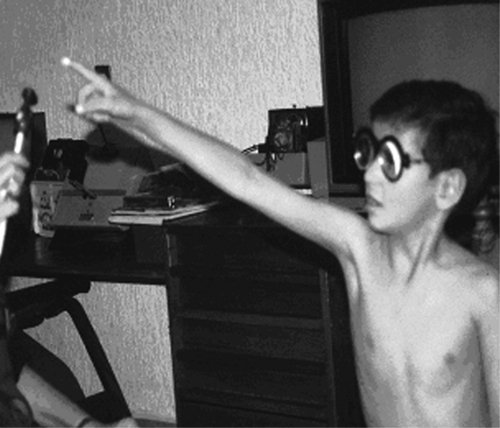
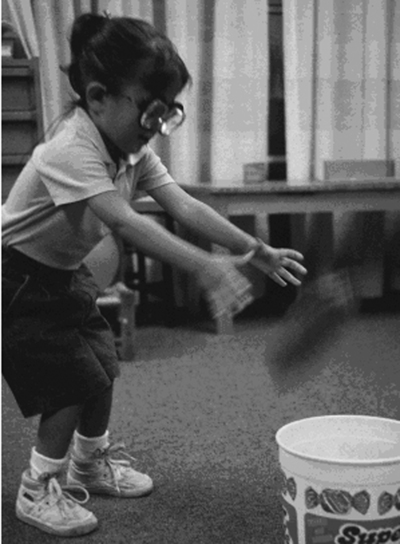
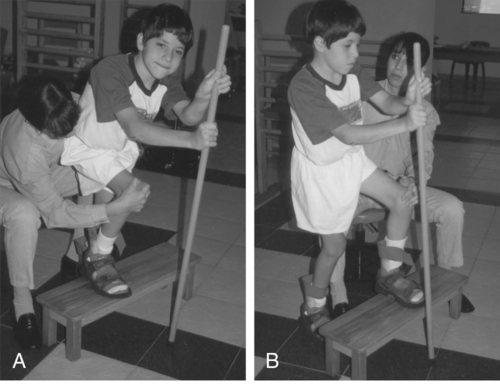
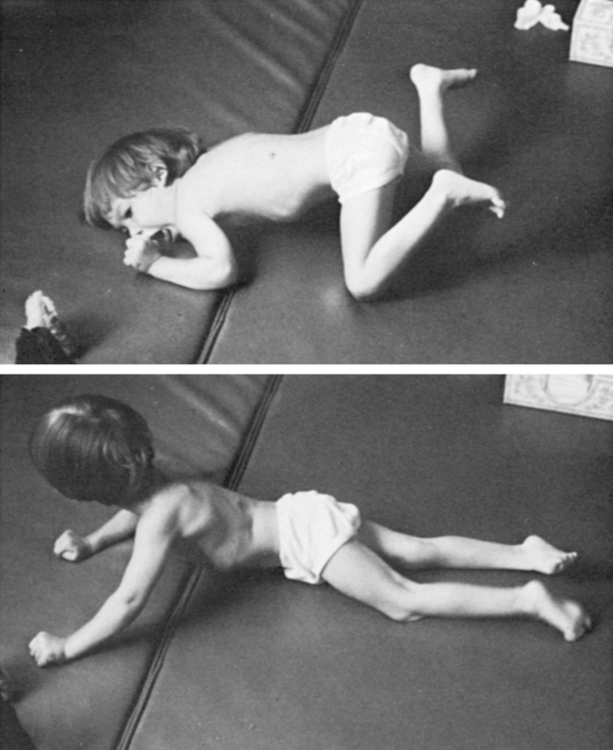
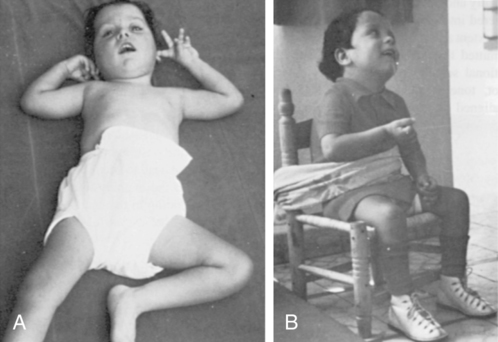
CLAUDIA R. SENESAC, PT, PhD, PCS After reading this chapter the student or therapist will be able to: 1. Identify the parameters of the diagnosis of cerebral palsy including motor, family, and psychosocial components. 2. Analyze the multifaceted aspects of the clinical problem and appreciate a multifaceted approach to evaluation and treatment. 3. Analyze treatment strategies and their application to clinical problems. 4. Identify and critique current research for the pediatric client with cerebral palsy. 5. Identify the therapist’s role in the treatment of the child with cerebral palsy, with family involvement, in different settings, and with other health professionals. Cerebral palsy is a misnomer at best. Little1 suggested the name in the mid-1800s, but there is still no established direct relationship between the identifiable state of the brain and the distortions in posture and movement control that we are able to observe in the individual.2,3 The condition is not always evident at birth, although the work of Prechtl4 statistically supports the possibility of a link between the quality of spontaneous movements in the first months of life and later difficulties in coordinated movement expression. In only a small number of children has a specific lesion been identified that corresponds to the observed motor responses of the child, and this elite group includes children with porencephaly and other early developmental malformations of the brain. Whether there is a biochemical element in the brain of a child that distorts the actual motor learning process has not been established. There is a shocking variability in the age at which intervention is initiated for individual children and a wide variety of programs that do not necessarily take into account the current information available from clinical studies on efficient motor development and brain function. This confusion has led us astray in understanding the process of movement and postural distortion that characterizes children who carry the label of “cerebral palsy.” Historically, the evolution of diagnosis and treatment intervention or management is clear and relates to the recognition of the special needs of this minority of society. The British physician Little identified the condition on the basis of observable characteristics of movement and posture, or—in other words—the external features of the condition, so the initial efforts at remediation fell to orthopedists such as Deaver and Phelps.3,5,6 Deaver placed importance on external bracing that was periodically reduced in the hope that the child would take over control of increasing parts of his or her own body.5 Phelps used bracing and surgery and was a significant force in obtaining schooling for these children in the United States.6 He pointed out that they did not belong in academic classes with children diagnosed as retarded or mentally handicapped and that children with cerebral palsy should be exposed to a traditional academic curriculum. In his Children’s Rehabilitation Institute in Reisterstown, Maryland, he also advocated restriction of a more functional limb to encourage use of the one less used, particularly in work with the upper extremities. In the 1950s and 1960s there simultaneously emerged new theories of neuromotor behavior that redefined the clinical characteristics of cerebral palsy and permitted clinicians to orient their intervention strategies to the principles of motor development and motor learning. Kabat in conjunction with Knott introduced proprioceptive neuromuscular facilitation (PNF), which was applied to children with movement disorders and to adults with a history of trauma.7 The use of diagonal patterns of movement in this approach changed the customary postures of the child and introduced more functional movement patterns in logical learning sequences. Physical and occupational therapist Margaret Rood added the more specific sensory components of ice and light quick brushing of the skin surface to guide the desired motor response.8 She spoke of the need to focus attention on both “heavy work” and “light work” during the early development of movement skills. These terms referred to the central body moving over limb support and limb movement with central stability. Bobath was working in London at this same time and observed the need to have a dynamic interaction between stability and mobility, after finding that inhibition of the reflexive movements was not sufficient to change the functional outcome of the child with cerebral palsy.9 They pointed out that the areas of the child’s body that appeared to be spastic changed when the body was placed in a different relationship to gravity. This observation held up for reexamination the prevailing view of the time, namely, that spasticity existed in a tendon or muscle, a specific structure. When the birth process is prolonged for any of many reasons, the physiological timing of these changes is interrupted. Unique combinations of pressure may make it difficult for the membranous structures to maintain their structural alignment. That lack of structural alignment may persist long after birth and affect future movement and development. Rapid changes of pressure, with minor misalignments of the head and body during the birth process, result in sufficient trauma to affect the nervous system and the delicate fascia and in a small percentage of infants to affect the expression of spontaneous movements. In the majority of healthy infants born at term the spontaneous movements seem to assist in the activation of the central body and the limbs so that physiological changes in the fascia are sufficient to permit a typical