Lumbar Spine
Back pain is one of the great human afflictions. Almost anyone born today in Europe or North America has a great chance of suffering a disabling back injury regardless of occupation.1 The lumbar spine supports the upper body and transmits the weight of the upper body to the pelvis and lower limbs. Because of the strategic location of the lumbar spine, this structure should be included in any examination of the spine as a whole (i.e., posture) or in any examination of the hip or sacroiliac joints. Unless there is a definite history of trauma, determining whether an injury originates in the lumbar spine, sacroiliac joints, or hip joints is often difficult; therefore, all three should be examined in a sequential fashion.
Applied Anatomy
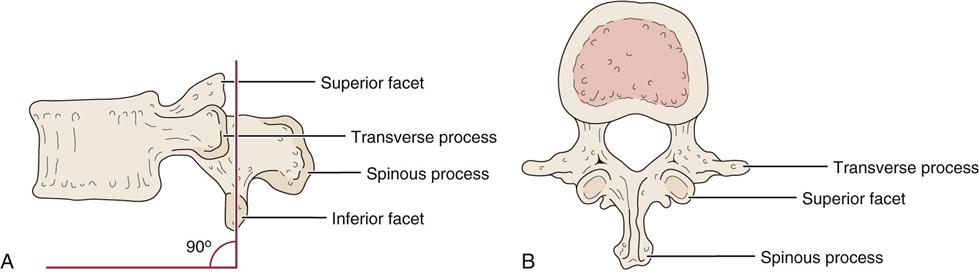
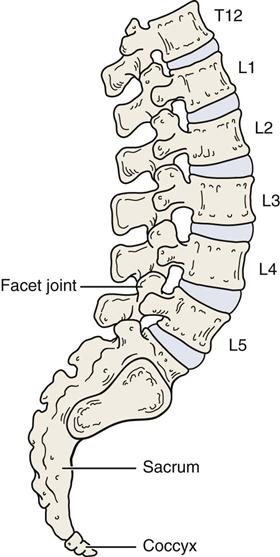
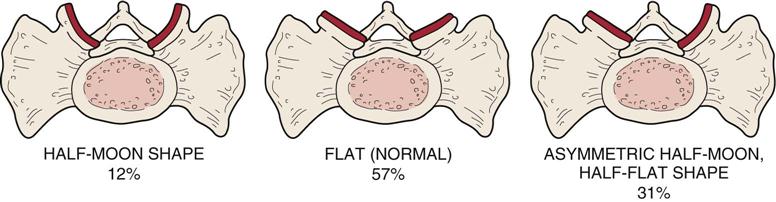
There are ten (five pairs) facet joints (also called apophyseal or zygoapophyseal joints) in the lumbar spine (Figure 9-1).2 These diarthrodial joints consist of superior and inferior facets and a capsule. The facets are located on the vertebral arches. With a normal intact disc, the facet joints carry about 20% to 25% of the axial load, but this may reach 70% with degeneration of the disc. The facet joints also provide 40% of the torsional and shear strength.3 Injury, degeneration, or trauma to the motion segment (the facet joints and disc) may lead to spondylosis4 (degeneration of the intervertebral disc), spondylolysis5 (a defect in the pars interarticularis or the arch of the vertebra), spondylolisthesis5 (a forward displacement of one vertebra over another), or retrolisthesis (backward displacement of one vertebra on another). The superior facets, or articular processes, face medially and backward and, in general, are concave; the inferior facets face laterally and forward and are convex (Figure 9-2). There are, however, abnormalities, or tropisms, that can occur in the shape of the facets, especially at the L5–S1 level (Figures 9-3 and 9-4).6 In the lumbar spine, the transverse processes are virtually at the same level as the spinous processes.
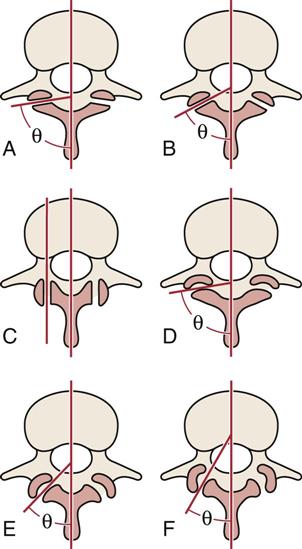
A, Flat joints oriented close to 90° to the sagittal plane. B, Flat joints orientated at 60° to the sagittal plane. C, Flat joints orientated parallel (0°) to the sagittal plane. D, Slightly curved joints with an average orientation close to 90° to the sagittal plane. E, “C”-shaped joints orientated at 45° to the sagittal plane. F, “J”-shaped joints orientated at 30° to the sagittal plane. (Redrawn from Bogduk N, Twomey LT: Clinical anatomy of the lumbar spine, New York, 1987, Churchill Livingstone, p. 26.)
