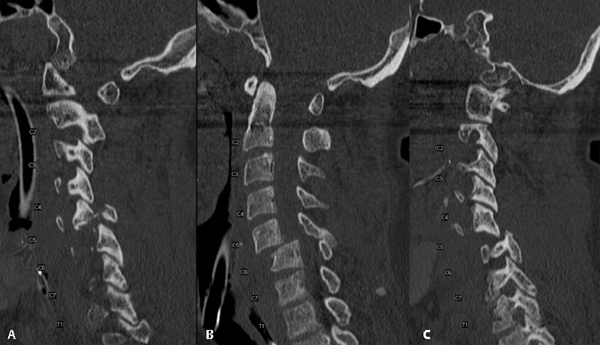
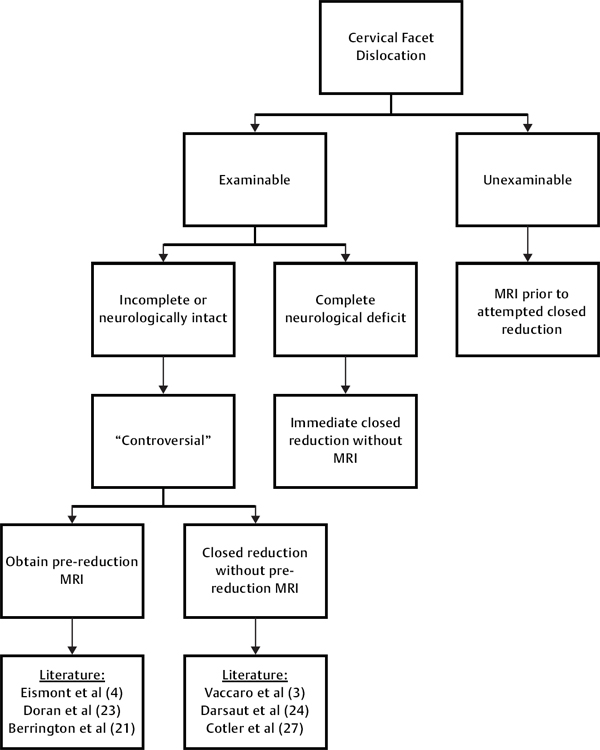
25 Key Points 1. High index of suspicion, strict cervical spine precautions, and complete clinical and radiographic evaluation are vital in patients presenting after trauma. 2. High-resolution multidetector CT scan is the study of choice in initial evaluation for cervical spine injury. 3. Timing of obtaining an MRI scan in patients with cervical facet dislocation is multifactorial and controversial. 4. Surgical technique is dependent on fracture stability, neurological status, presence of disk herniation, and whether a closed reduction is possible. Approximately 15,000 patients sustain spinal cord injury in the United States and Canada per year.1 Up to half of these injuries can be associated with neurological deficits, with initial mortality approaching 10%.2 Management of patients with cervical spine injury is a complex interdisciplinary process that requires efficient and accurate assessment and initiation of care. Cervical facet dislocations result from flexion-distraction forces with or without a rotational component acting on the subaxial cervical spine. Flexion may result from a force onto the occiput or from a deceleration mechanism associated with a motor vehicle collision. The flexion moment occurs around the center of rotation thought to be anterior to the vertebral body, resulting in progressive tension failure. This injury pattern is thought to be a continuum of pathology, with sequential disruption of various osseous and ligamentous structures. Imaging studies reveal that both unilateral and bilateral facet dislocations result from disruption of the posterior musculature, interspinous ligament, supraspinous ligament, facet capsule, ligamentum flavum, and annulus. Bilateral facet dislocations are associated with a statistically significant increase in disruption of both anterior and posterior longitudinal ligaments compared with unilateral facet dislocation.3 Disruption of the annulus raises the potential for extrusion of nucleus pulposus into the spinal canal and may have important implications in the patient management strategy.4 Based on the spectrum of severity, Allen et al. classified these injuries into four stages: (1) facet subluxation, (2) unilateral facet dislocation with 25% displacement, (3) bilateral facet dislocation with 50% displacement, and (4) complete dislocation.5 Patients with unilateral facet dislocations often have either an intact neurological exam or a nerve root injury, whereas bilateral facet dislocations more commonly result in neurological deficit. Among spine surgeons, much controversy surrounds appropriate management of cervical spine dislocations. Traditionally, rapid realignment of the spine through closed traction reduction followed by posterior spinal fixation has been recommended. Others have recommended obtaining an initial magnetic resonance imaging (MRI) scan followed by treatment decisions based on findings of this study. This chapter reviews recent evidence-based literature surrounding various controversies in the evaluation and management of cervical facet dislocations to help guide treatment recommendations. Missed cervical spine injury on initial evaluation has the potential to lead to catastrophic, permanent disability. Therefore, a careful clinical and radiographic evaluation is essential. All trauma patients should be treated as potentially having a cervical spine injury and be initially immobilized in a hard cervical collar. Management of all patients with suspected cervical spine injury should begin with primary survey and resuscitation as outlined by the Advanced Trauma Life Support protocol. Care must be taken to maintain cervical spine precautions throughout the trauma evaluation until appropriate cervical spine clearance can be obtained. Once the patient has been physiologically stabilized, a thorough spine and neurological assessment can be conducted as part of the secondary survey. A well-done history is vital in helping elucidate the mechanism of injury and may help direct evaluation for other concomitant injuries and provide insight on how forces were imparted on the cervical spine. In addition to documenting details of the actual trauma, it