often called a “release.” The actual forces are combinations of those used in massage, soft tissue, muscle energy, and possibly craniosacral techniques. The mechanism of the release of the “tightness” can be biomechanical (such as viscoelastic strain) or neuroreflexive, but, when accomplished, fascial resistance to forces applied should be symmetric, and the tissues should be relatively mobile, that is, responsive to the force.
Joint Play
This concept addresses the immediate cause of the joint motion restriction. In an idealized joint, the bone moves in small precise ranges, independent of voluntary muscle contraction, over the stationary contours of opposing joint surfaces as motion in the voluntary direction occurs. But actual joints sometimes have noncongruent and sometimes diseased nonsmooth surfaces, resulting in movement in an additional perpendicular or tangential direction to the plane of motion; this motion is called joint play by manipulation practitioners and accessory motion (29) by many physical therapists. Joint play includes motions in a nonvoluntary direction as well. Thus, motion restriction in a direction perpendicular to that of voluntary motion will limit voluntary motion in the voluntary direction. This concept leads naturally to manipulation because the practitioner can “gap” (11) the restricted joint allowing a return to a symmetrical balanced seating of the joint, whereas voluntary or active motion cannot.
Craniosacral Manipulation
Craniosacral manipulative treatment (9,10,30,31) is an approach based on the concept of a primary respiratory mechanism, a cyclic, palpable, rhythmic wave of inherent motion, which corresponds to the Traube-Hering-Meyer wave (a rhythmic variation related to vasomotor tone), and is most easily appreciated in the cranial and sacral areas (32). It is not clear whether this wave is related to low-frequency waves noted in cerebrospinal fluid (CSF) monitoring (32). This primary mechanism is described to include the inherent mobility of the central nervous system (CNS), CSF fluctuation, the articular mobility of the cranial bones, involuntary motion between the ilia, of the sacrum, and the mobility of intercranial and interspinal membranes (30).
The practitioner palpates the head, sacrum, or anywhere on the body to feel pulsations of the postulated wave motion in the 8 to 12 per minute range and for symmetry, amplitude, regularity, and frequency of the wave. In infants and those with head injury, it is easy to accept the concept of motion, but in the normal adult, motion at the cranial sutures must be quite small, animal studies notwithstanding (33). Whether elastic distortions could give rise to these motions or to palpable changes in elastic compliance (34) is unclear. When abnormalities are found, the practitioner uses gentle pressure on the skull and sacral areas to restore the wave to its normal symmetry, rhythm, and amplitude.
At this time, this technique remains controversial, even among some practitioners of manipulation. However, its largest subset of potential patients, infants with birth defects and patients with head injury, intersects strongly with the patient base of many physiatrists, and its recent growth in popularity demands inclusion in any current discussion of manipulation. Importantly, there is some indication that in the head injury population, cranial manipulation can produce undesirable results (35).
Hypothesis of Mechanism of Action
Manipulation is essentially a mechanical intervention that alters either the mechanical behavior of passive soft tissues or the neural control of the active skeletal muscles that cross a vertebral joint. It is not surprising that almost all the various components of the conceptual framework of manipulative medicine have position or motion of the joint and the soft active and passive tissues that determine these positions or motions as their unifying core. But other than this essential portion, there is wide divergence among practitioners and researchers as to the nature of the dysfunctional problem, its etiology, and what the intervention does to treat it. It is helpful to recognize that various terms refer to the same entity; for instance, minor intervertebral derangement, osteopathic lesion, chiropractic subluxation, manipulable lesion, joint blockage, segmental dysfunction, and somatic dysfunction are all used to describe the same entity. Generally, some pathology, such as fractures, sprains, strains, tears, avulsions, tumors, and joint inflammation, may be excluded from the various hypotheses because it is generally recognized that manipulation would rarely be considered as primary therapy for those conditions. Fibrotic contractures, sprains, and strains may be exceptions because these may be amenable to manipulation, including, but not limited to, thrust (36).
There are several hypotheses aimed at explaining the cause of somatic dysfunction. Some of the more common of these will be briefly mentioned here, especially as they are more likely to be encountered in physiatric practice.