These posterior facet joints direct the movement that occurs in the lumbar spine. Because of the shape of the facets, rotation in the lumbar spine is minimal and is accomplished only by a shearing force. Side flexion, extension, and flexion can occur in the lumbar spine, but the facet joints control the direction of movement. The close packed position of the facet joints in the lumbar spine is extension. Normally, the facet joints carry only a small amount of weight; however, with increased extension, they begin to have a greater weight-bearing function. The resting position is midway between flexion and extension. The capsular pattern is side flexion and rotation equally limited, followed by extension. However, if only one facet joint in the lumbar spine has a capsular restriction, the amount of observable restriction is minimal. The first sacral segment is usually included in discussions of the lumbar spine, and it is at this joint that the fixed segment of the sacrum joins with the mobile segments of the lumbar spine. In some cases, the S1 segment may be mobile. This occurrence is called lumbarization of S1, and it results in a sixth “lumbar” vertebra. At other times, the fifth lumbar segment may be fused to the sacrum or ilium, resulting in a sacralization of that vertebra. Sacralization results in four mobile lumbar vertebrae. These abnormalities are sometimes called transitional vertebra.7
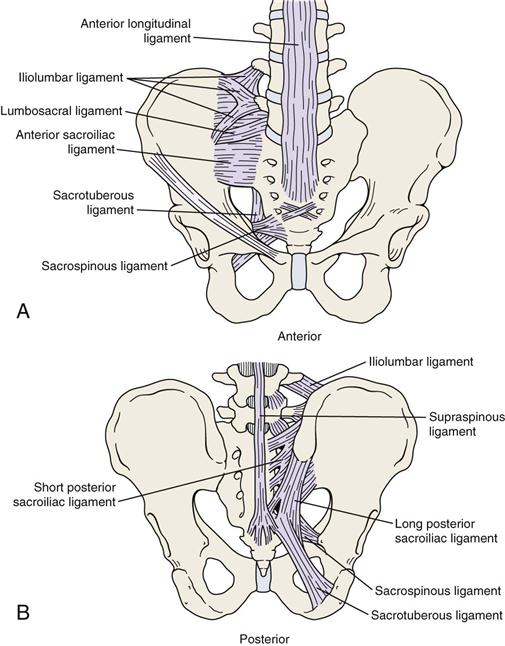
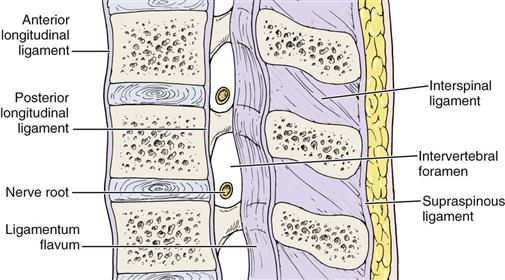
The main ligaments of the lumbar spine are the same as those in the lower cervical and thoracic spine (excluding the ribs). These ligaments include the anterior and posterior longitudinal ligaments, the ligamentum flavum, the supraspinous and interspinous ligaments, and the intertransverse ligaments (Figure 9-5). In addition, there is an important ligament unique to the lumbar spine and pelvis—the iliolumbar ligament (Figure 9-6), which connects the transverse process of L5 to the posterior ilium.8 This ligament helps stabilize L5 with the ilium and helps prevent anterior displacement of L5.9
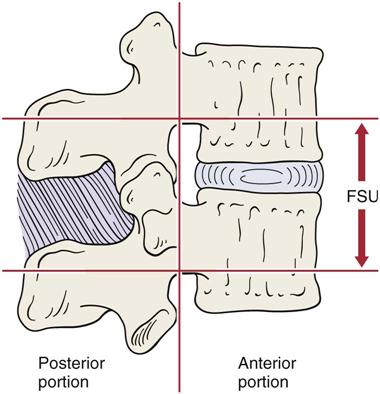
The intervertebral discs make up approximately 20% to 25% of the total length of the vertebral column. The function of the intervertebral disc is to act as a shock absorber distributing and absorbing some of the load applied to the spine, to hold the vertebrae together and allow movement between the bones, to separate the vertebra as part of a functional segmental unit acting in concert with the facet joints (Figure 9-7), and, by separating the vertebrae, to allow the free passage of the nerve roots out from the spinal cord through the intervertebral foramina. With age, the percentage of spinal length attributable to the discs decreases as a result of disc degeneration and loss of hydrophilic action in the disc.
Such a complex may also be seen in the cervical and thoracic spines.