is important to inquire regarding associated conditions and comorbidities that may be relevant in a patient suspected of having cervical spine injury (e.g., ankylosing spondylitis). The patient should be logrolled and each individual spinous process should be inspected and palpated to detect posterior midline tenderness and to detect step-off. While the patient is in a logrolled position, a rectal examination can assess for presence or loss of tone. The patient should be inspected for rotational or angular deformity that may point to a unilateral facet dislocation. A complete motor, sensory, and reflex examination should be done and should be clearly documented prior to the initiation of any treatment. A more detailed review of evaluating patients with spinal cord injury is presented in Chapter 2. Controversy about pharmacological treatment of patients with spinal cord injury, including methylprednisolone, is discussed in Chapter 10. Despite efforts to standardize radiographic evaluation in patients with suspected cervical spine injury, protocols remain highly debated and variable across institutions. Two large, prospective, multicenter studies have attempted to clarify the criteria for obtaining radiographs in patients presenting with possible cervical spine injury.6,7 These studies have become the cornerstone for emergency room trauma spine evaluation and been incorporated into triage trauma protocols at many institutions to determine the need for cervical spine screening imaging. Specific guidelines exist for clearance of cervical spine injuries in patients who are awake, alert, and without distracting injury or evidence of intoxication.7 No consensus, however, exists on evaluation of obtunded or unreliable patients with suspected cervical spine injury. This can often lead to prolonged use of rigid cervical collars until patients can safely be imaged or they regain the capacity to participate in an appropriate clinical examination. Prolonged rigid cervical collar can have significant associated morbidity, including compromised airway management, skin ulceration, limited central venous access, increased intracranial pressure, pneumonia, and deep venous thrombosis.8,9 The lack of consensus has led trauma centers to develop individualized algorithms for clearing cervical spines in obtunded patients. The imaging studies most commonly used include plain radiographs, dynamic radiographs, dynamic fluoroscopy, computed tomography (CT), and MRI. In the past 15 years, helical CT has replaced traditional cervical spine radiography at most large US trauma centers.10 An updated consensus document published by the Eastern Association for the Surgery of Trauma in 2009 reported that plain radiography has been supplanted by CT as the primary screening modality in patients requiring imaging of suspected cervical spine injury.11 The helical CT scan is especially useful for closer examination of suspicious or poorly visualized areas in the upper cervical spine or cervical thoracic junction. These images can also be reformatted into two- and three-dimensional reconstructions to assist the spine surgeon in evaluating complex injuries and in preoperative planning. Studies also show that helical CT scan of the cervical spine requires half the time of obtaining the standard six views of the cervical spine.12 If the rate of missed fracture is incorporated into the analysis, helical CT has been shown to be more cost-effective in the long run. Widder et al. performed a prospective study comparing plain radiographs and CT scans in detecting cervical spine injuries in obtunded patients and found the sensitivity, specificity, and accuracy of plain radiographs to be 39%, 98%, and 88%, while CT scans had a sensitivity of 100%.13 McCulloch and colleagues prospectively analyzed over 400 consecutive trauma patients and found plain radiographs to have a sensitivity of only 52% in detecting cervical spine fractures, compared with 98% for CT scans.14 There has been a recent trend in high-risk level 1 trauma patients toward using helical CT scans alone as a primary screening tool.15 Some potential pitfalls exist in exclusive use of helical CT. One caveat is that standard lower-resolution multislice helical CT may miss