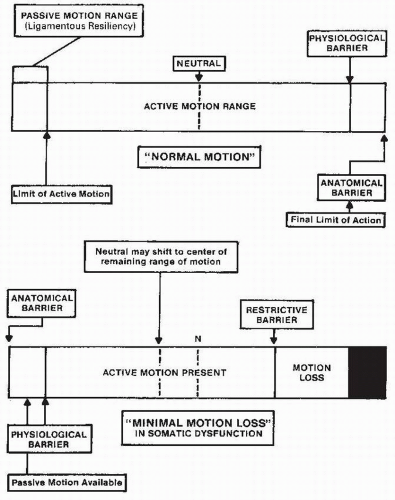
Barrier models have been described by several investigators to explain palpable findings (9,10,37,38) (Fig. 64-2). Normal joints possess an active range of motion and a larger passive range of motion. A barrier or motion restriction may result from abnormal muscle contraction, or capsular or ligamentous shortening across the vertebral segmental joints either in the direction of the intended motion or perpendicular to the joint surfaces that compress them. When a barrier forms between the neutral position and the usual limit, the patient cannot achieve normal range; the manipulator needs additional force to achieve the normal passive range. Asymmetry of the static force may lead to a new resting position for the vertebra, away from anatomic neutral. A variant of this approach considers strain of soft tissue as the basic pathologic condition (23); the resulting inflammation and edema then start a local vicious cycle resulting in pain and hypertonicity.
The facilitated segment model assumes that a vertebral body, chronically malpositioned by contracture or overly active muscle, floods the segmentally related area of the spinal cord with inappropriate nonfatiguing proprioceptive impulses. These in turn spill over and facilitate outgoing motor neurons and autonomics in the same vertebral segment of the cord (39). Thus, pathways are present for interaction between soma and viscera at related segments, and palpatory diagnosis of visceral disease and manipulative influence on the viscera are possible. This also allows abnormal segmental areas that were asymptomatic to develop symptoms from general illness, emotional stress, or distant disease. Physiatrists and other physicians familiar with reflex bladders and autonomic hyperreflexia will probably accept the concepts of somatovisceral reflexes and segmental spillover, but may find the magnitude and importance of these effects in the spine-intact human to be unclear (40,41). Manipulation is thought to release the proprioceptive input by bringing the vertebra to its normal, symmetric position.
Numerous hypotheses have been offered by the chiropractic profession to explain the relationships between altered structure and resultant pathologic conditions. These are adequately reviewed by Haldeman (40,42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53). The deleterious neurophysiologic effects that result from nerve compression caused by vertebra derangement have been conjectured to be a major cause of both somatic and visceral complaints. This viewpoint, prominent since the
earliest foundations of chiropractic, is perhaps the one most associated with chiropractic by other professionals. However, other concepts, including neurodystrophic effects, viscerosomatic reflexes, and a proprioceptive insult phenomenon similar to the segmental facilitation model discussed earlier, also appear.
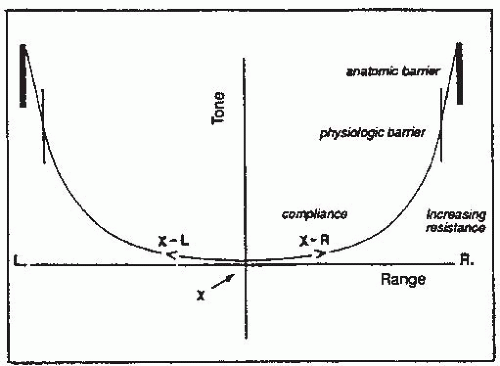
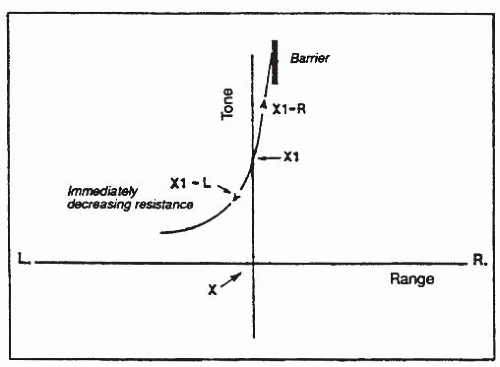
The concept of “ease and bind,” central to functional and other indirect techniques, uses a picture of vertebral motion around a symmetry point where motion in any direction encounters equal tissue resistance (Fig. 64-3). In a lesioned vertebra, the balance point is not the anatomic neutral, so that motion in one direction is met by more resistance (bind) than another (ease) (Fig. 64-4). The maintenance of the asymmetry arises in proprioceptive and γ motor spindle sensors, and treatment usually involves passive motion to and maintenance of the ease position so that the spindles can reset their output. The strain-counterstrain method suggests that the aberrant activity of the spindles can trigger reflex patterns and trigger points, which can be used to monitor the positional resetting of the spindle output (9,20).