The annulus fibrosus, the outer laminated portion of the disc, consists of three zones: 1) an outer zone made up of fibrocartilage (classified as Sharpey fibers) that attaches to the outer or peripheral aspect of the vertebral body and contains increasing numbers of cartilage cells in the fibrous strands with increasing depth, 2) an intermediate zone made up of another layer of fibrocartilage, and 3) an inner zone primarily made up of fibrocartilage and containing the largest number of cartilage cells.10 The annulus fibrosus contains twenty concentric, collar-like rings of collagenous fibers that crisscross each other to increase their strength and accommodate torsion movements.11
The nucleus pulposus is well developed in both the cervical and the lumbar spines. At birth, it is made up of a hydrophilic mucoid tissue, which is gradually replaced by fibrocartilage. With increasing age, the nucleus pulposus increasingly resembles the annulus fibrosus. The water-binding capacity of the disc decreases with age, and degenerative changes (spondylosis) begin to occur after the second decade of life. Initially, the disc contains approximately 85% to 90% water, but the amount decreases to 65% with age.12 In addition, the disc contains a high proportion of mucopolysaccharides, which cause the disc to act as an incompressible fluid. However, these mucopolysaccharides decrease with age and are replaced with collagen. The nucleus pulposus lies slightly posterior to the center of rotation of the disc in the lumbar spine.
The shape of the disc corresponds to that of the body to which it is attached. The disc adheres to the vertebral body by means of the cartilaginous end plate. The end plates consist of thin layers of cartilage covering the majority of the inferior and superior surfaces of the vertebral body. The cartilaginous end plates are approximately 1 mm thick and allow fluid to move between the disc and the vertebral body. The discs are primarily avascular with only the periphery receiving a blood supply. The remainder of the disc receives nutrition by diffusion, primarily through the cartilaginous end plate. Until the age of 8 years, the intervertebral discs have some vascularity; however, with age this vascularity decreases.
Usually, the intervertebral disc has no nerve supply, although the peripheral posterior aspect of the annulus fibrosus may be innervated by a few nerve fibers from the sinuvertebral nerve.13,14 The lateral aspects of the disc are innervated peripherally by the branches of the anterior rami and gray rami communicants. The pain-sensitive structures around the intervertebral disc are the anterior longitudinal ligament, posterior longitudinal ligament, vertebral body, nerve root, and cartilage of the facet joint.
With the movement of fluid vertically through the cartilaginous end plate, the pressure on the disc decreases as the patient assumes the natural lordotic posture in the lumbar spine. Direct vertical pressure on the disc can cause the disc to push fluid into the vertebral body. If the pressure is great enough, defects may occur in the cartilaginous end plate, resulting in Schmorl nodules, which are herniations of the nucleus pulposus into the vertebral body. These are found in 20% to 30% of individuals.15 Normally, an adult is 1 to 2 cm (0.4 to 0.8 inch) taller in the morning than in the evening (20% diurnal variation).3,16 This change results from fluid movement in and out of the disc during the day through the cartilaginous end plate. This fluid shift acts as a pressure safety valve to protect the disc.
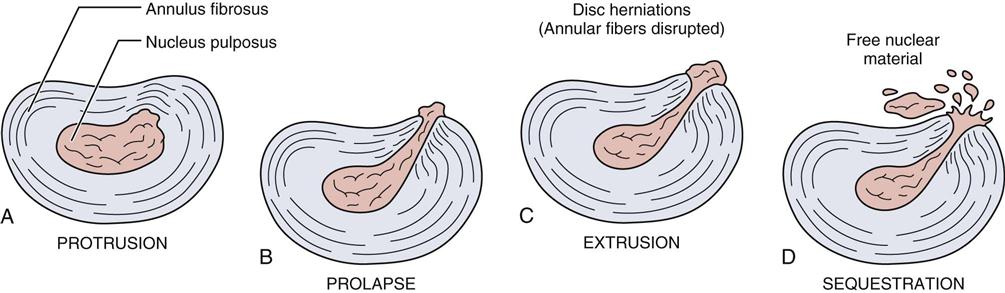
If there is an injury to the disc, four problems can result, all of which can cause symptoms.17 There may be a protrusion of the disc, in which the disc bulges posteriorly without rupture of the annulus fibrosus. In the case of a disc prolapse, only the outermost fibers of the annulus fibrosus contain the nucleus. With a disc extrusion, the annulus fibrosus is perforated, and discal material (part of the nucleus pulposus) moves into the epidural space. The fourth problem is a sequestrated disc, or a formation of discal fragments from the annulus fibrosus and nucleus pulposus outside the disc proper (Figure 9-8).18 These injuries can result in pressure on the spinal cord itself (upper lumbar spine) leading to a myelopathy, pressure on the cauda equina leading to cauda equina syndrome (saddle anesthesia [Figure 9-9], bowel/bladder dysfunction),19 or pressure on the nerve roots (most common). The amount of pressure on the neurological tissues determines the severity of the neurological deficit.20 The pressure may be the result of the disc injury itself or in combination with the inflammatory response of the injury. Saal has outlined favorable, unfavorable, and neutral factors for positive-outcome prognostic factors for nonoperative lumbar disc herniation (Table 9-1).17
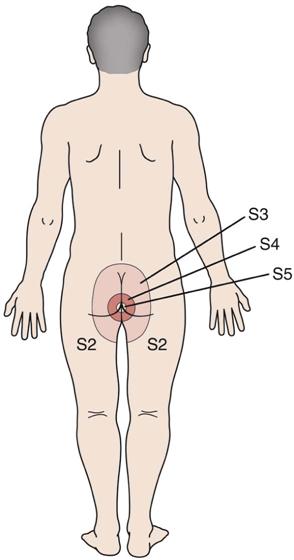
The S3, S4, and S5 nerves provide sensory innervation to the inner thigh, perineum, and rectum.
TABLE 9-1
Prognostic Factors for Positive Outcome with Nonoperative Care for Lumbar Disc Herniation
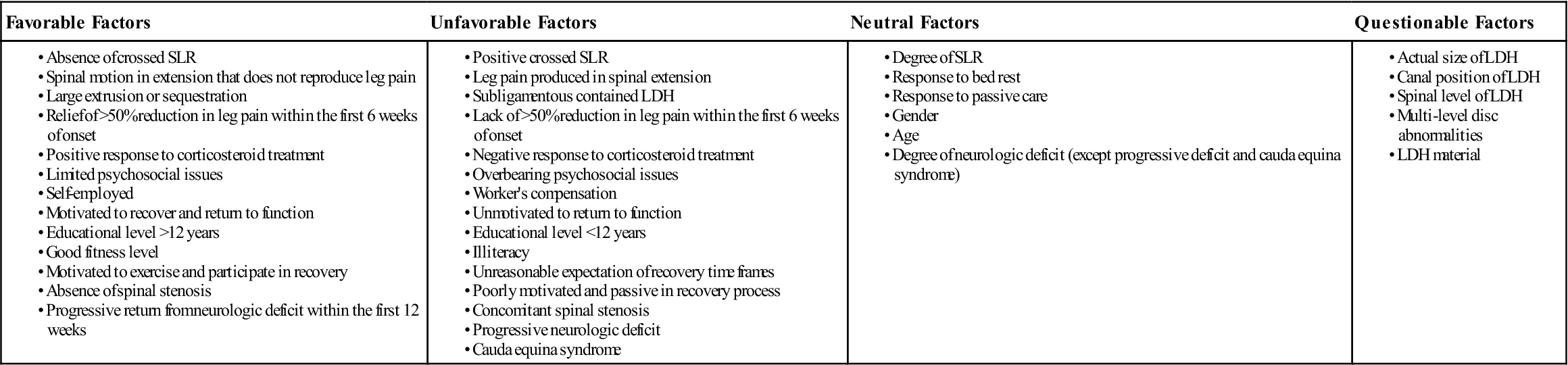
LDH, Lumbar disc herniation; SLR, straight leg raise.
Modified from Saal JA: Natural history and nonoperative treatment of lumbar disc herniation. Spine 21(24S):7S, 1996.
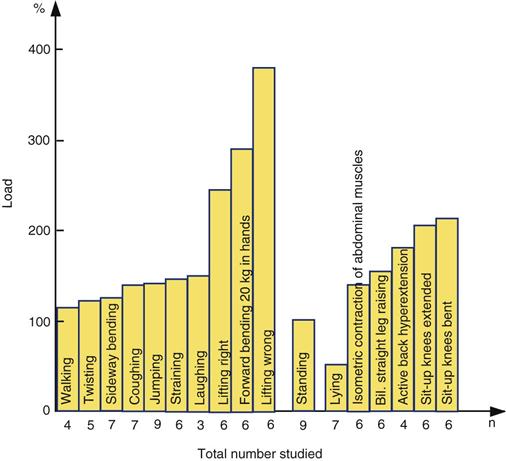
Within the lumbar spine, different postures can increase the pressure on the intervertebral disc (Figure 9-10). This information is based on the work of Nachemson and colleagues,21,22 who performed studies of intradiscal pressure changes in the L3 disc with changes in posture. The pressure in the standing position is classified as the norm, and the values given are increases or decreases above or below this norm that occur with the change in posture.
In the lumbar spine, the nerve roots exit through relatively large intervertebral foramina, and as in the thoracic spine, each one is named for the vertebra above it (in the cervical spine, the nerve roots are named for the vertebra below). For example, the L4 nerve root exits between the L4 and L5 vertebrae. Because of the course of the nerve root as it exits, the L4 disc (between L4 and L5) only rarely compresses the L4 nerve root; it is more likely to compress the L5 nerve root (Figure 9-11).
