CHAPTER 38 Management of Loose Bodies and Other Limited Procedures
INTRODUCTION
The arthroscope has proven itself to be ideally suited for the removal of elbow loose bodies and is the most common indication for elbow arthroscopy.4,16,26 Other limited procedures such as débridement and synovectomy are also very amenable to arthroscopic management. Elbow arthroscopy has, in fact, proven itself valuable in the treatment of many elbow conditions.1,3,4,8,12,14–16,28,31,34 The potential advantages of elbow arthroscopy in the identification and removal of loose bodies include reduced iatrogenic insult using limited portal site incisions, a more thorough and complete assessment of the anterior and posterior compartments of the elbow, and possibly reduced propensity for scarring postoperatively as a result of limited disruption of the elbow capsule. Disadvantages of elbow arthroscopy center squarely on the technical requirements to safely and effectively perform the procedure due to the close proximity of neurovascular structures. A thorough knowledge of the anatomy of the elbow, particularly from the arthroscopist’s perspective, is critical in reducing the chances of neurovascular injury.33 Preinsufflation of the joint with fluid and maintaining the elbow at approximately 90 degrees of flexion during the procedure increase the distance of the neurovascular structures from the articular surfaces and arthroscopic instruments, decreasing the chance of morbidity from portal placement.17 Also, drawing the anatomic landmarks, including marking the location of the ulnar nerve at the initiation of the procedure, probably serves to reduce the risk of injury to these structures as well.32
LOOSE BODIES
Patients with loose bodies usually present with complaints of elbow pain and stiffness and often report catching, snapping, popping, or locking of the joint (Fig. 38-1) (see Chapter 84). Loose bodies do not cause elbow contracture, but they are often present in patients with elbow contracture. These patients with elbow contractures develop loose bodies as a result of the underlying pathologic condition such as osteochondritis dissecans, posterior impingement, or degenerative arthritis with posterior osteophytes on the olecranon and in the olecranon fossa. On physical examination, patients with loose bodies generally have maintenance of elbow motion but may have mild degrees of flexion and/or extension loss. Also, a mild effusion best identified in the posterolateral gutter of the elbow may be present.
Although anteroposterior (AP) and lateral radiographs of the elbow often demonstrate loose bodies (Fig. 38-2), as many as 30% of loose bodies are not detected on plain x-ray studies.26,29,41 Most often, when loose bodies are suspected but not identified on plain radiographs, they will be found in the posterior compartment of the elbow25 (Fig. 38-3). In addition, loose bodies will often migrate within the elbow and even between compartments, making reliable identification more difficult.
Computed tomographic arthrography and magnetic resonance imaging may be helpful in diagnosing loose bodies.41 However, even if objective testing fails to demonstrate loose bodies in patients with classic loose body symptoms, elbow arthroscopy may still be indicated because it represents the best diagnostic modality.
SURGICAL TECHNIQUE
Originally, elbow arthroscopy was performed with the patient in the supine position and the hand suspended in traction. Poehling et al33 used the prone position for elbow arthroscopy, allowing improved access to the posterior aspect of the elbow and facilitating the conversion to open procedures when necessary. O’Driscoll and Morrey27 have popularized the lateral decubitus position. In this position, the arm is placed across the chest. All of these positions are acceptable for removal of loose bodies, but the posterior compartment, where loose bodies are more often found, may be more difficult to access with the patient in the supine position. Regardless of patient position, a thorough assessment of both the anterior and posterior elbow compartments is required. In many patients, more loose bodies are identified at arthroscopy than can be seen on preoperative radiographs.27
Once the patient has been properly positioned, careful palpation of the anatomic structures, particularly the ulnar nerve, is imperative. A dislocated or subluxatable ulnar nerve is present in 16% of the population,5 and care should be taken to ensure that the nerve can be identified in its normal anatomic location. Next, 20 to 30 mL of sterile saline is injected into the joint using the straight posterior or soft spot portal location. Insufflation should continue until some resistance to further fluid injection is felt. Complete filling of the joint with fluid ensures a tight elbow capsule, making joint penetration with the arthroscopic trocar and cannula safer and more reliable.