The concept of tight-loose refers to the tightness of the fascia around a stimulated agonist muscle and the accommodating looseness of the fascia around the antagonist muscle. This is a central theme in myofascial release approaches to manipulation. The “release” phenomenon is the practitioner’s sense of relaxation of the tight fascia when treatment is successful (9,10).
Concepts of Manipulative Treatment
The possible therapeutic effects of manipulation include the following:
Passive stretch or even microtrauma (36) to the soft noncontractile tissues (ligament, capsule, tendon, fascia) whose contracture is limiting the vertebral range of motion.
Relaxation of inappropriately contracted skeletal muscle whose shortening has limited vertebral joint range of motion. This can happen as a result of changes in the afferent branch of a reflex, by resetting of the muscle spindle equilibrium point or by a change in afferent activity at the vertebral joint’s range endpoint (40,41).
Flooding of the cord with proprioceptive or kinesthetic signal to close the gate on pain (54)
Endorphin release, although, as noted previously, the data are contradictory on this possibility (43).
Placebo effect may be present in manual technique (43). The concept of the therapeutic benefit of human contact, or touch, should not be discounted when discussing any manual treatment.
It should be clear that manipulation success is reported for many, if not most, patients treated with widely varying techniques by practitioners working with very different assumptions as to the cause of the problem and the therapeutic action of the interventions. It would seem that any procedure that induces muscular relaxation or vertebral motion has some chance of success. Because most of the postulated actions of manipulation are accomplished by most techniques, success itself for each technique provides little feedback as to the validity of the various concepts. All, or possibly none, of the hypotheses presented may ultimately be found valid. The placebo effect, which may be diminished or enhanced when the manipulation is relegated to nonphysicians, is impossible to objectively gauge or compare among the various approaches.
Choosing Manipulation
Risks and Benefits
Few risks are involved in manipulative treatment. Complications resulting from isometric or articulatory treatment have not been reported. There are reports of complications of thrust manipulation to the cervical spine, but the number of reported problems, which is in the hundreds (55), is actually quite small when compared to complication rates of spinal surgery or the use of NSAIDs.
Most recently, cervical manipulation has received attention in the lay press in connection with the development of permanent neurologic sequelae, sometimes with strokelike symptoms (56). This serious and most often reported side effect seems to be related to thrusting style techniques applied to the cervical spine, especially when this region is placed in a position of extension, and without localization to a single vertebral segment at the time of the thrust. It is believed that this type of manipulation, with the cervical spine maximally extended, affects the vertebral artery by causing embolization of plaque material lining the artery. Some basic precautions, including neurological screening examination, with assessment of vertebral-basilar symptoms, and persistent monitoring of the patient during treatment, as well as careful patient selection, can minimize the risk of this rare, but serious, adverse effect.
Osteopathic and chiropractic proponents of manipulative treatment believe in distant visceral benefits, beyond the systemic benefits produced by good structural and biomechanical efficiency and relief of pain (8). However, distant visceral complications temporally related to manipulation have been documented only twice in the past 100 years (57,58); therefore, the physiatrist may safely evaluate the benefits or detriments of manipulation solely on musculoskeletal results.
Benefits of manipulation have been definitively proven to be as effective as NSAIDs and traditional care in the treatment of acute back pain and consensus is growing because it may offer relief in the treatment of acute and chronic low back pain (4,59). Proponents anecdotally report excellent results in treating acute musculoskeletal problems and good results in treating chronic conditions. Empirically, these outcomes are comparable with those achieved with “conventional” modalities, which also often carry no proof of efficacy. The growing number of patients obtaining manipulative treatment indicates at least some degree of perceived benefit.
Few studies have investigated the use of manual medicine in combination with other “standard” treatments, in part because of the potential difficulty separating the additional benefit of manipulation from its counterpart treatment. Most recently, studies have investigated the use of “standard” physical therapy and exercise with and without manual treatments for lumbar spinal stenosis and the use of osteopathic manipulative treatment with acupuncture to treat acute low back pain (60,61). Each of these studies, though small in size, and differing in methodology, found favorable results with combination treatment involving manipulation. Perhaps this is where future research effort, particularly in the physiatric application of manipulation, should be focused.
Applicability to a Physiatrist’s Practice
The physiatrist should be able to identify, through a focused history and physical examination, that subpopulation of patients most likely to benefit from the incorporation of manipulation into their treatment plan. Although some manipulative techniques may have hospital applicability, for example, rib mobilization in patients with either pulmonary disease or complications from surgery, most patients with conditions appropriate for manipulation are in the outpatient setting. This group includes people with structural problems such as pelvic asymmetries, and vertebral rotations, and others whose diagnosis may rely on palpatory expertise.
While there is a relative dearth of solid research on the use of manipulation, the bulk of what is available addresses what tend to be acute and chronic pain conditions, especially low back pain, treated in the outpatient setting. From these studies, the use of manipulation in acute conditions has been shown to be the most accepted indication (62). The use of manipulation for chronic spinal pain is not yet generally accepted (1,63). Studies (64) are difficult to perform because total eradication of chronic pain is rare, regardless of treatment method employed. Manipulative treatment in these cases should be directed at the restoration of normal spinal segmental motion, thereby reducing pain, with the hope that overall physical activity might increase (65). As with all treatments for chronic pain, whether there is demonstrable evidence of injury or not, the goal is to assist the patient to adapt, compensate, and continue to function well. An improved understanding of his or her condition can facilitate increased activity, social and vocational reintegration, and self-efficacy.
Objective evidence of the usefulness of manipulation for chronic pain is becoming more apparent. Randomized prospective clinical trials have shown improvement in pain complaints, increased paraspinal pain threshold levels, improved range of motion, and faster return to work (64,66, 67, 68). Patients with chronic back pain might be referred for a course of manipulation in conjunction with epidural injections, transcutaneous electrical nerve stimulation (TENS), psychological counseling, and other interventions.
In the inpatient setting, there is little published objective evidence for the use of manipulation. Much of what is written is anecdotal or case-study based. Historically, manual care was successfully used in the 1917 to 1918 influenza epidemic to assist respiratory function and resulted in significantly improved survival rates in persons treated with manipulation (69). Other small studies have been done with hospitalized pneumonia patients and other groups. Extrapolating from these data, it would seem that treating the thoracic region, rib cage, and diaphragm of severely deconditioned or bedconfined persons or those with spinal cord dysfunction might be beneficial and improve tolerance of routine activity or prescribed therapy. Patients with impaired mobility or who have undergone total joint replacement or other surgical procedure, especially if they have concurrent fluid accumulation in the limbs, might benefit from gentle manipulative techniques to assist in fluid mobilization until the patients own mobility could do so. Myofascial release techniques could assist in the recovery from trauma-induced issues. Perhaps persons with traumatic brain injury or children with developmental delay could benefit from craniosacral manipulation. Of course, all of these potential treatments come with the advice of careful patient, provider, and technique selection and to follow the “golden rule” of medicine: “First do no harm.”
Patient Selection
A general physiatric examination should be performed on every new patient. Any underlying impairment must be identified and treated, including fractures, disc herniations with neurologic signs and symptoms, and major sprains, strains, tears, hematomas, and joint injuries. A thorough physical examination, including assessment of gait, posture, muscle tone, muscle stretch reflexes, manual muscle testing, coordination, mental status, and cranial nerves, is strongly recommended prior to initiation of, or referral for, manipulation. Considerations for imaging or electromyography would be no different for the physician using forms of manipulative treatment than for any other type of intervention. There are specific contraindications for thrusting and articulatory manipulation that must be considered, which are discussed below.
