Fig. 49.1
Patellar dislocation can occur when the femur rotates internally and the tibia externally with the foot fixed on the ground
Table 49.1
Predisposing factors
Trochlear dysplasia |
Patella alta |
Increased femoral antetorsion |
Increased tibial torsion |
Lateral patellar tilt |
Vastus medialis muscle hypoplasia |
Subtalar joint pronation-valgus alignment of the lower limb |
Ligamentous laxity |
Tall height |
Excess weight |
49.2 Injury Mechanism
A complex interaction between muscles, ligaments, bone morphology, and lower extremity alignment influences patellar motion. The most important stabilizer of the patella beyond 30° of knee flexion is bony stability of the femoral trochlea. Additional stability is provided by active and passive restraint. Actively, the rectus femoris and vastus intermedius muscles act along the femoral axis, and the vastus lateralis and medialis help stabilize the patella in the medial/lateral plane. Passive restraints include patellar tendon, the medial menisco-patellar ligament, and the medial patellofemoral ligament (MPFL), a thin but relatively consistent ligament [4, 5]. The MPFL extends from the medial margin of the patella and attaches to the femur between the adductor tubercle and the medial epicondyle [6, 7]. The MPFL is important in initiating smooth entry into the trochlea with knee flexion and seems to be the major ligamentous restraint against patellar dislocation [8]. Traumatic primary patellar dislocation is almost always associated with hemarthrosis, MPFL injury, and medial retinacular disruption [3]. Clinically, 94–100 % of patients suffer from MPFL rupture after acute patellar dislocation [8].
49.3 Clinical and Diagnostic Examination
The initial evaluation of a first-time patellar dislocation should include an appropriate patient history, family history of patellar dislocation or hyperlaxity, and physical examination. Patients frequently report that their knee “gave way” and that they “felt a pop.” Clinical findings include large effusion with tenderness about the medial retinaculum and hemarthrosis. The patella is usually spontaneously reduced, making the diagnosis less clear if the athlete cannot clearly identify what happened during injury. The clinician can rarely assist the reduction by applying a medially directed force with knee extension to push the patella over the lateral trochlea and back into the trochlear groove. If the patella does not easily reduce, the procedure should be aborted. A fracture fragment of the patella or condyle may limit the reduction and can be verified with radiographic studies [9].
Aspiration of the knee joint should be performed in patients with moderate to severe effusions. The presence of a hemarthrosis raises the likelihood that a significant osteochondral fracture has occurred. Clinical findings are not specific, so careful examination should be undertaken for anterior cruciate ligament, posterior cruciate ligament, and collateral and rotational laxity. Patellar apprehension and mobility should be assessed by medial and lateral patellar translation. A common physical examination sign to asses patella laxity is measuring the movement of the patella when passively stressed, recording the movement in quadrants of mobility as well as its endpoint firmness [10]. Increased lateral patella translation is suggestive of a lateral patellar dislocation.
Plain radiographs are always needed to evaluate patellar position and to asses osteochondral fractures, in particular, an AP-extended knee weight-bearing view, a Mercer-Merchant view (45° flexion weight-bearing view), and a 30° flexion lateral view. Both patellae should be included in the axial view. Even when the radiographs are normal, an osteochondral fracture may have occurred. Osteochondral fracture has been reported to be missed in 30–40 % of initial radiographs in both surgical and MRI studies [11, 12]. MRI is recommended to be performed quite soon after the injury to verify the diagnosis, evaluate additional injuries, asses the cartilage more precisely, classify the MPFL injury, and describe the anatomic factors of the patellofemoral joint (Fig. 49.2). MPFL injuries have been classified into three categories based on location: at the level of the MPFL patellar insertion, at the midsubstance, and at the femoral origin of the MPFL [13, 14]. Between 40 and 90 % of MPFL disruptions are located in the femoral attachment, whereas some studies have reported figures up to 50–60 % at the patellar insertion. The MPFL midsubstance region seems to be less frequently affected [15]. Recently, Sillanpää proposed a new classification for patellar insertion MPFL injuries: type P0 with ligamentous disruption, type P1 with bony avulsion fragment, and type P2 with bony avulsion involving articular cartilage surface from the medial facet of the patella [15].