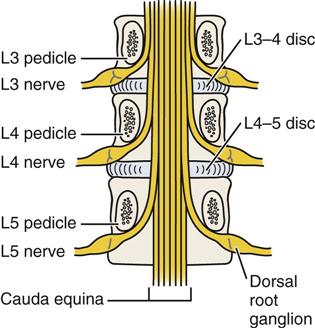
Note that the exiting root takes the name of the vertebral body under which it travels into the neural foramen. Because of the way the nerve roots exit, L4–L5 disc pathology usually affects the L5 root rather than the L4 root. (Redrawn from Borenstein DG, Wiesel SW, Boden SD: Low back pain: medical diagnosis and comprehensive management, Philadelphia, 1995, WB Saunders, p. 5.)
In general, the L5–S1 segment is the most common site of problems in the vertebral column because this level bears more weight than any other vertebral level. The center of gravity passes directly through this vertebra, which is of benefit because it may decrease the shearing stresses to this segment. There is a transition from the mobile segment, L5, to the stable or fixed segment of the sacrum (S1), which can increase the stress on this area. Because the angle between L5 and S1 is greater than those between the other vertebrae, this joint has a greater chance of having stress applied to it. Another factor that increases the amount of stress on this area is the relatively greater amount of movement that occurs at this level compared with other levels of the lumbar spine.
Patient History
Problems of the lumbar spine are difficult to diagnose; in fact, diagnosing pain due to a disc is primarily diagnosis of exclusion.23 Most of the examination commonly revolves around differentiating symptoms of a herniated disc (or space occupying lesion), which refers radicular symptoms into the leg from other conditions (e.g., inflammatory reaction, sprains, strains, facet syndrome) more likely to cause localized pain.24 If there are no radicular symptoms below the knee, it often becomes difficult for the examiner to determine where in the spine the problem is, or for that matter, whether the problem is truly in the lumbar spine or coming from problems in the pelvic joints, primarily the sacroiliac joints, or the hips. Waddell pointed out that in only about 15% of cases can a definitive diagnosis as to the pathology of back pain be made.3 Hall broke low back pain into four categories—two of which are back pain dominant and two of which are leg pain dominant (Table 9-2).25 Pattern 1 suggests disc involvement, whereas pattern 2 suggests facet joint involvement. Pattern 3 suggests nerve root involvement (primarily by a disc or some other space occupying lesion or an injury accompanied by inflammatory swelling), and pattern 4 suggests neurogenic intermittent claudication (pressure on the cauda equina). Thus, only by taking a careful history, followed by a detailed examination, is the examiner able to determine the cause of the problem.26–28 Even then, some doubt may remain.
TABLE 9-2
| Pattern | Where Pain Is Worst | Aggravating Movement | Relieving Movement | Onset | Duration | Probable Cause | |
| Back Dominant Pain/Mechanical Cause | 1 | Back/buttocks (>90% back pain) Myotomes seldom affected Dermatomes not affected | Flexion Stiff in morning | Extension | Hours to days | Days to months (sudden or slow) | Disc involvement (minor herniation, spondylosis), sprain, strain |