Next, the physiatrist contemplating manipulative intervention performs a focused, detailed structural examination in areas suggested by symptoms or by the general examination, with the goal of finding treatable “manipulable lesions.” This evaluation involves careful observation and palpation as well as active and passive motion examination. Subsequent success with manipulation will depend on an accurate diagnosis of lost motion. The findings of palpation and segmental autonomic changes constitute the most important components of structural diagnosis.
The factors generally sought on vertebral or segmental levels are summarized in Table 64-1 (9,70). Passive vertebral motion is evaluated for range, symmetry, quality of motion, and force needed to achieve full range (10,71). Additionally, assessing forward, backward, or side bending and rotation of the vertebra (72) and tenderness elicited by local pressure on the interspinous ligament (70) are useful clues to dysfunctional conditions and loss of joint play. Subcutaneous tissue texture changes (e.g., edema, fibrosis) (72) noted by palpation and skin rolling (10) are signs of dysfunction, and some practitioners look carefully for segmental autonomic changes such as perspiration (10) and hyperemic response to light pressure. The ribs, occiput, and pelvis often need to be included in this part of the examination. Vertebrae identified by positive findings in this type of examination are considered dysfunctional and, if hypomobile, are candidates for manipulation unless contraindications exist.
Hypermobile vertebral segments are themselves not amenable to manipulative treatment (11) but as they may signal the presence of hypomobile segments elsewhere in the spine, should prompt a search for reduced motion elsewhere. If hypomobile segments are found, successful manipulation could conceivably resolve a distant hypermobility. This interconnectedness of the vertebrae is one of the features that make dysfunctions of the spine difficult yet fascinating to study.
A structural examination of this type may add 5 to 10 minutes to an initial visit and less than 5 minutes to subsequent examinations. The physiatrist choosing to manipulate will of course need to do this evaluation with a relatively high degree of acumen and skill. Physiatrists referring a patient to another physician or a therapist for manipulation can probably stop with identification of a hypomobile or tender segment and leave some of the detailed motion analysis to the practitioner providing the manipulation. However, sufficient examination must be accomplished to identify the vertebral segment needing attention and to establish an endpoint of therapy that the physiatrist can verify.
TABLE 64.1 Vertebral and Segmental Findings on Palpation | ||||
|---|---|---|---|---|
|
Modes of Practice
Availability of manipulative treatment depends on which mode of practice is chosen. Physiatrists who wish to use manipulation but not practice it themselves have two alternatives.
Referral to a Physician
The referral of the patient for concurrent manipulative care to another practitioner works well in many instances (38), but potential problems may occur, such as oversight of the patients care. This impediment may be addressed through a specific referral that states the exact nature and the scope of treatment requested, that encourages discussion with the referring physician, and that makes clear the intent of the physiatrist to resume the remainder of care, if that is the case. In addition, some physiatrists may be unable to assess the manipulators competence, and some patients may resent a referral to another practitioner.
Referral to a Licensed Nonphysician
The second option is for the physiatrist to diagnose the problem and write a prescription for manipulation to be performed by a licensed nonphysician, typically a physical therapist (6). This becomes a viable option as more nonphysicians acquire training in manipulation. In the United States, physical therapists traditionally have been limited to providing isometric and articulatory techniques, although counterstrain and myofascial release techniques are becoming more popular. Manipulation can be provided as part of a comprehensive physical therapy program. Even with such a referral pattern, however, the physician should at least acquire basic palpatory diagnostic skills, which then allows one to write a detailed prescription for an anatomic area to be treated and motion to be restored, along with a suggested technique to be used and frequency and length of treatment. The physician can then monitor progress of the treatment objectively and determine the endpoint and possible side effects or failure of the manipulation. Sequential monitoring of each manipulative intervention can be left to the therapist, given the safety of isometric and articulatory techniques. The acquisition of minimal diagnostic palpatory skills may take 1 to 2 weeks. However, the physiatrist probably will use these skills frequently and maintain them easily. The time commitment and economic investment are far less for this option than in the provision of manipulative treatment itself.