expression of developmental movement responses after birth. Body movement and respiration are coordinated with the infant’s physiological rhythms in this initial adaptation to the world of gravity. With complications of the pregnancy or the birth process, these spontaneous movements that are so easily made by the healthy infant become laborious and sometimes impossible, affecting motor actions, postural mechanisms, and the basic physiological rhythms. Cerebral palsy is a heterogeneous collection of clinical syndromes, not a disease or pathological or etiological entity.10 Little described cerebral palsy as “a persistent disorder of movement and posture appearing early in life and due to a developmental nonprogressive disorder of the brain.”3 Current definitions have reiterated that atypical execution of movement and interference with postural mechanisms are the key characteristics of this nonprogressive disorder affecting the developing brain.10,11 Cerebral palsy affects the total development of the child. The primary disorder is of motor execution, but common associated dysfunctions include sensory deficits (hearing or vision); epilepsy; learning disabilities; cognitive deficits; emotional, social, and behavioral problems; and speech and language disorders. The degree of severity varies greatly from mild to moderate to severe.10–12 The clinician must be aware that the categorization of cerebral palsy is based on descriptions of observable characteristics; thus, it is a symptomatic description. The hypertonus of spasticity prevents a smooth exchange between mobility and stability of the body. Constriction of respiratory adaptability occurs with poor trunk control. Incrementation of postural tone occurs with an increase in the speed of even passive movement, and clonus may occur in response to sudden passive movement. Although diagnostic terms reflect the distribution of excessive postural tone, the entire body must be considered to be involved. Spasticity, by nature, involves reduced quantity of movement, which makes its distribution easier to identify. Recruitment of the corticomotor neuron pool is affected in the presence of spasticity, and therefore timing issues result in the poor grading of agonists and antagonists.13,14 There is also a risk of reduction in the range of limb movements over time when therapy does not include active adaptation in end ranges and organization of postural transitions.15 This category (spasticity) has the highest occurrence of cases of cerebral palsy.16 There are several spastic types of cerebral palsy that require clarification. Spastic diplegia implies that the lower extremities are more involved than the upper extremities but could manifest with varying degrees of hand function, and often the involvement is asymmetrical.14 Hemiplegia displays involvement of one side of the body and can manifest itself with the arm involved more than the leg or the leg involved as much as or more than the arm.10 Quadriplegia, as the term implies, involves the entire body.10 Dyskinetic syndromes, which include athetosis and dystonic types of cerebral palsy, are characterized by involuntary movements. The term dyskinetic is commonly used with children who lack posture and axial and trunk coactivation. The excessive peripheral movement of the limbs occurs without central coactivation. Dystonic types of cerebral palsy are dominated by tension, and athetosis usually has a hypotonic base or underlying tone. Dyskinetic syndromes may occur with greater involvement in particular extremities, although the condition most often interferes with postural stability as a whole. When pathological or primitive reflexes are used to accomplish movement, there is a difficulty with midline orientation. Dyskinetic distribution of postural tone is changeable in force and velocity, particularly during attempted movement by the individual. Midrange control is limited if present at all, and frequently end ranges of motion are used to accomplish a motor task.10 For these reasons, these children have a reduced risk for contractures over time. Hypotonicity is another category of cerebral palsy, but it may also mask undiagnosed degenerative conditions (see Chapter 13). Recent reports suggest that “pure hypotonia” is not an attribute of cerebral palsy, and further testing to rule out other causation may be indicated.16 True ataxia is a cerebellar disorder that is seen more frequently as a sequela of tumor removal (see Chapters 21 and 25) than as a problem occurring from birth. Ataxic syndromes are more commonly found in term infants. This type of cerebral palsy is a diagnosis of exclusion. In a small number of patients there is congenital hypoplasia of the cerebellum. Most of these children are hypotonic at birth and display delays in motor acquisition and language skills.10 Recruitment and timing issues remain problems in this population. Trajectory of the limbs, speed, distance, power, and precision are frequently documented as problems in this category. Midline is often achieved, but control of midrange movements of the extremities and control of trunk postural reactions are affected. These classifications, even when accurately applied, give the therapist only a general idea of the treatment problem and must be supplemented by a specific analysis of posture and movement control during task performance, an interview for home care information, and assessment of treatment responses (see Chapters 7 and 8). The therapist is then ready to establish treatment priorities for the individual child. Many of the characteristics described in the preceding paragraphs also apply to children who have had closed head traumas or brain infections. Further information can be obtained in Chapters 24 and 26. Some of the treatment suggestions that follow may also be applied in such cases. As with cerebral palsy, early positioning and handling after trauma may deter later problems. A problem-based approach to the assessment and management of the child with cerebral palsy includes the family as key members of the team.17 While observing the child, the experienced therapist will want to periodically elicit from the parents their view of the problem. By listening carefully, the therapist will also be able to discern the emotional impressions that have surrounded previous experiences with professionals. Sometimes what is not said is more important than what is verbally offered immediately. Listening carefully and clarifying facts are more important than overwhelming the parents with excessive information and suppositions during early contacts. Observation of the family response to information will keep the therapist on track in developing a positive relationship with parents that deepens over time. The therapist’s role is often as interpreter of medical information as parents attempt to make some sense of their child’s diagnosis. The next general step is to observe, in as much detail as possible, the spontaneous movement of the child when separated from the parent (Figure 12-1). Is the child very passive? Does he or she react to the supporting surface (Figure 12-2)? Are there atypical patterns of movement to reach a toy? Are clearly typical responses occurring with specific interference by reflexive synergies or total patterns of movement? Does the child rely heavily on visual communication? Do the eyes focus on a presented object, or does the postural abnormality increase with an effort to focus the eyes? Does the child lead or follow hand activity? Does an effort to move result only in an increase of postural tone with abnormal distribution? Does respiration adapt to new postural adaptations (Figure 12-3)? Is the child able to speak as well while standing as while sitting? This type of observation is valuable because movement patterns directly reflect the state of the central nervous system and can generally be seen while the parent is still handling the child.18 Once the child is on the mat or treatment table, outer clothing can be removed to observe interactions of limbs and trunk. Movement responses of the child can gradually be influenced directly by the therapist. Many disabled children associate immediate undressing in a new environment with a doctor’s office, and the chance to establish rapport is lost. In some instances it is preferable to have the parent gently remove some of the child’s clothing or even to leave the child dressed during the first therapy session. Gaining the trust of the child and parent is crucial during the first few sessions. Standardized assessments are often used by facilities to document the developmental level of the functioning of a child with disability and to justify treatment. The Gross Motor Function Measure (GMFM) was developed to assess children with cerebral palsy and has good reliability and validity for children aged 5 months to 16 years.19,20 The Gross Motor Function Classification System (GMFCS), developed in 1997, is often used in conjunction with the GMFM.21,22 The GMFCS has five levels of classification for gross motor function, emphasizing movement initiation related to sitting, walking, and mode of mobility. Descriptors of motor function span an age range of 2 to 18 years, reflecting environmental and personal factors. The Pediatric Evaluation and Disability Inventory (PEDI) assesses children aged 6 months to 7.5 years in three domains: social, self-care, and mobility.23 The Functional Independence Measure for Children was developed as a test of disability in children aged 6 months to 12 years. This assessment covers self-care, sphincter control, mobility, locomotion, communication, and social cognition.24–26 This tool has been used to track outcomes over time. Although several instruments have been developed that meet psychometric criteria to document function in children with disabilities, the GMFM and the PEDI are thought to be the most responsive to change in this population of children because of their good reliability and validity.27,28 Often the decision to use an instrument to assess development will be left up to the clinician or facility. To date, there is no one tool that will cover all the categories necessary to document change in a child with cerebral palsy, so the clinician will need to rely on observational skills to describe quality of movement and response to changes in position in space and handling. Each child will differ in the ability to separate from her or his parents. Spontaneity of movement, interest in toys, general activity level, and communication skills will also vary from child to child.29 Responding to the specific needs of the child enables the therapist to set priorities more effectively. If fatigue is likely to be a factor, it is important first to evaluate those reactions that present themselves spontaneously, followed by direct handling to determine the child’s response and potential for more typical movements. Movements or abilities for which there is a major interference from spasticity, reflexive responses, or poor balance may be better checked at the termination of the assessment so that the child remains in a cooperative mood as long as possible. Information regarding favorite sleeping positions, self-care independence, and chair supports used at home can be requested as the session comes to a close. Clinical reasoning involves taking information from the assessment, including observations, results from standardized tools, family input, and the therapist’s handling of the child to formulate a treatment plan. Placing this information into a framework that makes sense to the therapist, the physician, other health professionals, and the family will assist in goal writing. The International Classification of Functioning, Disability and Health (ICF)30 is well known in the field of health care and allows one to see the overall interaction of the person with his or her environment and activities in the presence of the health condition.30 If the child totally avoids certain postures during spontaneous activity, these are likely to be the more important positions for the therapist to evaluate. Observing how the child conforms to the support surface and how much contact there is with the surface will provide information about the ability to initiate movement from the surface. Support surface contact is essential for weight bearing and weight shifting to occur; both are critical for movement. Placement of the child in the previously avoided position will permit the therapist to feel the resistance that prevents successful control by the child.29 As mentioned previously, this may be held for the end of the assessment. The parent should play an active role in the assessment whenever possible. Continued dialog with the parents reveals factors such as the frequency of a poor sitting alignment at home or a habitual aversion to the prone position. Sitting close to the television set or tilting the head when looking at books should also be noted so that functional vision skills can be related to other therapy interventions.31 These contributions by the parents establish the importance of good observation and the need for parents and the therapist to work cooperatively. Therapists of different specialties need to initiate continuing communication to coordinate therapy objectives. According to the guide for typical development, infants should be able to maintain the posture in which they are placed before they acquire the ability to move into that position alone.32,33 The problems presented by cerebral palsy occur to some extent as a reaction to the field of gravity in which the child moves.32 Visual perceptions of spatial relationships motivate and determine movement patterns while the child must react at a somatic level to the support surface. It is helpful, therefore, to attempt placement of the infant or child into developmentally or functionally appropriate postures that are not assumed spontaneously (Figure 12-4). Resistance to placement indicates an increase in tone, a structural problem, or an inability to adapt to the constellation of sensory inputs for that alignment. A movement that resists control by the therapist will be even less possible for the child. What appears to be a passive posture may hide rapid increases in hypertonicity when movement is initiated or instability of a proximal joint when weight bearing is initiated. A child may have learned to avoid excitation of the unwanted reactions and may fix the body position to avoid the alignment that cannot be controlled. Another child may enjoy the sensory experience of accelerated changes in postural tone and deliberately set them off as a means of receiving the resulting stimulation to his or her system. It is the visual-motor aspect of performance function that is of primary concern to the therapist because spatial judgments are needed to control movement of the body in an upright alignment. The infant who is able to stand and walk along a support and then seems unable to let go of the support is often found to have functional vision interferences. The child with cerebral palsy most often demonstrates significant neuromotor delay in the developmental process, which often results in the inadequate establishment of matching of inputs from the postural and visual systems (Figure 12-5). Visual-motor learning experiences are filled with compensatory responses from both systems. Vision plays an important role in early motor development for learning about, manipulating, and exploring the environment. Therefore vision requires attention during the assessment of motor abilities. (Refer to Chapter 28.) The visual system in its development has many parallels with the postural system.34 Binocular control and freedom of movement are necessary for the system to function properly. Ambient visual processing must be integrated with central visual processing to take in information that relates to position in space and to focus on a particular target. A simple screening examination may check acuity at 20 feet on the E chart and declare vision to be normal. An ophthalmological examination is needed to determine the health of the eye structures, particularly in the case of infants born preterm. Equally important is a functional vision examination given by a behavioral or developmental optometrist to reveal the level of efficiency that the two eyes have achieved in working together and whether the ability to focus in far and near ranges is smoothly established. Strabismus dysfunctions commonly coexist with cerebral palsy and may cause the child to receive a double image of environmental objects. Judgments about space are related to a three-dimensional perception of the surrounding environment, which requires coordinated use of the two eyes. Conservative management of eye alignment problems is done with the use of lenses and prisms by the experienced optometrist, which permits the therapist to work for basic head control by the child before any irreversible changes are made to the eye muscles. Eye movement differentiates from head movement in much the same way that the hand differentiates from general arm movement, corresponding to general maturation of the central system. Because the visual system is first a motor system, children with cerebral palsy most often have difficulty separating eye movement from head movement and controlled convergence for focal changes. When their posture is supported, eye movement can proceed to evolve in accuracy and complexity. With inadequate alignment of the head in relation to the base of support, the visual system accumulates distortions and inconsistent input, which leads to the formation of an inadequate perceptual base for later motor learning (see Chapters 4 and 28). Even after improvement in the control of posture and movement, the visual system continues to adapt to the previous faulty visual-motor learning, resulting in perceptual confusion and inefficient organization of body movement in space. The therapist who is working for improved motor control may notice that such a child reacts with adequate postural adaptations when facing the therapist or a support and that the movement quality seems to disintegrate when the child faces an open space. This immediately jeopardizes the ability of the child to use her or his new responses after leaving the therapy environment. Visual orientation to the environment will dictate alignment against gravity, and the reverse is also true; poor alignment against gravity will affect visual orientation to the environment. Movement, postural stability, and muscle activation are closely related to vision.35 Padula, a behavioral optometrist specializing in neuro-optometric rehabilitation, has described a posttrauma vision syndrome in adults with acquired central dysfunction and has applied this information to children with cerebral palsy.36 A perceptual distortion in the perceived midline of the body, known as visual midline shift syndrome, is corrected with the use of prescribed prism lenses, which then permits the child to step into the perceived space with more confidence (Figure 12-6). The observant therapist will begin to notice that the sudden increase in neuromuscular tension in a child taking steps in a walker is often accompanied by closing of the eyes. This seems to be a momentary inability of the central processing system to integrate the information arriving from different sources. With the use of prism correction, the child experiences the body as more coherent with visual-spatial perceptions. By incorporating an understanding of visual observations into intervention strategies, physical and occupational therapists are able to note compensatory adaptations by the complementary systems and use them to their advantage in effective treatment intervention. Some children who walk on their forefeet or even on their toes and who have made little if any permanent gait change after the use of inhibitory casting or orthotics also fall into the population described previously. With prisms that correct the perception of forward space, the child places the entire foot in contact with the support. Such prism lenses are used during therapy handling as a perceptual learning experience for the child, with the optometrist and the therapist coordinating their efforts. Hand-coordination activities also require timing of reach and grasp that is based on feed-forward input from the visual system.35 In some cases the therapist observes the visual system to overfocus in the moment that the child loses control of his or her postural stability. This suggests that the visual system may be attempting to compensate for the inadequacy of the postural control, much in the same way that we all adjust our head position to see better. Understanding the nature of the continuing dynamic interaction between these two functional subsystems of the central nervous system and attending to the needs of visual-postural orientation will increase the successful evolution of clients with cerebral palsy. The quality of a body posture or position in space determines the quality of the movement that is expressed. Lack of head control, poor midline organization, and deficient trunk strength begin the process of compensation. From a distorted starting position the movement initiated is one that is restricted (Figure 12-7). The lack of central “core” stability in the body restricts the full mobility of a limb. This limitation over time is increased by fascial and muscular restrictions on smooth coordinated muscle action. The child continues to learn the atypical responses because the movement patterns tend to be reinforced by either accomplishment or reinforcement of some kind from the environment. Compensatory movement patterns evolve because of necessity rather than any feedback as to efficiency or functional smoothness. Active therapy intervention allows the sensorimotor learning of the child to be modified so that some part of the compensatory response becomes unnecessary and the movement becomes more typical (Figure 12-8). This relative approximation of what is expected in a typical response may occur in the area of initiation, timing, strength, or ability to sustain an antigravity alignment. As movement expression and postural stability are better established, the compensatory patterns are used less often, and new motor learning occurs on a base of closer-to-normal experience. Compensatory processes have their positive aspects.37 The independence finally achieved by the older child reflects her or his intelligence and motivation and the family’s attitude toward the child and the disability. The most debilitating handicap of cerebral palsy in an intelligent child may be social or psychological when the child is not accepted by the family and therefore cannot develop a positive self-image. Compensatory movement patterns may permit greater independence, if and when they do not limit or block the active learning of new motor strategies. Nutrition is viewed as providing an important biochemical base for enhanced human performance. Williams,38 author of the classic reference Biochemical Individuality, was one of the first to point out the existence of significant variability in the need for specific individualized nutrients because of differences in assimilation and other factors. Physicians Crook and Stevens,39 Smith,40 Pfeiffer,41 and Cott42 are a few of the leaders who have analyzed the link between nutrient intake and behavioral differences in children and adults. Many of these references address issues of attention and learning. To have efficient function of the transmitters at the myoneural junction and good health for the myelinated neurons of the nervous system, a variety of trace elements must be present.41 Lack of dendritic proliferation is associated with malnutrition regardless of the cause.43 The ambulatory child with cerebral palsy will need to be considered for a new level of energy expenditure to avoid short stature and poor nutritional status.44 Another body of work explains more about the direct link between food intake and muscle efficiency for high performance and normal function. The need for water is paramount for healthy fascia. In children with cerebral palsy and related disorders there is often from the beginning a difficulty in the smooth automatic sucking needed for nutritive intake. Uncoordinated patterns of mandibular and tongue motion persist when not addressed in early and precise intervention strategies. Even the digestive process is affected negatively by inadequate chewing, a higher-than-typical percentage of food allergies, and less-than-efficient physiological functions.45 It is likely that brain dysfunction in some of these children extends to the hypothalamus, thus influencing the entire digestive process. Duncan and colleagues46 have documented the risk of osteopenia in nonambulatory children with cerebral palsy. This retrospective study showed that fewer than 75% of the calories needed were administered to 95% of the children with gastrostomy tubes. Nutrients were also deficient. This may explain part of the poor physical response level of such children. Sonis and colleagues47 looked specifically at energy expenditure in children and adolescents with spastic quadriplegia in relation to food intake. They found dietary intake to be markedly overreported for this population and determined that nutrition-related growth failure was likely related to inadequate energy intake. Reflux is also common in infants with developmental problems. In some infants reflux subsides as the physical stress is reduced in the tissues bordering the upper thoracic and cervical spine, but it can be related to milk sensitivity or even susceptibility to environmental contaminants. To supplement nutritional intake in the child with cerebral palsy, the individual child must be considered with regard to age, size, activity level, and growth factors.48 Ideally, blood, urine, or hair analyses would be done to determine nutrient imbalances, and supplementation with specific nutrients would be guided by a specialist. Environmental medicine has taken the lead in this type of work. The rehabilitative process places increased demands on the entire system and requires fuel to set the stage for improved muscle function. Protein, carbohydrates, and adequate hydration are sources that build muscle and provide a foundation for strengthening and the advancement of motor skills in populations without disability.49,50 A well-balanced diet will provide the requisite energy for exercise. However, little research has been done specifically on children with cerebral palsy and appropriate levels of protein during exercise. Therefore it is necessary to discuss these issues with the family using caution unless specifically trained to do so. A nutritional consultation is warranted when concerns arise in this area. Shintani and colleagues51 performed a careful study of 233 children with cerebral palsy to determine the presence of obstructive sleep apnea. In 10 children with cerebral palsy who were received at the hospital for treatment of severe obstructive sleep apnea, these authors determined that adenoidal or tonsillar hypertrophy were noted in only four children and that the main cause of sleep apnea in the other six children was pharyngeal collapse at the lingual base. Fukumizu and Kohyama52 looked at central respiratory pauses, sighs, and gross body movement during sleep in 19 healthy children, ages 3 months to 7 years. Central pauses occurred more often during non–rapid-eye-movement sleep and increased with age. Developmental differences need further study. Decreased oxygen levels have been associated with impaired cognitive and physical performance in the literature.53 In the presence of inadequate peripheral oxygen saturation, low levels of oxygen can be administered during the night. This practice has been used with selected low-tone and athetoid children for improved energy during the day during growth changes, but formal study is needed on a larger group of children with cerebral palsy. Better oxygenation of the tissues can also result in increased food intake and consequently improved energy levels. The primary role of the therapist is in direct treatment or physical handling of the child in situations that offer opportunities for new motor learning. This should precede and accompany the making of recommendations to parents, teachers, and others handling the child. Positioning for home and home handling recommendations should always be tried first by the therapist during a treatment session. As noted for the initial assessment, many interventions will cause a reaction unique to the particular youngster.29,54 It is the role of the therapist to analyze the nature of the response that is accompanied by adaptation inadequacies, to analyze the movement problems, and to choose the most effective intervention (Figure 12-9). It will then be possible for other persons to manage play activities and supervise independent functioning that reinforce treatment goals.55 Simple documentation of observed changes in a child over a series of regular clinic visits is still too common for many children with cerebral palsy. Regular appointments, with periodic assignment of a new piece of apparatus, do not constitute active treatment. Although physical intervention in