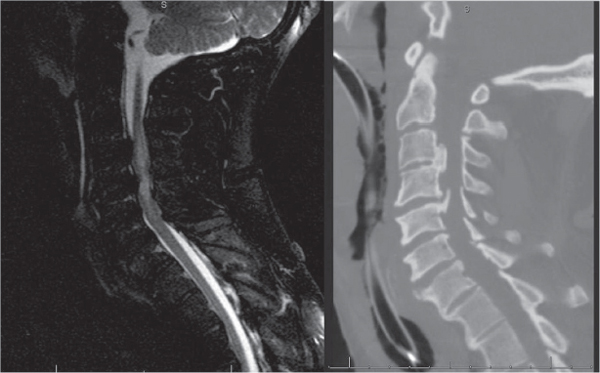
27 Key Points 1. Most spinal injuries in the elderly are cervical, and over 50% of those injuries occur without fracture; the relative proportion of these injuries in the population is increasing. 2. Fractures may not be readily apparent in the spondylotic or spondylitic spine, and the clinician must maintain a high index of suspicion for extension/distraction injury in the setting of advanced degenerative spondylosis. 3. The indications for, and timing of, surgical intervention are controversial, but it is generally agreed that imaging-confirmed spinal cord compression should be decompressed. Early decompression (within 24 hours of injury) is feasible and safe, but prospective data are needed to ascertain the effect of early decompression on long-term outcomes. The reported incidence of spinal cord injury (SCI) in North America varies from 25 to 93 per million population.1–5 The distribution of spinal cord injuries is bimodal, with younger patients generally sustaining injury from motor vehicle accidents and other high-energy mechanisms, and older patients predominantly incurring injury via lower-energy mechanisms, such as falls.6 Accordingly, in the elderly, most injuries are cervical spinal cord injuries, and over 50% of cervical spinal cord injuries in the older population occur without fracture.2 The size of the elderly population is increasing, and this corresponds to an increased incidence of elderly patients presenting with acute SCI: the National Spinal Cord Injury Statistical Center data indicate an increase in the relative proportion of spinal cord injuries that occur in the elderly.6 Given the increasing relative proportion of the elderly in the population, coupled with the increased survival rates for spinal injuries,6,7 it is likely that the management of cervical spine trauma in the elderly will become an issue of increasing relevance in the future. Central cord syndrome describes a neurological presentation of disproportionate weakness of the upper relative to the lower extremities in the setting of cervical spine trauma; the injury mechanism is classically described as that of hyperextension in the setting of a congenitally narrow or spondylotic spine. First described by Schneider et al.,8 the clinical presentation of central cord syndrome was initially hypothesized to be due to injury and subsequent hematoma at the center of the cord (gray matter), with associated damage to the medial fibers of the corticospinal tract. The clinical presentation was hypothesized to be due to the somatotopic organization of the corticospinal tract, in which the fibers for the lower extremities and sacrum were hypothesized to be more superficial and lateral than the fibers corresponding to the upper extremities. Historically, it was hypothesized that the forces resulting from in-buckling of the posterior ligamentum flavum coupled with anterior compression from a spondylotic disk-osteophyte complex (the spinal canal is narrowed by up to 30% in hyperextension)9,10 yielded a net compressive force that was maximal in the center of the spinal cord. Thus, the nidus of injury has historically been described as being in the central gray matter, with subsequent expanding hematoma. More recently, the attribution of the clinical presentation of central cord syndrome to a somatotopic organization of the corticospinal tract (with the upper extremity fibers more centrally located) has been criticized, due in large part to the lack of published literature establishing such an organization of the corticospinal tract in humans and primates.11,12 Jimenez et al.11 examined the cervical spinal cords of five patients with acute traumatic central cord syndrome or Bell cruciate paralysis compared with age-matched controls and found degeneration of the corticospinal axonal tracts, with Wallerian degeneration distal to the injury. The identified loss of motor neurons supports a hypothesis that the disproportionate upper extremity dysfunction in central cord syndrome may be due to injury involving the large fibers of the lateral corticospinal tract,11 and suggests that the corticospinal tracts may be disproportionately involved in upper, relative to lower, extremity function. The patient presenting with new-onset neurological deficit is in neurological and physiological extremis. Standard trauma protocols should be followed, first securing the airway, and then supporting respiratory and cardiovascular status. Initial trauma films should be obtained as per institutional protocols. Particularly in the older patient with significant spondylosis, a high index of suspicion should be maintained for possible fracture, and there should be a low threshold for obtaining advanced imaging studies. Adequate imaging of the cervical spine is crucial, including the C7– T1 junction. Depending on the mechanism of injury and associated clinical suspicion, one should also consider obtaining imaging studies of the thoracic and lumbar spine because noncontiguous injuries in the cervical spine or cervicothoracic junction have been identified in up to 28% of patients with cervical spine trauma.13,14 In the setting of a neurological deficit or suspicion of diskoligamentous injury, a magnetic resonance imaging (MRI) scan should be obtained of the appropriate spinal regions. Any area of clinical suspicion or where fracture or dislocation cannot be excluded with x-ray studies should be considered for evaluation with computed tomographic (CT) imaging. In the older patient presenting with a neurological deficit in the setting of advanced degenerative spondylosis, the clinician should maintain a high index of suspicion for an extension/distraction injury.15 Soft-tissue swelling in the prevertebral space or distraction in a spondylitic disk space is suggestive of a possible extension/distraction mechanism, and MRI should be considered to further evaluate the anterior soft tissues and diskoligamentous complex.15 At the time of presentation to the physician, the primary injury has occurred, and the goal of management is to mitigate the secondary injury cascade and to provide physiological support that maximizes the potential for recovery. Paramount to this goal is the maintenance of adequate perfusion pressures. One should consider prompt placement of an arterial line at the time of initial evaluation to facilitate the maintenance of the mean arterial pressure; a central line may need to be considered if there is concern about cardiovascular instability or the possible need for pressors to maintain central perfusion. As will be discussed, there is significant controversy regarding the role and timing of surgical decompression of any compressive pathology. The rationale for decompression and the debate regarding the timing of decompression are based in part on mitigating the ischemic insult due to vascular compromise. Maintaining spinal cord perfusion pressures is readily accomplished in the trauma bay with medical management and monitoring; constant attention to the mean arterial pressure should be stressed. The clinician should also be aware of the possibility of spinal shock in the setting of a significant SCI and maintain it16 in the differential diagnosis of any hemodynamic instability. The role of steroids in the acute SCI patient is controversial,17–19 and there is no clear consensus. Steroids may be considered as a management option if the patient meets appropriate National Acute Spinal Cord Injury Study (NASCIS) inclusion criteria, but the physician must also consider patient-specific factors when weighing the potential comorbidities of high-dose steroid treatment. Management strategy is dictated, in large part, by the injury mechanism. A high-energy injury in a younger patient population is more likely to present with a fracture or dislocation, with spinal cord compression in the setting of mechanical instability. In this scenario, the surgical management will be aimed at restoring spinal stability, with a concomitant decompression of the neural elements, and in the setting of traumatic fracture-dislocation with neural element compression, the spine should be decompressed and stabilized as expeditiously as possible given patient-specific factors; closed reduction may be a management option to facilitate rapid decompression. The role of closed reduction for specific fracture types is beyond the scope of this chapter, but it is mentioned to stress that, although central cord syndrome is typically discussed as a separate entity in cervical spine trauma, a central cord presentation in the setting of a fracture-dislocation should be managed as appropriate for the given injury mechanism. The elderly patient presenting after a relatively low-energy hyperextension mechanism, such as a fall from standing, without a fracture is the more classic presentation of a central cord syndrome. As is discussed in this chapter, there is considerable controversy regarding the role and timing of surgical decompression in this patient population. This is due in part to the fact that the natural history of central cord syndrome is one of relatively significant motor improvement. Several treatment algorithms19 advocate for observation during this phase of improvement, with intervention only if there is a plateau in improvement or a neurological decline. This creates a selection bias in the literature because patients historically operated on as the initial treatment are those that had a more severe neurological injury, failure to improve, or new deterioration; given that the most important predictor of neurological outcome is initial neurological status, this may bias against positive outcomes in the historical operative cohorts. The literature regarding clinical outcomes of central cord syndrome is diverse. Although it is generally thought that patients with central cord syndrome have a reasonable prognosis for some degree of recovery, the majority of published studies are Class III data with differing outcomes measures.20 The single greatest prognostic indicator of final neurological outcome is the initial neurological status. As reviewed by Dvorak et al., other prognostic variables described have included patient age, spasticity, and hyperpathia.20 However, the majority of published studies have not linked given outcome indices to generic health-related quality of life (HRQoL). Although many patients with central cord syndrome have improvement in their motor function, improvement of motor function has been correlated with increased spasticity,20 and spasticity negatively correlates with functional status21,22 and HRQoL.20 Dvorak et al.20 utilized a prospectively collected database to analyze American Spinal Injury Association (ASIA) motor scores at the time of injury and at follow-up, and they evaluated the short form (SF)-36 and the Functional Independence Measure (FIM) at follow-up. Level of education was found to directly correlate with HRQoL and motor recovery, and spasticity was found to correlate with degree of motor recovery. The degree of spasticity was confirmed to adversely affect outcome measures, and age was found to adversely affect the FIM. Aito et al.23 similarly found that age > 65 was a negative prognostic factor for recovery but did not find any correlation between patient age and bladder function or spasticity; spasticity developed in 54% of patients in Aito et al.’s cohort; Perkash24 reported a 48% incidence of spasticity. A 37-year-old male with acquired and congenital cervical stenosis incurred a hyperextension injury due to a fall. At the time of presentation, the patient had an incomplete spinal cord injury, and was classified as ASIA C (Fig. 27.1 and 27.2). Due to the patient’s neurologic status in the setting of neural element compression, it was elected to perform a posterior cervical decompression and fusion procedure (Fig. 27.3). The issue of the acute management of SCI is controversial, particularly with respect to traumatic central cord syndrome (TCCS). To date, the majority of published studies on the timing of surgical decompression of SCI have been retrospective, level III evidence. There is wide variation in the definition of early versus late decompression in the literature. Ethical considerations pose a considerable challenge to the design and execution of a prospective randomized trial. The Surgical Treatment for Acute Spinal Cord Injury Study (STASCIS) outcomes suggest that there may be a significant benefit to neurological outcome with early (within 24 hours) decompression; patients that were decompressed early (mean 14.2 hours) had odds of improving at least 2 AIS grades that were 2.8 times higher than patients that were decompressed later (mean 48.3 hours).25 The management of TCCS is perhaps more complicated than other aspects of SCI because some authors consider it separately from other cervical SCI, and in fact, some authors have specifically excluded the condition when reporting their cohorts.26 Central cord syndrome occurs more commonly in an older population, which has an associated higher incidence of medical comorbidities to consider in treatment.27 Fig. 27.1 Sagittal magnetic resonance imaging (short tau inversion recovery) and CT reconstruction of the cervical spine of a 37-year-old male with congenital and acquired cervical stenosis who fell, striking his head, with a resulting hyperextension injury. Note the posterior osteophytes at C3–4 and C4–5, and the significant cord edema from C3–6. The patient presented as an incomplete spinal cord injury (American Spinal Injury Association C).
Management of Central Cord Syndrome
 Spinal Cord Injury Epidemiology
Spinal Cord Injury Epidemiology
 Central Cord Syndrome: Definition, Mechanism, Pathophysiology
Central Cord Syndrome: Definition, Mechanism, Pathophysiology
 Initial Evaluation and Management Strategies
Initial Evaluation and Management Strategies
 Prognostic Factors for Clinical Outcome
Prognostic Factors for Clinical Outcome
 Case Example
Case Example
 Management Controversies
Management Controversies
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