subtle spinal fractures, and not all institutions are equipped with a higher-resolution CT scanner. The downside to high-resolution multidetector CT scans is that they expose the patient to higher levels of radiation than a standard CT scan. No current studies compare sensitivity and specificity of various types of CT scanners in detecting cervical spine injuries. Figure 25.1 displays an example of a sagittal CT scan obtained in a blunt trauma patient presenting with a cervical facet dislocation. MRI offers a method of assessing soft tissues and often complements the bony detail provided by CT scans with enhanced depiction of soft-tissue pathology. The use of MRI to identify potential cervical spine trauma missed by CT scan remains controversial. Tomycz and colleagues performed a retrospective analysis of 690 obtunded trauma patients who had undergone both cervical CT and MRI.16 Of the 180 patients (26.2%) with normal CT scans, MRI detected acute traumatic injury in 38 (21.1%). None of the injuries identified by MRI, however, was unstable or required additional surgical intervention. On the contrary, Menaker et al.17 performed a similar analysis of 734 obtunded trauma patients and found a change in management of 7.9% of patients with additional findings on MRI. The incidence of vertebral artery injury in patients with major blunt cervical spine trauma is estimated to be between 24 and 46%.18 Most vertebral artery injuries are asymptomatic due to ample collateral circulation, and it is important to determine which patients should be screened for clinically significant injuries. Insufficient evidence currently exists to support standards or guidelines for either the diagnosis or treatment of these injuries.19 Screening of all cervical spine injuries is not generally recommended because these imaging studies can be associated with complications of their own as well as added financial and technical resource use with no clear clinical benefit. Most spine surgeons advocate obtaining vascular imaging studies when the patient’s neurological findings are suggestive of vascular etiology. Others recommend screening patients with high-risk injury patterns, such as fractures through the foramen transversarium, vertebral dislocations, and upper cervical spine injuries.20 Patients with evidence of posterior ischemia can be managed with either anticoagulation or observation, whereas observation alone is recommended in those with no evidence of posterior circulation compromise. Fig. 25.1 Sagittal computed tomography scan revealing bilateral facet fracture dislocation at the C5-6 level. (A) Scan demonstrating the left facet fracture dislocation. (B) Midline of the scan demonstrating greater than 50% anterior translation of C5 on C6 consistent with bilateral facet dislocation. (C) Scan demonstrating the right facet dislocation. The next step in patients presenting with cervical facet dislocation is to quickly and safely realign the spine. Cervical facet dislocations are often associated with soft-tissue injury, including the presence of possible disk herniation. The presence of a disk herniation does not necessarily result in neurological deficit. Eismont et al.4 and Vaccaro et al.21 define a disk herniation as potentially dangerous when the disk protrudes behind the cephalad vertebral body (Fig. 25.2). Whether an MRI scan is necessary prior to reduction has been a topic of debate since the early 1990s. Some advocate that all patients with bilateral facet dislocation undergo MRI evaluation prior to attempted reduction, due to the fear of neurological deterioration secondary to further posterior disk migration into the canal with a reduction maneuver. Eismont et al. highlighted the danger of closed reduction in a case series of six patients in 1991 with associated cervical disk herniation and facet dislocation or subluxation.4 One of the patients in the series sustained neurological deterioration after reduction was performed under general anesthesia. Other small retrospective case series have recommended MRI prior to reduction secondary to potential neurological deficit as a result of disk herniation during closed reduction.22–24 Fig. 25.2 Prereduction sagittal T2-weighted magnetic resonance imaging demonstrating an associated disk herniation behind the body of C6 in a patient with bilateral facet dislocation. An anterior C6-7 diskectomy was performed prior to intraoperative open reduction. Several subsequent studies, including a prospective clinical trial by Vaccaro et al., suggest that closed reduction in an awake, alert, cooperative patient can be performed safely without a prereduction MRI scan.21 Eleven patients with cervical spine dislocations were prospectively evaluated with pre- and postreduction MRI. Two patients were noted to have a disk herniation prior to reduction. Closed reduction was attempted in all 11 patients, nine of which were successful. Five disk herniations were found postreduction, none had worsening neurological exams postreduction. Though disk herniations may be increased, the investigators concluded that closed reduction could be safely performed in awake, cooperative patients. Similarly, Cotler and colleagues reviewed a series of 24 neurologically normal patients awake and able to cooperate with an exam. All patients were successfully reduced with increasing traction weight without neurological deterioration. A recent study by Darsaut et al. presented 17 patients with cervical fracture-dislocations treated with closed reduced with in-line axial traction under MRI guidance.25 All patients tolerated traction without neurological worsening; interestingly, the investigators illustrated with a sequential MRI-aided reduction technique that a herniated disk could reconstitute itself into its respective disk space. A survey analysis of the Spine Trauma Study Group (STSG) resulted in highly variable opinions and no consensus on timing or utilization of MRI in cervical facet dislocations.26 There are also no radiological studies to date that explore differentiating disk material from hematoma or that delineate how large a disk herniation must be to cause cord impingement. Surgeon interpretation of a significant anterior lesion is highly subjective, with no clear literature to guide treatment. In the case of an obtunded patient who cannot cooperate with a clinical exam, a prereduction MRI is recommended to gain better understanding of the status of the spinal cord and to delineate any potential soft-tissue or bony structure that may place the spinal cord at risk during reduction. Patients who present with complete or near complete neurological deficit should undergo immediate closed reduction, given that the patient has little to lose and the greatest possibility of neurological functional recovery.27 Figure 25.3 summarizes a general algorithm on how to approach imaging of cervical facet dislocation, along with some of the supporting literature. Reduction and realignment of cervical facet dislocation can either be done with a closed or open technique. If the patient is examinable and a prereduction MRI scan does not show a significant anterior space– occupying lesion, a closed reduction may be considered safe. Without a clear definition of what constitutes a dangerous disk fragment, whether a closed reduction is safe can be debatable. Several articles present level IV evidence that closed reduction in an awake, alert patient can be performed relatively safely.21,28,29 Conversely, no consensus exists on the safety of such a maneuver in obtunded, unexaminable patients. Most would agree that a closed reduction should not be attempted in obtunded unexaminable patients in most circumstances. An open reduction with or without decompression can be considered in patients having undergone a failed attempted closed reduction after an MRI scan is obtained or when a dangerous herniated disk is present on prereduction MRI. When an open reduction is deemed necessary, a preoperative MRI should be obtained to assess the status of the disk and would help dictate surgical approach. Fig. 25.3 General algorithm for evaluation of cervical facet dislocation.
Management of Cervical Facet Dislocation
 Evaluation
Evaluation
History and Physical Exam
Screening Radiographic Studies
When to Obtain a Magnetic Resonance Imaging Scan

 Reduction and Realignment
Reduction and Realignment
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Musculoskeletal Key
Fastest Musculoskeletal Insight Engine