| 2 | Back/buttocks Myotomes seldom affected Dermatomes not affected | Extension/Rotation | Flexion | Minutes to hours | Days to weeks (sudden) | Facet joint involvement, strain | |
| Leg Pain Dominant/Nonmechanical Cause | 3 | Leg (usually below knee) Myotomes commonly affected (especially in chronic cases) Pain in dermatomes | Flexion | Extension | Hours to Days | Weeks to months | Nerve root irritation (most likely cause—disc hernation) |
| 4 | Leg (usually below knee) (May be bilateral) Myotomes commonly affected (especially in chronic cases) Pain in dermatomes | Walking (extension) | Rest (sitting) and/or postural change | With walking | ? | Neurogenic intermittent claudication (stenosis) |
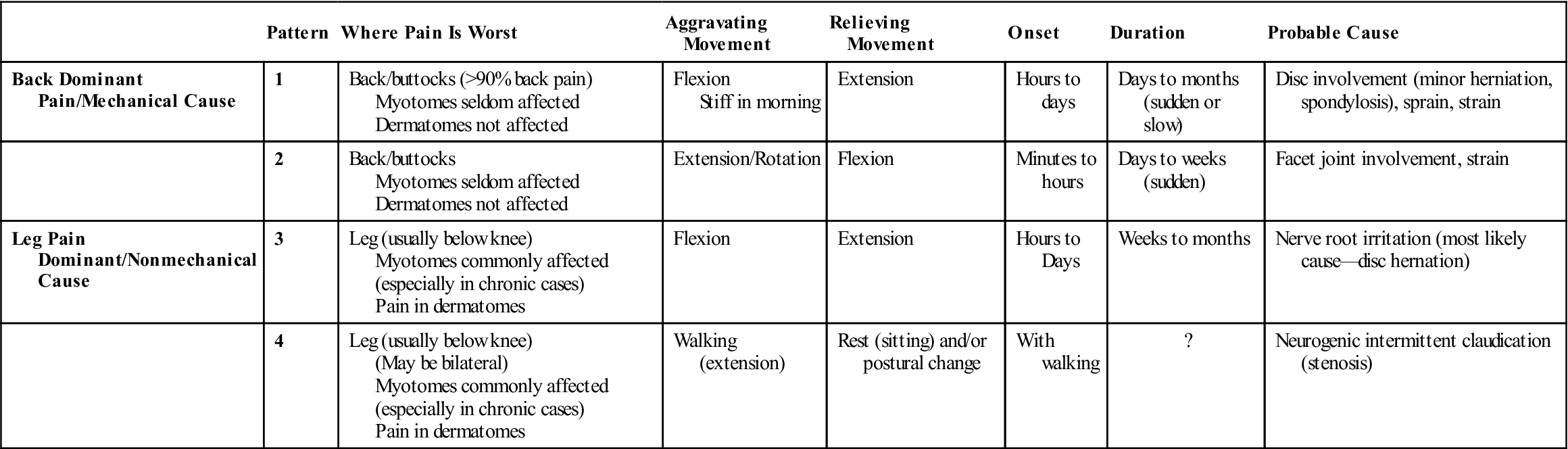
Modified from Hall H: A simple approach to back pain management. Patient Care 15:77–91, 1992.
In addition to the questions listed under the “Patient History” section in Chapter 1, the examiner should obtain the following information from the patient:
1. What is the patient’s age?29 Different conditions affect patients at different ages. For example, disc problems usually occur between the ages of 15 and 40 years, and ankylosing spondylitis is evident between 18 and 45 years. Osteoarthritis and spondylosis are more evident in people older than 45 years of age, and malignancy of the spine is most common in people older than 50 years of age.
2. What is the patient’s occupation?3,30 Back pain tends to be more prevalent in people with strenuous occupations,31 although it has been reported that familial influences have an effect as well as occupation.32,33 For example, truck drivers (vibration) and warehouse workers have a high incidence of back injury.34 Patients who have chronic low back pain develop a deconditioning syndrome, which compounds the problem as it leads to decreased muscle strength, impaired motor control, and decreased coordination and postural control.35 How active is the patient at work (usual job, light duties, full time, frequent days off because of back pain, unemployed because of back, retired)?
4. What was the mechanism of injury? Was major trauma (e.g., car accident) involved? Lifting commonly causes low back pain (Tables 9-3 and 9-4). This is not surprising when one considers the forces exerted on the lumbar spine and disc. For example, a 77-kg (170-lb) man lifting a 91-kg (200-lb) weight approximately 36 cm (14 inches) from the intervertebral disc exerts a force of 940 kg (2072 lbs) on that disc. The force exerted on the disc can be calculated as roughly ten times the weight being lifted. Pressure on the intervertebral discs varies depending on the position of the spine. Nachemson and colleagues showed that pressure on the disc can be decreased by increasing the supported inclination of the back rest (e.g., an angle of 130° decreases the pressure on the disc by 50%).21,22 Using the arms for support can also decrease the pressure on the disc. When one is standing, the disc pressure is approximately 35% of the pressure that occurs in the relaxed sitting position. The examiner should also keep in mind that stress on the lower back tends to be 15% to 20% higher in men than in women because men are taller and their weight is distributed higher in the body.
5. How long has the problem bothered the patient? Acute back pain lasts 3 to 4 weeks. Subacute back pain lasts up to 12 weeks. Chronic pain is anything longer than 3 months. Waddell has outlined predictors (yellow flags) of chronicity with back pain patients.3,36
6. Where are the sites and boundaries of pain? Have the patient point to the location or locations. Note whether the patient indicates a specific joint or whether the pain is more general. The more specific the pain, the easier it is to localize the area of pathology. Unilateral pain with no referral below the knee may be caused by injury to muscles (strain) or ligaments (sprain), the facet joint, or, in some cases, the sacroiliac joints. This is called mechanical low back pain (in older books it is called “lumbago”). With each of these injuries, there is seldom if ever peripheralization of the symptoms. The symptoms tend to stay centralized in the back. If the muscles and ligaments are affected, movement will decrease and pain will increase with repeated movements. If the pain extends to the hip, the hip must be cleared by examination. With facet joint problems, the range of motion (ROM) remains the same (it may be restricted from the beginning), as does the pain with repeated movements. Pain on standing that improves with walking and pain on forward flexion with no substantial muscle tenderness suggests disc involvement.37 The sacroiliac joints will show pain when pain-provoking (stress) tests are used. A minor disc injury (protrusion) may show the same symptoms, but the pain is more likely to be bilateral if it is a central protrusion.38
7. Is there any radiation of pain? Is the pain centralizing or peripheralizing (Figure 9-12)?39,40 Centralization implies the pain is moving toward or is centered in the lumbar spine.41–43 Peripheralization implies the pain is being referred or is moving into the limb. If so, it is helpful for the examiner to remember and correlate this information with dermatome findings when evaluating sensation. The examiner must be careful when looking at the lumbar spine that he or she does not consider every back problem a disc problem. It has been reported that disc problems account for only about 5% of low back pain cases.44 Some authors feel the only definitive clinical diagnosis of a disc problem is neurological pain extending below the knee.25 This means that although there may be pain in the back and in the leg, the leg pain is dominant.3 Pain on the anterolateral aspect of the leg is highly suggestive of L4 disc problems, whereas pain radiating to the posterior aspect of the foot suggests L5 disc problems if the history indicates a disc may be injured.45 Pain radiating into the leg below the knee is highly suggestive of a disc lesion, but isolated back or buttock pain does not rule out the disc. Minor injuries, such as protrusion of the disc, may result only in back or buttock pain.45 Such an injury makes diagnoses more difficult because such pain may also result from muscle or ligament injury or from injury or degeneration to the adjacent facet joints.
Lumbar and sacroiliac pain tend to be referred to the buttock and posterior leg (and sometimes to the lateral aspect of the leg). Hip pain tends to be in the groin and anterior thigh although it may be referred to the knee (usually medial side). The hip can be ruled out later in the examination by the absence of a hip capsular pattern and a negative sign of the buttock.46 The examiner must also determine whether the musculoskeletal system is involved or whether the pain is being referred from another structure or system (e.g., abdominal organs). Abnormal signs and symptoms or red flags (see Table 1-1) would lead the examiner to consider causes other than the musculoskeletal system.
11. Are there any postures or actions that specifically increase or decrease the pain or cause difficulty?39,47 For example, if sitting increases the pain and other symptoms, the examiner may suspect that sustained flexion is causing mechanical deformation of the spine or increasing the intradiscal pressure.48 Classically, disc pathology causes increased pain on sitting, lifting, twisting, and bending.49 It is the most common space-occupying lesion in the lumbar spine and, therefore, is the most common cause of radiating pain below the knee. If standing increases the pain and other symptoms, the examiner may suspect that extension, especially relaxed standing, is the cause. If walking increases the pain and other symptoms, extension is probably causing the mechanical deformation, because walking accentuates extension. If lying (especially prone lying) increases the pain and other symptoms, extension may be the cause. Persistent pain or progressive increases in pain while the patient is in the supine position may lead the examiner to suspect neurogenic or space-occupying lesions, such as an infection, swelling, or tumor. Remember that pain may radiate to the lumbar spine from pathological conditions in other areas as well as from direct mechanical problems. For example, tumors of the pancreas refer pain to the low back. Stiffness or pain after rest may indicate ankylosing spondylitis or Scheuermann disease. Pain from mechanical breakdown tends to increase with activity and decrease with rest. Discogenic pain increases if the patient maintains a single posture (especially flexion) for a long period. Pain arising from the spine almost always is influenced by posture and movement.
The pelvis is the key to proper back posture. Ideally, an individual should be able to stand with the pelvis in neutral. In this position, the anterior superior iliac spines (ASISs) are one to two finger widths lower than the posterior superior iliac spines (PSISs). For the pelvis to “sit” properly on the femora, the abdominal, hip flexor, hip extensor, and back extensor muscles must be strong, supple, and “balanced” (Figure 9-13). Any deviation in the normal alignment should be noted and recorded. For example, shoe heel height can modify the pelvic angle and lumbar curve, altering the stress on the spine.50
13. Which movements hurt? Which movements are stiff? Table 9-5 demonstrates some of the causes of mechanical low back pain and their symptoms. The examiner must help the patient differentiate between true pain and discomfort that is caused by stretching. Postural, or static, muscles (e.g., iliopsoas) tend to respond to pathology with tightness in the form of spasm or adaptive shortening; dynamic, or phasic, muscles (e.g., abdominals) tend to respond with atrophy. Pathology affecting both types of muscles can lead to a pelvic crossed syndrome (discussed later). Does the patient describe a painful arc of movement on forward or side flexion? If so, it may indicate a disc protrusion with a nerve root riding over the bulge or instability in part of the ROM.47 Patients with lumbar instability or lumbar muscle spasm have trouble moving to the seated position, whereas patients with discogenic pain usually have pain in flexion (e.g., sitting) and the pain may increase the longer they are seated.