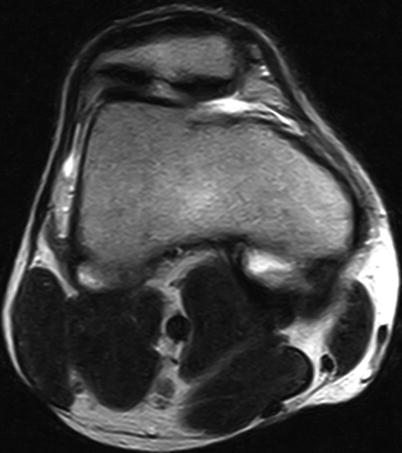
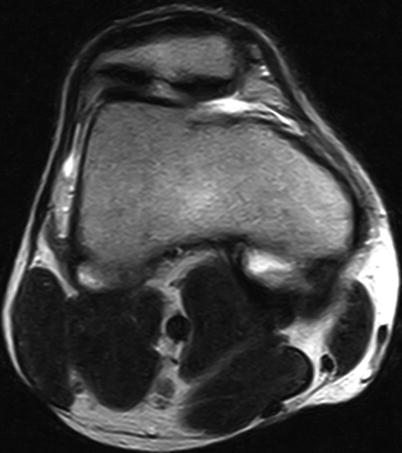
Fig. 49.2
Right knee MRI performed after first-time patellar dislocation. It can be noted a patellar osteochondral fracture at the MPFL insertion
49.4 Treatment Strategy
The initial management of a first-time traumatic patellar dislocation is controversial with no evidence-based consensus to guide decision-making. Conservative treatment has been historically suggested for patients with primary patellar dislocation. A short immobilization period is used for patient comfort and is followed by formal physiotherapy. Therefore, the optimal conservative management has yet to be established [16]. The surgical treatment should be considered in specific conditions. These include the finding of an osteochondral fracture, a substantial disruption of the MPFL, and a laterally subluxated patella with normal alignment of the contralateral knee [17].
49.4.1 Nonoperative Treatment
Hemarthrosis can be aspirated for pain relief. It is important to prescribe rest, ice, compression, elevation, and NSAIDs. The drainage massage of the knee may be useful in order to reduce the post-traumatic edema. Common at this stage is the use of physical therapy for the resolution of edema and pain. The patient should be immobilized initially for comfort (3–4 weeks) to allow immediate weight bearing as tolerated on crutches with early mobilization. Immobilization in extension may allow for a better environment for MPFL healing, but this comes at the expense of stiffness, weakness, and loss of limb and proximal control [18]. The aims of physiotherapy are to restore knee range of motion and to strengthen the quadriceps muscles to restore the dynamic part of the patellar soft-tissue stabilizers. At 4–6 weeks, walking and knee range of motion should be normalized.
49.4.2 Surgical Options
Studies that observed a patellar dislocation recurrence rate of up to 44 %, findings of slow-developing symptoms with previous pain in the frontal region of the knee, and recurring instability rate above 50 % after nonoperative treatment led to an increase in initial treatment with surgical repair and reconstruction of the medial patellar stabilizers [19]. In literature, there is no sufficient evidence to confirm a significant difference in the outcome between surgical or nonsurgical initial management after first patellar dislocation [20]. Surgical intervention should be considered in specific conditions. These include the finding of an osteochondral fracture or major chondral injury, a substantial disruption of the MPFL-VMO-adductor mechanism, a laterally subluxated patella on the plain Mercer-Merchant view with normal alignment of the contralateral knee, a patient fails to improve with nonoperative management especially in the presence of predisposing factors to patellar dislocation, and subsequent redislocation [17].
There is a very high prevalence of MPFL lesion after first-time patellar dislocation. Clinically, up to 94–100 % of patients suffer from MPFL rupture [8]. As described earlier, MRI is suggested to classify MPFL injury. In literature, there are many methods described for the acute surgical repair, but no one seems to show better long-term outcomes compared to conservative treatment [21–25]. Camano et al. suggest that MPFL patellar or femoral attachment injury can be surgically reinserted with sutures or suture anchors with satisfying results and may lead to a better outcome than nonsurgical treatment [22]. In different prospective studies is yet described that operative treatment does not improve medium-term outcome [23–25]. Midsubstance MPFL injury should be repaired only in rare cases with extensive VMO fascial disruption in a high-energy dislocation when the VMO detaches from the medial patellar capsule, and the quadriceps pull vector may be significantly lateralized; therefore, the patella dislocates in extension when the quadriceps is activated [16].
Surgical open repair and fixation is recommended when the osteochondral fracture is greater than 10 % of the patella articular surface or part of the weight-bearing portion of the lateral condyle [26]. Fixation is performed with pins, screw sutures, or bioabsorbable nails. If the osteochondral fragment is smaller than 5 × 10 mm, especially when located in a low-pressure area, surgery treatment is not recommended. Small fracture that acts as a loose body and produces symptoms should be arthroscopically removed [27].
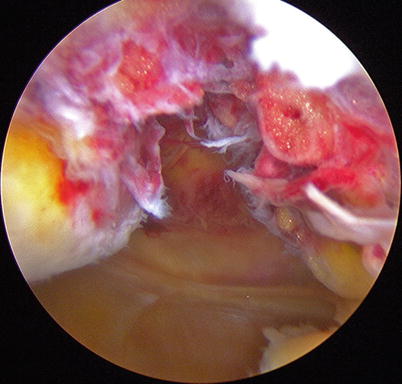
Mariani et al. described an arthroscopic technique for acute repair of patellar MPFL through reattachment at the patellar border with two trans-patellar sutures (Fig. 49.3). The potential benefit of performing an arthroscopic repair at medial hedge of the patella is to directly restore the MPFL to its anatomic position without associated surgical complications and to achieve a good tension of the ligament itself. In this prospective study, only one out of 17 patients treated with arthroscopic reinsertion of the MPFL reported one episode of patellar instability; 14 patients were able to return to sports at the same levels as before [28].