Realistically, many physiatrists allow the practitioner to choose areas of treatment and techniques. This is effective in most cases but can lead to loss of physician direction. Caution must be used to avoid unnecessary continuation of treatment when pain relief does not correlate with biomechanical improvement. If the patient has little to no perceived benefit following four to six appropriate manipulative treatments, the patient should be reassessed by the physiatrist. If the biomechanical deficit persists, additional regions of the patients body should be reevaluated for their possible contributions to the somatic dysfunction. If the structural lesion is improving, based on the evaluation of the prescribing physician, but the patient does not feel the treatments have been helpful,
additional sessions of manipulation should be approached with caution. Consideration of another type of treatment, or a different provider, should be entertained.
additional sessions of manipulation should be approached with caution. Consideration of another type of treatment, or a different provider, should be entertained.
Most physicians employing manipulation believe that restoration of the vertebral joint’s normal passive and active ranges of motion and resting equilibrium position is the endpoint of treatment (10). In this view, spinal manipulation is analogous to peripheral passive range of motion and end stretching. It is a natural extension of the physical therapy that physiatrists already prescribe for spine problems because it simply addresses individual joints rather than the spine as a whole.
Acquiring Manipulation Skills
There are three obstacles to the physiatrist performing manipulation:
Acquiring initial skills
Maintenance of skills
Economics of manipulation
Thrusting types of manipulation, because of the significant forces involved and potential for harm, are best learned on volunteers, not patients, under the close direction of a skilled practitioner. Estimates of the minimum initial learning time required vary from 6 to 8 weeks (7). Even the lower estimates place this type of training out of the reach of many physiatrists. Because of their inherent safety, isometric (muscle energy) and articulatory techniques sufficient for therapy initiation can be acquired by most in 1 to 2 weeks of formal course work. This is so because even an inappropriate isometric technique rarely causes detrimental effects. Thus, the physiatrist may begin working with patients early in training and develop improved techniques with time.
Postdoctoral programs such as those approved by the American Academy of Physical Medicine and Rehabilitation, the American Osteopathic Association, Colleges of Osteopathic Medicine, the American Manual Medicine Association, and other sources can provide a mechanism for the physiatrist to become acquainted with the skills necessary to begin manipulation. There are numerous other courses available that may also be of use to the physiatrist but would have to be investigated individually. There is growing interest among physiatric residents in acquiring this type of training (73), which has led to expanded training opportunities.
The actual minimum frequency of use needed to maintain competence or excellence varies considerably from one person to another. Clearly, however, the potential user should consider maintenance of skills before investing time and money in the acquisition of these skills.
Although any physician can study manipulation techniques, acquiring manipulation skill is demanding, requires practice, and not all physicians will derive satisfaction from providing it. Anecdotally, at least, manipulators who do not enjoy performing manipulation may not do it well.
Indications for Manipulative Treatment
Manipulative treatment, if there are no contraindications, is applicable in all musculoskeletal pain problems of the back, pelvis, neck, and limbs in which loss of motion or localized pain on induced motion may be a contributing factor. Some recent injuries (fractures, tears, sprains, strains, disc herniations with neurologic signs, tumors, anomalies, joint disease, inflammation, stenosis) will not respond to manipulation because of the resultant hypermobility, or because local conditions constitute contraindications. Again, all visceral or systemic pathologic conditions, which could manifest through viscerosomatic reflexes must be excluded or at least be under concurrent care.
Although mechanical back and neck pain is the most common indication, other musculoskeletal conditions responding to manipulative treatment have been described. Carpal tunnel syndrome and thoracic outlet syndrome have been shown to improve with myofascial stretch techniques (74, 75, 76). Techniques to optimize thoracic cage, clavicular, and scapular motion have benefit in many shoulder girdle problems (10,11). Common sports and repetitive use injuries can be treated with manipulation in conjunction with exercise to restore proper biomechanics (9,77).
Adverse Effects
Spinal manipulative treatment has a number of reported side effects (78,79). Perhaps the most common is a transient increase in discomfort for 6 to 72 hours after treatment (70). This should resolve to a level less than that of the pretreatment pain and should be less of a problem with each successive treatment. Minor autonomic effects, such as increased perspiration and early or increased menses, have been reported.
Duration and Frequency of Treatment
Appropriately applied treatment with the correct diagnosis generally produces objective improvement in 2 to 4 weeks (16). Lack of improvement in range of motion or function after 2 to 4 weeks would suggest the need to reevaluate the diagnosis or therapeutic plan. Duration of treatment is determined on an individual basis.