the form of direct handling of the child is considered a conservative treatment by most physicians, relatively few children receive sufficient physical treatment at an early age.56,57 Therapists need to demonstrate their unique preparation and describe their interventions in ordinary language so that families as well as other health care professionals understand the importance of specific treatment versus general programs of early stimulation that are designed for neurologically intact infants. The prognosis for change in cerebral palsy is too often based on records of case management rather than on the effect of direct and dynamic treatment by a well-prepared therapist. Bobath32,58 documented accurately the developmental sequence expected in the presence of spasticity or athetosis. Her book consolidates some observations of older clients that help professionals understand the uninterrupted effects of the cerebral palsy condition. In any institution one can observe the tightly adducted and internally rotated legs, the shoulder retraction with flexion of the arms, and the chronic shortening of the neck so common as the long-term effects of cerebral palsy. The long-term influence of athetosis results in compensatory stiffness or limited movement patterns to create a semblance of the missing postural stability while a limited number of movement patterns with limited degrees of freedom are used to function (Figure 12-10). Within the clinical community there is increasing evidence that soft tissue restrictions further limit spontaneous movement in children with cerebral palsy. The fact that these fascial restrictions are often found in infants suggests that they originate early rather than as a gradual result of limited ranges in movement. Because of the tendency of fascial tissue to change in response to any physical trauma or strong biochemical change, some of these characteristics might be originating with traumatic birth experiences, and they would be exacerbated by daily use of limited patterns of movement. Tissue restrictions can also occur with immobilization or general infectious processes.59–61 Soft tissue begins to change its physiological structure with the application of gentle sustained pressure, so it serves as documentation that there are changes caused by the therapist’s simple hand contact. Some of the sensory information in the form of tapping or holding or application of pressure affects fascial meridians and muscle alignments.62 A therapist must be prepared to defend his or her approach with a solid foundation, theory, and objective outcomes. Objective documentation is important when dealing with any population but essential for demonstrating therapeutic change. Applying specific soft tissue treatment techniques to any person with a neuromotor disorder creates the need for immediate follow-up with practice of new skills using this improved range of motion. Creating excessive tissue mobility in a given area of the body can destroy the delicate patterns of coordination that permit synergic function in the person with cerebral palsy, so functional activation of the body after each specific mobilization is strongly recommended to integrate the tissue change. Well documented in the literature on current motor control and motor learning is the need to practice, practice, practice.63 Practice time is related to skill performance; the amount and type of practice are determined by the stage of learning that an individual is in and the type of task to be learned63–65 (see Chapter 4 on motor control and learning). Interestingly, most of what we know about motor control and motor learning is based on individuals who are “typicals,” and it is yet to be determined whether the same principles that are considered important in healthy individuals apply to people with disability. However, it makes sense that practice would influence the use of any new or relearned skill. An occupational therapist, Josephine Moore, stressed Bach-y-Rita’s66 works to emphasize some important points for therapists regarding the concept of increasing functional demands on the central system and the importance of the neck structures in developmental movement sequences. Children with spasticity often have a lack of developmental elongation of the neck, whereas children with athetoid or dystonic movement lack neck stability and consistent postural activation. Tone changes often originate with changes in the delicate postural interrelationship between head and body or with ambient visual processing. By appreciating the abundance of polysynaptic neurons and parallel processing in the central nervous system, the therapist will become more optimistic regarding his or her role as facilitator and feedback organizer to guide new movement. Restak,67 in his book The New Brain, confirms the continual reorganization of the brain in response to new input. Several animal and human studies on neuroplasticity have confirmed that the brain reorganizes after an injury and that this reorganization is shaped by rehabilitation and motor skill learning.68–71 In the child with cerebral palsy, the therapist looks for subtle changes in the child’s response to determine newly integrated sensorimotor learning. For example, excessive emphasis on extensor responses in the prone posture for the older child can jeopardize the quality of neck elongation in sitting, so it is essential to work on the components necessary for control of the new posture desired. The direct treatment of infants deserves special mention because there are significant differences in intervention strategies for the infant and the older child. Aside from the delicate situation of the new parents, the infant is less likely to have a diagnosis and presents a mixture of typical and atypical characteristics. It is essential that the clinician have a strong foundation in the nuances