14. Is paresthesia (a “pins and needles” feeling) or anesthesia present? A patient may experience a sensation or a lack of sensation if there is pressure on a nerve root. Paresthesia occurs if pressure is relieved from a nerve trunk, whereas if the pressure is on the nerve trunk, the patient experiences a numb sensation. Does the patient experience any paresthesia or tingling and numbness in the extremities, perineal (saddle) area, or pelvic area? Abnormal sensations in the perineal area often have associated micturition (urination) problems. These symptoms may indicate a myelopathy and are considered by many to be an emergency surgical situation because of potential long-term bowel and bladder problems if the pressure on the spinal cord is not relieved as soon as possible.51,52 The examiner must remember that the adult spinal cord ends at the bottom of the L1 vertebra and becomes the cauda equina within the spinal column. The nerve roots extend in such a way that it is rare for the disc to pinch on the nerve root of the same level. For example, the L5 nerve root is more likely to be compressed by the L4 intervertebral disc than by the L5 intervertebral disc (Figure 9-14). Seldom is the nerve root compressed by the disc at the same level, except when the protrusion is more lateral.
15. Has the patient noticed any weakness or decrease in strength? Has the patient noticed that his/her legs have become weak while walking or climbing stairs? This may be the result of an injury to the muscles themselves, their nerve supply, or reflex inhibition caused by pain.28,53
17. Which activities aggravate the pain? Is there anything in the patient’s lifestyle that increases the pain? Many common positions assumed by patients are similar to those in some of the provocative special tests. For example, getting into and sitting in a car is similar to the slump test and straight leg raise test. Long sitting in bed is a form of straight leg raise. Reaching up into a cupboard can be similar to an upper limb tension test. A word of caution: There can be a 10° to 20° difference in straight leg raise in lying and sitting because of the change in lordosis and position of the pelvis.3
23. Is the patient able to cope during daily activities? Psychosocial issues often play a role in low back pain, especially if it is chronic.54–57 It is normal for people suffering prolonged pain to exhibit altered psychosocial behaviors that are subject to wide individual differences and the effects of learning.58 Fear avoidance questionnaires, especially Waddell, et al.,59 Fear-Avoidance Beliefs Questionnaire (FABQ) (Figure 9-15) and Linton and Hallden’s Acute Low Back Pain Screening Questionnaire60 (Figure 9-16), are becoming more commonly used in lumbar examination.61–67 The New Zealand Acute Low Back Pain Guide outlines yellow flags indicating psychosocial barriers for recovery with questions related to attitudes and beliefs about back pain, behavior, compensation issues, diagnosis and treatment, emotions, family and work.58 These yellow flags should be seen as factors that can be influenced positively to facilitate recovery and reduce work loss and long term disability.58 Haggman, et al.68 felt that two questions were particularly significant to ask the patient to screen for depressive symptoms:1) “During the past month, have you often been bothered by feeling down, depressed, or hopeless?” and 2) “During the past month, have you been bothered by little interest or pleasure in doing things?”37,69 If the answers to these questions are positive, the patient should be monitored closely and if progress does not occur, then further psychological follow-ups should be considered.70 Does the patient have trouble with work, leisure activities, washing, or dressing? How far can the patient walk before the pain begins?71 What is the patient’s level of disability? Disability implies the effect of the pathology on activity, not pain. Thus, disability testing commonly revolves around activities of daily living (ADLs) and functional activities. Thus, this question may be tied in with the use of the questions in the functional assessment discussed later.
Finally, the examiner must be aware that although in most cases, people who have low back pain have simple mechanical back problems or have nerve root problems involving the disc, there is always the possibility of nonmusculoskeletal causes (e.g., kidney stones, abdominal aortic aneurysm, pancreatic problems) or serious spinal pathology (e.g., tumors).23,37 Waddell outlined signs and symptoms that would lead the examiner to conclude that more serious pathology is present in the lumbar spine (Table 9-6).3
TABLE 9-3
Some Implications of Painful Reactions
| Activity | Reaction of Pain | Possible Structural and Pathological Implications |
| Lying sleeping | ↓ | |
| ↑ | ||
| First rising (stiffness) | ↑ | |
| Sitting | ↑ | |
| With extension | ↓ | |
| ↑ | ||
| With flexion | ↓ | |
| ↑ | ||
| Prolonged sitting | ↑ | |
| Sitting to standing | ↑ | |
| Walking | ↑ | |
| Driving | ↑ | Get Clinical Tree app for offline access 
|