The optimal frequency of manipulative treatment is somewhat difficult to discuss. A search of the literature for a study to answer this question produced no results. Similarly, a review of several major textbooks on manipulation also failed to provide guidelines for treatment frequency. From experience, different practitioners of manipulation have their own preferences regarding style and frequency of treatment. The authors of this chapter feel that duration and frequency of treatment should be based on the condition being treated and the type of manipulation being used. There are undocumented, anecdotal reports of the development of hyperlaxity of ligaments resulting from the use of high velocity low amplitude (thrusting) techniques. The exact frequency and duration required to produce this undesirable effect is not clear. Soft-tissue techniques and indirect treatments, such as counterstrain, and other positional approaches, should allow the patient’s body adequate time to respond to each treatment before the same area is treated again, thereby preventing development of proposed reactive hyperlaxity of ligaments that is postulated with
more direct techniques. Another consideration to remember for areas of somatic dysfunction which seem to require frequent treatment to maintain the correction is to expand the physical examination to look for other areas of dysfunction which may be contributing to or causing the lesion in question, and appropriately treat this area first. This will no doubt be the topic for future studies on the use and application of manipulation.
more direct techniques. Another consideration to remember for areas of somatic dysfunction which seem to require frequent treatment to maintain the correction is to expand the physical examination to look for other areas of dysfunction which may be contributing to or causing the lesion in question, and appropriately treat this area first. This will no doubt be the topic for future studies on the use and application of manipulation.
Contraindications
Manipulative techniques differ as to their degree of invasiveness. Because of the higher forces involved, thrust is considered the most invasive, whereas articulation, isometrics, and functional approaches are considered less invasive. The more invasive the approach, the more likely it is to be contraindicated. The literature concerning contraindications for thrusting techniques has been reviewed comprehensively by Kleynhans and others (1,7,80,81); contraindications to articulation are discussed by several investigators (16,82, 83, 84).
Absolute contraindications for manipulation, especially nonthrusting techniques, are rare, and relative contraindications are few in number. Clearly, manipulation should only be performed for a hypomobile vertebral segment that might respond to manipulation; therefore, accurate diagnosis is important. Inadequate skill of the practitioner is a major contraindication for all types of manipulation.
Contraindications are summarized in Table 64-2.
Patients with concurrent cognitive or affective disorders may be poor candidates for thrusting interventions (84).
In addition, some investigators consider the absence of any pain-free direction of vertebral motion a contraindication to thrust. Pregnancy with known threat of miscarriage is an absolute contraindication to manipulation. Back pain and intervention in the normal low-risk pregnancy are discussed by Mantle (85). Because the disturbed biomechanics and hormonal ligamentous interactions of pregnancy are frequently implicated in back pain in pregnancy, this subject continues to stimulate discussion in the literature (86, 87, 88, 89, 90).
TABLE 64.2 Contraindications for Manipulation | ||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Objective radicular signs are a contraindication to articulation or thrust. The question of manipulation for clearly defined root pain without objective neurological findings is controversial, but most authors appear to avoid forceful techniques in favor of positional interventions (2,38,91, 92, 93). Isometrics in a nonlateral position appear to be safe, but there is no conclusive literature on this or any other contraindication to isometrics. Vertebral isometric techniques should not be used if the lesion would preclude passive range of motion, gentle stretching, or isometrics in a peripheral joint with the same condition. Catastrophic results do not occur in isometric techniques; some of the absolute contraindications to thrust and articulation, specifically osteoporosis, central cervical intervertebral disc herniation, rheumatoid disease distant from the cervical area, degenerative joint disease, and joint laxity may become relative contraindications, and patients with these problems probably can be cautiously treated with isometrics. Concurrent active myositis may contraindicate isometrics because of the patient’s active muscular contraction; however, for functional and counterstrain techniques, no contraindications have been documented, but it would seem reasonable to assume these may parallel restrictions against massage, discussed later in the chapter.
Complications
Clearly, complications may occur as a result of procedures that are done despite contraindications. However, the subject needs elucidation beyond that simple statement, best accomplished by discussing cervical procedures and thoracolumbar-sacral procedures separately.
Cervical Manipulation Complications