A proximal anteromedial portal is established initially, and thorough arthroscopic assessment of the anterior elbow joint is carried out. Next, a proximal anterolateral portal may be established. On identification of loose bodies, they can be removed using a variety of arthroscopic graspers (Fig. 38-4). Loose bodies can be surprisingly large and may require a bigger grasper. In fact, these loose bodies will often be larger than the plastic cannula used in the procedure. Options for removal of large loose bodies include either breaking the loose body into more easily removable fragments or grasping the loose body with a large grasper and backing the cannula out of the elbow while keeping this loose body in contact with the tip of the cannula. Additionally, the arthroscopic camera can be used to help push the grasped loose body out of the opposite side of the elbow. Other tips for removal of loose bodies include “pinning” the loose fragment with a spinal needle to provide resistance for grasping the loose body.
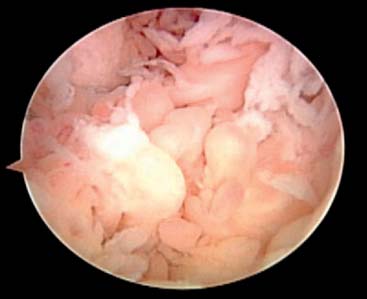
Débridement of osteophytes or loose articular fragments, and arthroscopic management of other anterior compartment pathologic conditions may be necessary at the time of loose body removal. Also, inflammatory tissue and reactive synovitis may be present, and synovectomy should be carefully performed as well11,13,20 (Fig. 38-5). However, use of motorized shavers around the anterior capsule can lead to perforation of the capsule and put the neurovascular structures at increased risk for injury. A thorough synovectomy is important, however, to maximize the outcome of arthroscopic treatment and to help identify loose bodies that can sometimes be obscured by the presence of this synovial tissue. The supplemental use of arthroscopic retractors is valuable and effective in improving visualization during procedures such as synovectomy and in providing additional protection of the capsule and the adjacent neurovascular structures. These retractors can be placed either on the same side as the working portal or opposite that portal depending on the areas to be accessed. In fact, retractors are important to use for a variety of arthroscopic procedures (Fig. 38-6). Blunt-tipped switching sticks and smooth freer elevators can also be used effectively as soft tissue retractors.

FIGURE 38-6 Arthroscopic retractors can improve visualization and protect the capsule and other structures.
Following loose body removal and débridement of the anterior compartment, attention is turned to the posterior compartment. Loose bodies or attached fragments of bone are often present in the olecranon fossa. Leaving the inflow anteriorly may help to “flush out” posteromedial gutter or posterolateral gutter loose bodies as well. In addition, “milking” the gutters, which is accomplished by manually pressing against the posterolateral and posteromedial capsule, may allow for the identification of additional loose bodies located here. Thorough arthroscopic visualization and assessment of both the posteromedial and posterolateral gutters helps to ensure that all loose bodies posteriorly are identified. Limited arthroscopic débridement of soft tissue, particularly in the posterolateral gutter, is often required to view all of the articulating surfaces and to identify loose bodies in this area. Finally, as is the case for the anterior compartment, débridement and removal of reactive tissue and prominent osteophytes posteriorly is important as well.
OUTCOMES
Multiple studies have demonstrated the effectiveness of elbow arthroscopy in the diagnosis and treatment of loose bodies, with success rates of 90% reported.4,16,23 In a review by O’Driscoll and colleagues,26 70% of 71 consecutive elbow arthroscopies were therapeutically beneficial, with loose body removal being the most successful procedure. In fact, all patients with isolated loose bodies benefited from the intervention. However, it is also important to recognize that loose body removal without supplemental arthroscopic management of osteoarthritis has not been found to help patients significantly.23,26,29
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree