Managing Bone Loss with Metal Augments
Henry D. Clarke
Arlen D. Hanssen
INDICATIONS
Primary total knee arthroplasty (TKA) has proven reliable, yet failures do occur (1,2). Contemporary causes of failure include aseptic loosening, infection, and osteolysis caused by particulate wear debris (3,4). Each of these etiologies can result in significant bone loss that must be managed at the time of revision TKA.
The management of this bone loss in revision TKA is based on the size and type of defects that are encountered during the procedure. Numerous options exist and in many circumstances, alternative reconstructive techniques may be considered, including:
Cement
Particulate and structural bone grafts
Metal augments
Allograft prosthetic composites
Segmental replacement prostheses
The strategy used by each surgeon may be influenced by factors including availability of the required items, surgeon experience, operative time, cost, and age and activity level of the patient. As for many surgeons, our preferred choice primarily depends on the size of the defect.
Numerous classification systems have been previously described to aid in both pre-operative planning and intraoperative management of bone loss in revision TKA. We favor the use of the Anderson Orthopaedic Research Institute (AORI) classification, which is relatively simple and has been validated (Table 19-1) (5,6).
Practical guidelines have been published, based on the AORI classification, to aid the surgeon in managing the bone loss encountered in revision TKA (5,7). With the introduction of larger standard and trabecular metal augments, the spectrum of defects that can be managed with this technique has increased and represents our primary choice in most circumstances. Based on the size of the lesion, our preferred techniques are as follows:
AORI type 1 defects of the femur and tibia, including small, contained defects less than or equal to 5 mm in depth can be managed with cement or traditional metal augments.
AORI type 2 defects, whether unicondylar or bicondylar, including uncontained defects up to 20 mm in depth can usually be addressed with conventional metal or trabecular-metal augments.
AORI type 3 defects have historically been managed with structural allograft bone, allograft prosthetic composites, or megaprostheses. However, the introduction of very large trabecular metal augments, which can be used with a variety of prosthesis systems, has largely replaced our use of structural allografts.
TABLE 19-1. AORI Classification of Bone Defects in Total Knee Arthroplasty | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||
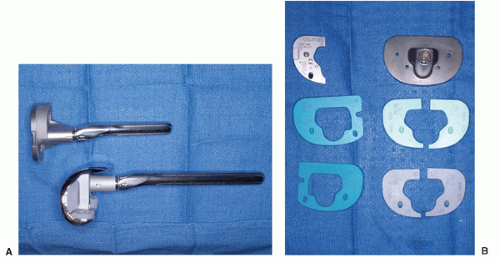
Standard metal augments are augments that regardless of size, attach directly to the body of the prosthesis with cement, snap, taper fit, or screw fixation. They may be composed of titanium, cobalt chrome, or tantalum. These augments are system specific and are available in a variety of sizes and styles. Femoral augments, typically blocks 5- to 20-mm thick, attach to the distal or posterior condyles of the prosthesis (Fig. 19-1A). Tibial augments include blocks and partial or full wedges that attach to undersurface of the tibial tray (Fig.19-1A,B). These tibial augments also replace up to 15 to 20 mm of bone loss. In addition, sleeve augments are available in some systems for the tibia and femur. These sleeve augments insert over the stem of a revision component and are designed to fill metaphyseal defects.
Very large trabecular metal cone augments do not attach to the prosthesis but instead are impacted directly into large areas of femoral or tibial metaphyseal bone loss (Fig. 19-2). These trabecular metal cone augments allow the restoration of a stable foundation upon which the prosthesis with or without additional standard augments can be supported. This ability to use these augments independently of the prosthesis as a structural bone graft substitute differentiates trabecular metal cone augments from other porous-coated metaphyseal filling metal augments. Currently
available trabecular metal cone augments are all manufactured by a single company (Zimmer, Warsaw, IN) from commercially pure tantalum. This material is formed into a porous trabecular geometry that approximates the structure of cancellous bone (8,9). Trabecular metal has two to three times the porosity of conventional porous metal coatings, which helps maximize the potential for bone ingrowth (8,9). In addition, because of its inherent strength, it may be used without the need for conventional metal backing to create structural augments. Widespread use in many areas of orthopedic reconstruction has shown the rapid manner in which osseous ingrowth into this tantalum substrate occurs (8). Potential advantages of the trabecular metal cone augments versus structural bone graft include:
available trabecular metal cone augments are all manufactured by a single company (Zimmer, Warsaw, IN) from commercially pure tantalum. This material is formed into a porous trabecular geometry that approximates the structure of cancellous bone (8,9). Trabecular metal has two to three times the porosity of conventional porous metal coatings, which helps maximize the potential for bone ingrowth (8,9). In addition, because of its inherent strength, it may be used without the need for conventional metal backing to create structural augments. Widespread use in many areas of orthopedic reconstruction has shown the rapid manner in which osseous ingrowth into this tantalum substrate occurs (8). Potential advantages of the trabecular metal cone augments versus structural bone graft include:
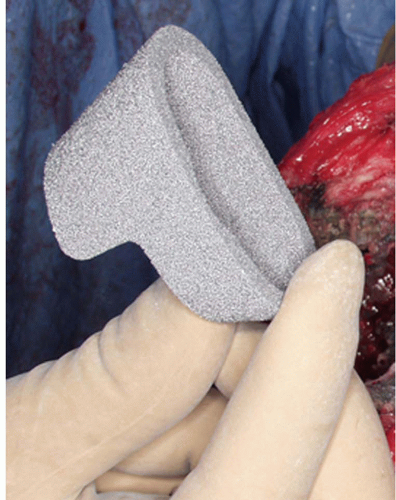 FIGURE 19-2 Trabecular metal cone augments are used independently of the prosthesis to reconstruct metaphyseal bone loss in the tibia or femur. A stepped tibial cone is shown before implantation. |
Availability of a wide variety of prefabricated shapes and sizes of augments
Quick and easy use
Ability to contour to obtain a custom fit
Immediate load bearing
Rapid bone ingrowth with stable long-term fixation
In distinction, although structural grafts and impaction grafting techniques have been reported to have acceptable results in complex revision hip and knee arthroplasty cases, reservations persist (10, 11, 12, 13). Potential problems with large bone grafts include:
Limited availability
Risk of bacterial and viral disease transmission
Increased intraoperative time
Prolonged weight-bearing restrictions until graft incorporation has occurred
As a result of these ongoing concerns with the use of structural bone grafts, coupled with the increasing availability of the large cone augments and good early results in the revision TKA setting, we have increased our use of trabecular metal cones in AORI type 2 and 3 bone defects, where we would have previously used bone graft material.
CONTRAINDICATIONS
Absolute contraindications for the use of standard and very large trabecular metal cone augments include typical contraindications for TKA, such as infection. Relative contraindications for the use of all metal augments regardless of size and composition include absence of host bone support. In cases in which massive bicondylar bone loss exists with absence of any rim of cortical bone, allograft prosthetic composites or segmental replacement prostheses should be considered.
PREOPERATIVE PREPARATION
Accurate preoperative assessment and classification of bone loss is important to ensure that appropriate augments or bone graft material are available. Because of the potential for iatrogenic bone loss during component removal, however, the final classification of the bone defects must be based on the intraoperative findings after prosthesis removal and debridement. Therefore, in revision TKA, the surgeon must be prepared for several contingencies.
Although not definitive, preoperative studies can provide helpful information about the type of defects that may be encountered intraoperatively.
Knee radiographs are low cost but may fail to allow accurate assessment of the number and size of lesions, especially in the setting of osteolysis (14
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree