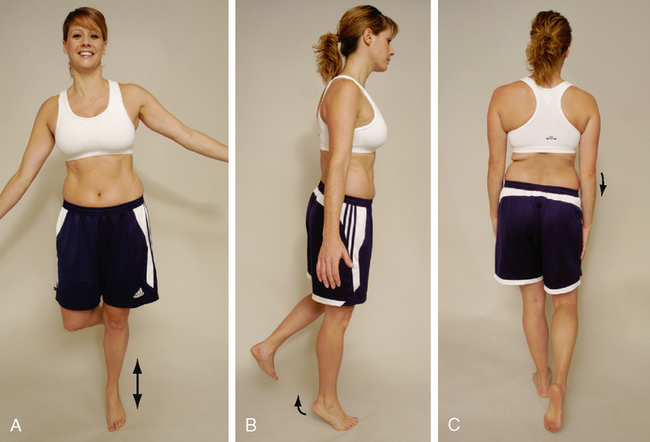
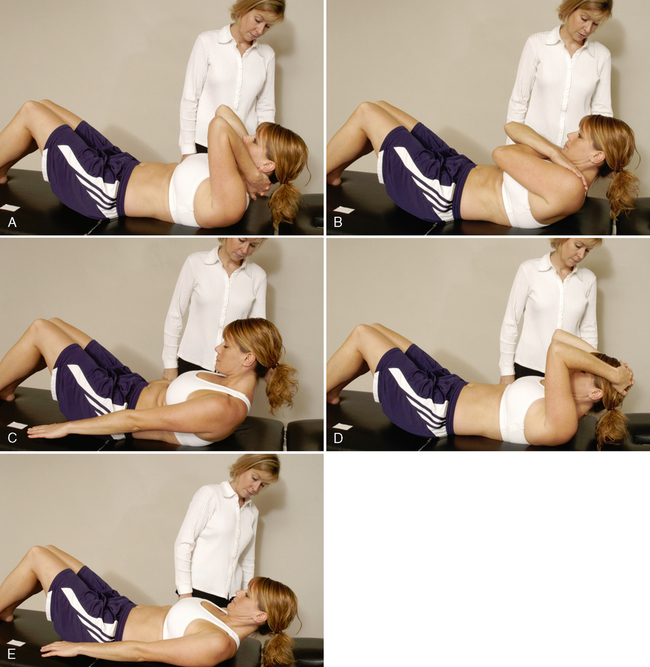
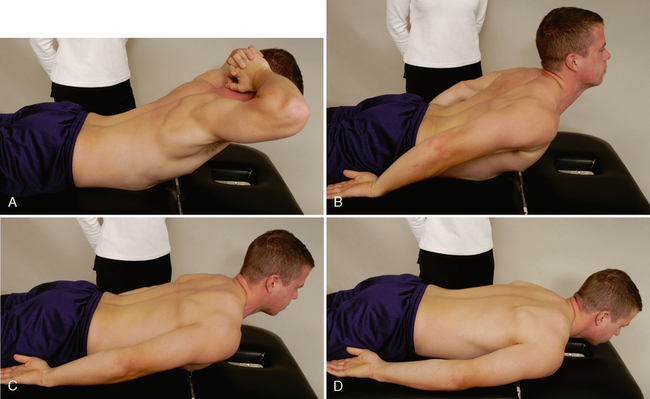
CHAPTER 8 Précis of the Lumbar Spine Assessment* Passive movements (only with care and caution) Peripheral joint scan (standing) Resisted isometric movements (sitting) Resisted isometric movements (supine lying) Dynamic abdominal endurance test Internal/external abdominal obliques test Dynamic horizontal side support (side bridge or side plank) test Peripheral joint scan (supine lying) Hip joints (flexion, abduction, adduction, and medial and lateral rotation) Knee joints (flexion and extension) Ankle joints (dorsiflexion and plantar flexion) Foot joints (supination, pronation) Reflexes and cutaneous distribution (anterior and side aspects) Resisted isometric movements (side lying) Joint play movements (side lying) Peripheral joint scan (prone lying) Resisted isometric movements (prone lying) Reflexes and cutaneous distribution (prone lying) Reflexes and cutaneous distribution (posterior aspect) Joint play movements (prone lying) Posterior-anterior central vertebral pressure (PACVP) Posterior-anterior unilateral vertebral pressure (PAUVP) Resisted isometric movements (quadriped position) *The assessment is shown in an order that limits the amount of movement the patient must do but ensures that all necessary structures are tested. After any assessment, the patient should be warned that symptoms may be exacerbated by the assessment. McKenzie1 recommended repeating the active movements, especially flexion and extension, 10 times to see whether the movement increases or decreases the symptoms. • On forward flexion, the lumbar spine should move from its normal lordotic curvature to at least a straight or slightly flexed curve. If this change does not occur, some hypomobility probably is present in the lumbar spine either from tight structures or muscle spasm. • In a patient with no back pain, when returning to the upright posture from forward flexion, the person first rotates the hips and pelvis to about 45° of flexion; during the last 45° of extension, the low back resumes its lordosis. • In a patient with back pain, most movement usually occurs in the hips, accompanied by knee flexion; in some cases, the patient also uses hand support, working up the thighs. • The examiner must differentiate the movement that occurs in the lumbar spine from that occurring in the hips or thoracic spine. Some patients can touch their toes by flexing the hips, even if no movement occurs in the spine. The degree of injury also has an effect. For example, the more severely a disc is injured (e.g., if sequestration has occurred rather than a protrusion), the greater is the limitation of movement. • Often, an “instability jog” may be seen during one or more movements, especially flexion, returning to neutral from flexion, or side flexion. An instability jog is a sudden movement shift or rippling of the muscles during active movement, which indicates an unstable segment. • Similarly, muscle twitching during movement or complaints of something “slipping out” during lumbar spine movement may indicate instability. • If the patient bends one or both knees on forward flexion, the examiner should watch for nerve root symptoms or tight hamstrings, especially if spinal flexion is decreased when the knees are straight. INDICATIONS OF A POSITIVE TEST Extension (backward bending) normally is limited to 20° to 35° in the lumbar spine. • Bourdillon and Day2 recommend having the patient do this movement in the prone-lying position to hyperextend the spine. They called the resulting position the “sphinx position.” The patient hyperextends the spine by resting on the elbows with the hands holding the chin and allows the abdominal wall to relax. The position is held for 10 to 20 seconds to see whether symptoms occur or worsen if already present. • Although the patient usually is in the standing position, rotation may be performed while the patient is sitting to eliminate or decrease pelvic and hip movement. If the patient stands, the examiner must take care to watch for this accessory movement and try to eliminate it by stabilizing the pelvis. • If a movement (e.g., side flexion) toward the painful side increases the symptoms, the lesion is probably intra-articular, because the muscles and ligaments on that side are relaxed. • If a disc protrusion is present and lateral to the nerve root, side flexion to the painful side increases the pain and radicular symptoms on that side. • If a movement (e.g., side flexion) away from the painful side alters the symptoms, the lesion may be articular or muscular in origin, or it may be a disc protrusion medial to the nerve root. • In the spine, the movement of side flexion is a coupled movement with rotation. Because of the position of the lumbar facet joints, side flexion and rotation occur together, although the amount and direction of movement may not be the same. • Patients often deviate into forward flexion instead of remaining in true side flexion. To prevent this, the patient can be cued to run the hand down the back of the thigh instead of the side of the thigh. TRENDELENBURG’S TEST (MODIFIED) • This is, in effect, a modified Trendelenburg’s test. A weak gluteus medius muscle or a coxa vara (abnormal shaft-neck angle of the femur) on the stance leg side may produce a positive sign on the nonstance side. • The examiner should look for patient compensations when completing the test. The most common compensation is trunk side flexion toward the stance leg. The patient side flexes to move his or her center of gravity over the stance leg, thus decreasing the demand on the gluteus medius. Therefore, the test may appear normal because the ilium responds normally, but if the side flexion is corrected, the positive response occurs. ADVANCED RESISTED MOVEMENTS OF THE LUMBAR SPINE Provided neutral resisted isometric testing in sitting is normal or causes only a small amount of pain, the examiner can go on to other tests that place greater stress on the muscles. These tests often are dynamic and provide both concentric and eccentric work for the muscles supporting the spine. With all of the following tests, the examiner should make sure the patient can hold a neutral pelvis before doing that test. If excessive movement of the anterior superior iliac spines (ASISs) (supine) or posterior superior iliac spines (PSISs) (prone) is noted when the patient does any of the movements, the tests should be stopped. In normal individuals, the ASIS or PSIS does not move during these tests. Motivation may also affect the results.3 The patient starts the test in the patient position noted above. The examiner then sequentially asks the patient to move to the end position of each level of testing. The patient is instructed to hold the end position for as long as possible. Testing begins with the Trace Grade and progresses sequentially to the Normal Grade (see Table 8-1). Table 8-1 Isometric Abdominal Test Grading INDICATIONS OF A POSITIVE TEST The number of seconds the patient holds the contraction before cheating (e.g., holding the breath, altered mechanics) or the onset of fatigue is recorded as the manual muscle test (MMT) score. The grading for this isometric abdominal test is described in Table 8-1. RELIABILITY/SPECIFICITY/SENSITIVITY5 Reliability (interrater) ICC = 0.25 DYNAMIC ABDOMINAL ENDURANCE TEST5,8 The patient attempts to extend the spine as far as possible by lifting up the head and trunk. Depending on how the patient does the test (the aim is to get the highest score possible) and how long the position is held (see Table 8-2), the examiner records the MMT score. The patient holds the end position as long as possible. Table 8-2 Isometric Extensor Test Grading INDICATIONS OF A POSITIVE TEST The examiner times how long the patient can hold the extended position. The test is graded as described in Table 8-2. INTERNAL/EXTERNAL ABDOMINAL OBLIQUE TEST6,11 The patient is asked to lift the head and the shoulder on one side and reach over and touch the fingernails of the other hand or to flex and rotate the trunk. Depending on how the patient does the test (the aim is to get the highest score possible) and how long the position is held (see Table 8-3), the examiner records the MMT score. The patient holds the end position as long as possible. The patient’s feet should not be supported, and the patient should breathe normally. Table 8-3 Internal/External Abdominal Oblique Test Grading INDICATIONS OF A POSITIVE TEST The number of seconds the contraction is held before cheating (e.g., holding the breath, altered mechanics) or the onset of fatigue is recorded as the score. The test is graded as described in Table 8-3. DOUBLE STRAIGHT LEG LOWERING TEST6,11–13 INDICATIONS OF A POSITIVE TEST As soon as the examiner feels the ASIS start to rotate forward during the leg lowering, the test is stopped and the examiner holds the patient’s legs in that position while measuring the angle (plinth to thigh angle). The test must be done slowly, and the patient must not hold the breath. The test is graded as described in Table 8-4. Table 8-4 Double Straight Leg Lowering Test Grading • This test should be performed only if the patient receives a grade of “normal” in the dynamic abdominal endurance test or the abdominal isometric test. • This is an abdominal eccentric test that can put a great deal of stress on the spine; therefore, the examiner must make sure the patient is able to hold a neutral pelvis before doing the exercise. If the patient cannot hold neutral spine or if the patient is symptomatic with the test, the test should not be completed. This test also causes greater abdominal activation than curl-ups. DYNAMIC HORIZONTAL SIDE SUPPORT (SIDE BRIDGE OR SIDE PLANK) TEST14,15 INDICATIONS OF A POSITIVE TEST The patient should not roll forward or backward when doing the test. The examiner times how long the patient can hold the position without cheating. The test is graded as described in Table 8-5. Table 8-5 Dynamic Horizontal Side Support (Side Bridge) Test Grading • The test may also be done dynamically, to test endurance, by having the patient repeat the side bridging as many times as possible on each side. • McGill et al.15 reported that the side bridge should be able to be held 65% of the extensor time for men and 39% for women, and 99% of the flexor time for men and 79% for women. The examiner’s position varies, depending on the joint to be scanned.
LUMBAR SPINE

SELECTED MOVEMENTS
![]()
Grade
MMT Score
Patient Position
Normal
5
With the hands clasped behind the neck, able to raise the upper body until the scapulae clear the table (20- to 30-second hold)
Good
4
With the arms crossed over the chest, able to raise the upper body until the scapulae clear the table (15- to 20-second hold)
Fair
3
With the arms straight, able to raise the upper body until the scapulae clear the table (10- to 15-second hold)
Poor
2
With the arms extended toward the knees, able to raise the upper body until the top of the scapulae lift from the table (1- to 10-second hold)
Trace
1
Unable to raise more than the head off the table
![]()

Grade
MMT Score
Patient Position
Normal
5
With the hands clasped behind the head, extends the lumbar spine, lifting the head, chest, and ribs from the bed/floor (20- to 30-second hold)
Good
4
With the hands at the side, extends the lumbar spine, lifting the head, chest, and ribs from the bed/floor (15- to 20-second hold)
Fair
3
With the hands at the side, extends the lumbar spine, lifting the sternum off the bed/floor (10- to 15-second hold)
Poor
2
With the hands at the side, extends the lumbar spine, lifting the head off the bed/floor (1- to 10-second hold)
Trace
1
Only slight contraction of the muscle with no movement
![]()
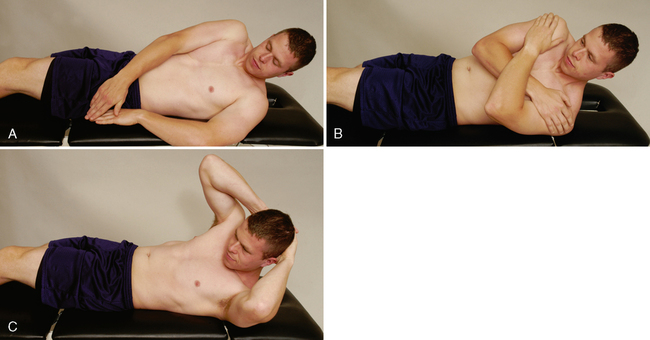
Grade
MMT Score
Patient Position
Normal
5
Flexes and rotates the lumbar spine fully with the hands behind the head (20- to 30-second hold)
Good
4
Flexes and rotates the lumbar spine fully with the hands across the chest (15- to 20-second hold)
Fair
3
Flexes and rotates the lumbar spine fully with the arms reaching forward (10- to 15-second hold)
Poor
2
Unable to flex and rotate fully
Trace
1
Only slight contraction of the muscle with no movement
None
0
No contraction of the muscle
![]()
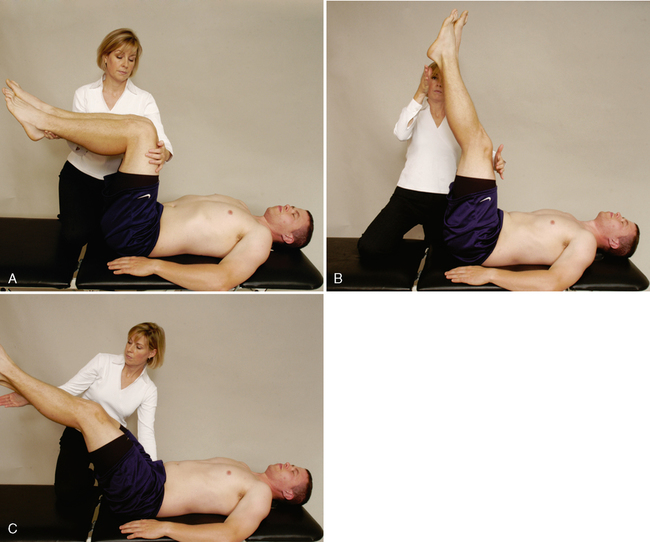
Grade
MMT Score
Patient Position
Normal
5
Able to reach 0° to 15° from the table before the pelvis tilts
Good
4
Able to reach 16° to 45° from the table before the pelvis tilts
Fair
3
Able to reach 46° to 75° from the table before the pelvis tilts
Poor
2
Able to reach 75° to 90° from the table before the pelvis tilts
Trace
1
Unable to hold the pelvis in neutral at all
![]()

Grade
MMT Score
Patient Position
Normal
5
Able to lift the pelvis off the examining table and hold the spine straight (10- to 20-second hold)
Good
4
Able to lift the pelvis off the examining table but has difficulty holding the spine straight (5- to 10-second hold)
Fair
3
Able to lift the pelvis off the examining table but cannot hold the spine straight (<5-second hold)
Poor
2
Unable to lift the pelvis off examining table
PERIPHERAL JOINT SCANNING EXAMINATION