Management of Patella Fractures After Total Knee Arthroplasty
Charles Nelson
INTRODUCTION
Patella fractures following total knee arthroplasty (TKA) are very different from traumatic patella fractures. Whereas traumatic patella fractures in nonarthroplasty patients tend to be associated with reasonably good outcomes with internal fixation, TKA patients tend to be older, have by definition had at least one prior surgical procedure to the knee that likely disrupted at least a portion of the patellar blood supply, and if they underwent patellar resurfacing, have less patellar bone stock, with less area for internal fixation and less surface area for healing. Additionally, osteonecrosis may be present because of disruption of the geniculate blood flow as well as from thermal necrosis caused by the exothermic reaction of polymerizing PMMA cement. Furthermore, TKA alters normal knee kinematics and proprioception under optimal conditions. In the setting of malrotation or malalignment, TKA may further alter kinematics and joint forces, predisposing to patellar fracture and patellar dislocation or subluxation. When malalignment and malrotation following TKA are not corrected during surgical management of a post-arthroplasty patella fracture, these abnormal forces may lead to failure of an otherwise excellent repair or reconstruction.
Indications
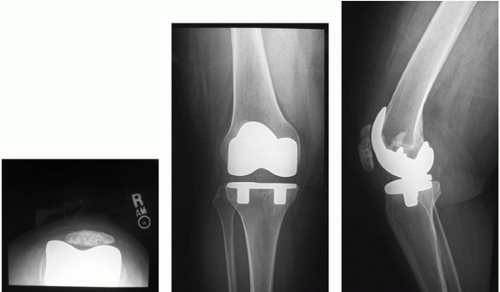
Patella fractures are often noted incidentally following TKA. Fractures noted incidentally on postoperative radiographs without associated symptoms may be successfully treated without surgery. Acute patellar fractures with a minimally displaced transverse component (typically displacement <5 mm) but with an intact extensor mechanism and no patellar component loosening are best managed in a locked brace or cast. In the setting of an acute fracture, immobilization in extension for approximately 6 weeks is recommended. For asymptomatic fractures noted incidentally with an intact extensor mechanism and well-fixed patellar component, observation alone is indicated (Fig. 30-1).
Although it is preferable to treat many patella fractures nonoperatively, there are some patients for whom surgery provides the only opportunity to achieve satisfactory outcomes. Indications for surgical treatment of periprosthetic patella fracture after TKA include displaced fractures with a disruption of the extensor mechanism (often manifest by displacement >5 to 10 mm and an extensor lag >20 degrees or a complete inability to extend the leg) and symptomatic fractures associated with patellar component loosening. Unfortunately, for patients who require surgical management for patella fractures after TKA, the outcomes of surgical management have often been poor (1, 2, 3, 4, 5).
CONTRAINDICATIONS
Surgical intervention is not indicated for the following fractures:
Asymptomatic and symptomatic periprosthetic patellar stress fractures
Asymptomatic fractures noted incidentally on radiographs
Nondisplaced fractures
Displaced transverse, longitudinal, and comminuted fractures with an intact extensor mechanism, well-fixed patellar implant, good function, and no or minimal pain
Most vertical fractures
Even in the setting of patellar component loosening, surgical intervention is generally not recommended if the extensor mechanism is intact when the patient has no or minimal symptoms, although retrieval of the patella component is recommended in this rare situation once fracture healing has occurred.
PREOPERATIVE PREPARATION
Preoperative evaluation of any patient in whom surgical management is indicated with a patella fracture after TKA includes an assessment of the femoral, tibial implants and patellar implants. A clinical and radiographic evaluation is performed to rule out infection, component loosening, instability, stiffness, neuropathic pain, and referred pain. It is important to pay particular attention to femoral and tibial component alignment and rotation. Many patients who develop patella fractures following TKA have component malalignment, malposition, and/or malrotation, as well as overstuffing of the patellofemoral compartment, which must be corrected to ensure success of surgical treatment of periprosthetic patella fractures (6,8).
Anteroposterior and lateral radiographs on a long cassette or 3-foot film are most useful for evaluating component alignment. Tangential patella views allow assessment of patellar tracking and may provide clues related to femoral and tibial rotation. Both lateral radiographs and tangential patellar views may allow analysis of whether the patellofemoral joint has been overstuffed, particularly when compared with preoperative radiographs or the contralateral knee. Computerized tomography is particularly valuable in evaluating appropriate femoral and tibial component rotation.
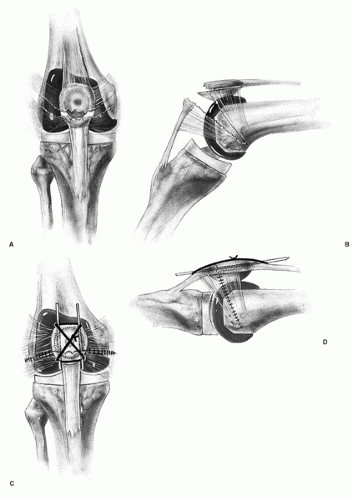
Ortiguera and Berry proposed a classification scheme that is helpful in the management of patellar fractures after TKA (Table 30-1) (1). An algorithm has been recommended based on this classification scheme (1,8). For type 1 fractures, nonoperative management with either observation or immobilization in extension is recommended. For type II fractures, extensor mechanism repair with partial or complete patellectomy or open reduction with internal fixation is recommended. For type III fractures, operative treatment has been recommended if the patient is sufficiently symptomatic. For type IIIa fractures, patelloplasty with either patellar component revision or resection arthroplasty has been recommended. For type IIIb, patellar component removal with patelloplasty or complete patellectomy has been advised. Extensor mechanism allografting can be performed early for type III fractures or later if other treatment methods have failed (8).
The surgical options for treating periprosthetic patella fractures include open reduction and internal fixation, partial or complete patellectomy with extensor mechanism repair or reconstruction, and patellar component removal with or without resurfacing. Preoperative planning requires that the surgeon make certain the instruments, implants, and allograft tissues (when appropriate) needed for primary and contingency treatment plans are available. Contingency plans should include revision femoral and tibial implants and instrument sets in case femoral and/or tibial component revision is necessary.