of typical developmental movement and early postural control.4,72 Soft tissue issues must be addressed in detail. Direct intervention can be offered as a means of enhancing development and overcoming the effects of a difficult or preterm birth. It will be important, however, to pursue a diagnosis for the infant who reaches 8 or 9 months of age and continues to need therapy because third-party payers often require a diagnosis beyond developmental delay or prematurity. Infants with early restrictions in motor control should be followed until they are walking independently, even if they no longer need weekly therapy. Infant responses can change rapidly as the therapist organizes the components of movement control. Soft tissue restrictions should be treated initially to have more success with facilitated movement responses. Careful observation is essential because all but the severely involved infant will change considerably between visits. The therapist should invest some time in training the parents to become skilled observers while appreciating the small gains made by their infant. Physiotherapist Mary Quinton73 has written specific intervention strategies for babies (Figure 12-11). Infant massage is important to improve the bonding of mother and child and to improve physiological measures.74,75 Inhibiting or stopping the movement of one part of a movement range or even one limb must be done in a way that permits the child to activate the body in a functional way. The child who lies in the supine position with extreme pushing back against the surface is rarely seen when therapy intervention has started early. The therapist initially eliminates the supine position entirely but would incorporate into the treatment plan the activation of balanced flexion and extension in sitting with the ability to vary pelvic tilt for functional play and reaching (Figure 12-12). The child might later be reintroduced to a supine position with postural transitions that support balanced control of the body with more differentiated movement. One of the primary considerations for the child with spasticity is adequate respiratory support for movement. Mobility of the thoracic cage and the midtrunk must be combined with trunk rotation during basic postural transitions (Figure 12-13). Consideration of age-appropriate movement velocity will guide the therapist in choosing activities that challenge better respiratory adaptability and prepare for speech breathing to support vocalization. The therapist will find it helpful to hum or sing or even make silly sounds that encourage sound production by the child during therapy. Movement of the child’s body changes respiratory demands and frequently results in spontaneous sound production during therapy. Assessing the ability to sustain a breath to speak is easily done during a therapy session by counting the letters in the alphabet that can be said with one breath. This should be done with the child supine and in an upright position because trunk control required while sustaining a breath changes with the posture attained against gravity. Describing the chest shape and movement of the thorax observed can serve to assist the therapist in problem solving and prioritizing the treatment plan. The therapist working with the child with cerebral palsy constantly monitors the quality of the child’s motor response. These continuing observations guide the manipulation of the environment and the assistance given the child to move toward a functional goal. Is the body tolerating the position? Does the child adapt to the supporting surface and use the supporting surface contact for movement initiation (Figure 12-14)? Is the movement of a limb graded and without unwanted associated reactions in other parts of the body? By analyzing the answers to such questions, the therapist is guided to an appropriate sequence of the therapy session and is enabled to set functional treatment goals and realistically change prognoses.
Management of clinical problems of children with cerebral palsy*
Overview
Historical perspective
Diagnostic categorization of the characteristics of cerebral palsy
Evaluative analysis of the individual child
Initial observations and assessment
 Typical infants accumulate a multitude of experiences as they move smoothly in their environments.
Typical infants accumulate a multitude of experiences as they move smoothly in their environments.
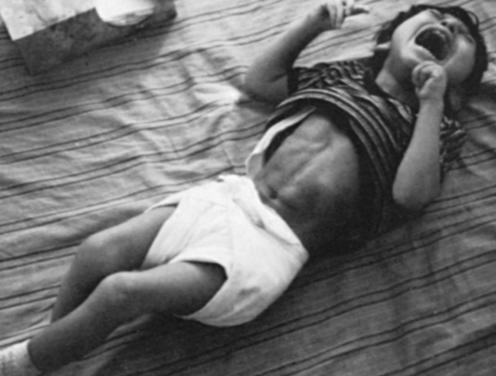
 Emotional reactions are also translated into stronger spastic reactions influencing respiratory adaptation (see Chapter 5 on the limbic system).
Emotional reactions are also translated into stronger spastic reactions influencing respiratory adaptation (see Chapter 5 on the limbic system).
Reactions to placement in a position
Visual-motor assessment
Posture and movement compensations
Other assessment considerations
Nutritional aspects of neuromotor function
Consideration of supplemental oxygen
Roles of the therapist
Role of the therapist in direct intervention
Case management and direct intervention
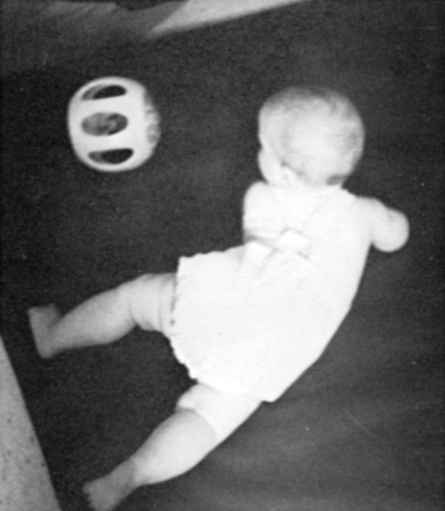
Special needs of infants
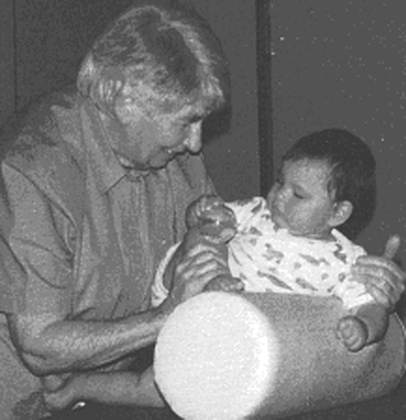
 Mary Quinton, British physiotherapist, is widely recognized as the originator of effective infant intervention.
Mary Quinton, British physiotherapist, is widely recognized as the originator of effective infant intervention.
Orientation to treatment strategies

 Rotational patterns combined with transitional movements can be used to mobilize the thoracic cage.
Rotational patterns combined with transitional movements can be used to mobilize the thoracic cage.

 This child has little contact with the supporting surface, resulting in poor movement initiation.
This child has little contact with the supporting surface, resulting in poor movement initiation.![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree