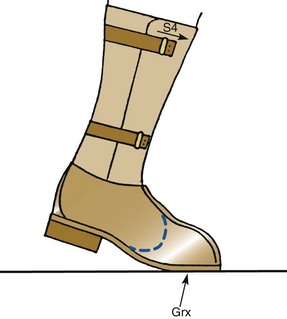
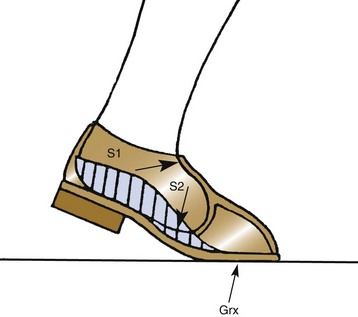
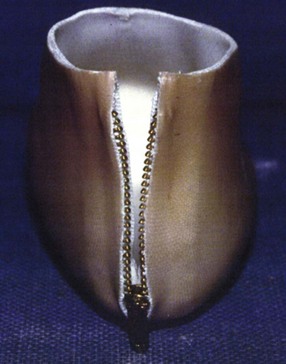
Chapter 29 Treatment by amputation has been a procedure of last resort. The primary goal was the preservation of life rather than a return to high levels of function or athletic endeavors. Although amputation has become a more accepted modality of treatment for the severely diseased or traumatized extremity, some surgeons still resist primary amputation as well as significant study of amputation procedures and outcomes. Limb-salvage techniques continue to improve, often allowing the saving of an at-risk limb. Unfortunately, there is little ability to predict the functional outcome and level of disability and pain from a salvaged limb compared with an amputation. Unfortunately, delaying amputation can result in increased medical expense, increased debilitation, or both, when the patient is nonambulatory for a long time. In some cases, amputation is truly the beginning of rehabilitation.9 Successful prosthetic management after amputation of the lower extremity requires knowledge of the mechanics of the normal foot and ankle, as well as the biomechanical consequences of each amputation level.11 Since the 1950s, the changes in prosthetic care have been in the area of materials and techniques, not with the mechanics of using such a device. These material and technique changes have had a significant impact on the overall function and comfort of an amputee using a prosthetic device. Materials such as silicone and polyurethane have become mainstream, helping to decrease the mechanical forces applied to areas of skin of a remnant limb. Carbon fiber and other materials have allowed prostheses to become lighter and stronger, decreasing the energy expenditure of the amputee during gait. All this is allowing the amputee to claim successes not previously achievable. Determining the level of amputation is often controversial and regionally specific. Traditionally, maintaining length when performing partial foot amputation was standard. Today, quality is more critical than quantity. Current analysis has shown that the former goal of maintaining a longer lever might not affect function or quality of gait and that generation of power across the ankle is significantly decreased irrespective of partial foot length, once the foot is amputated proximal to the metatarsal heads.13 Adding to the controversy over selecting the amputation level is the presence of scar tissue and skin grafts (Fig. 29-1). In cases of trauma, sometimes a decision must be made between saving a partial foot amputation with the addition of a skin graft or performing a Syme or below-knee amputation without additional surgical intervention. In these cases, grafts and scars should be avoided if possible. However, if eliminating grafts and scars requires the next higher level of amputation, the patient’s sensation, age, activities, and future goals must be carefully considered before selecting the level of amputation. When confronted with a phalangeal amputation, complete disarticulation is preferred to partial toe amputation (Fig. 29-2). A five-toe metatarsophalangeal (MTP) disarticulation may be indicated in patients with gross deformity when the toes are rigid, functionless, and painful and, occasionally, in patients with multiple painful MTP dislocations or significant painful clawing of the toes in the vascular-compromised foot. However, in a majority of cases, disarticulation of all five phalanges should be advanced to transmetatarsal amputation because of the potential for skin breakdown under the metatarsal heads. This is especially true in patients with vascular disease and associated neuropathy, who are at high risk for injuring an unprotected foot. The great toe should not be left if the rest of the toes are to be amputated because of potential hallux deformity and inability to wear standard shoes (Fig. 29-3).36 Amputation of a single phalanx usually has minimal effect on gait or comfort during ambulation. Ankle moments, power, and propulsion are minimally affected with this level of amputation. However, if the toe was painful before ablation, some alterations to the gait pattern may be observed. Mann et al22 evaluated patients with surgical ablation of the great toe with no other lower extremity disease. During gait, these patients merely lateralized the center of pressure at the later portions of the stance phase on the amputated side, compensating for the missing toe. However, the reduction of load-bearing areas can result in increased pressure over the metatarsal heads. In the dysvascular population, if adequate protection of the remaining foot is not provided, subsequent ulceration can occur around the lateral portion of the first metatarsal head, extending to the second or third metatarsal. There may also be some loss of push-off at late stance phase, retraction of the sesamoids, and metatarsalgia. A custom-made shoe or custom accommodative insert (or both) is indicated in these patients to protect the remaining foot.14 This may or may not include a filler for the ablated toe. Judicious use of the toe filler is warranted because often they can irritate the adjacent toes and create new problems for the user. Further, there appears to be little evidence of the efficacy of toe fillers in preventing adjacent toe angulation. For other central or multiple phalangeal amputations, the MTP joints of the adjacent toes can deform unless some type of semirigid toe filler is provided. Again, there is currently little evidence demonstrating that toe drift can be prevented with the use of an orthosis, and compliance is often a concern. A custom-molded orthosis or shoe insert should be provided for the dysvascular or diabetic patient for protection of the remaining foot from further insult or amputation (Fig. 29-4). Amputation of two or more phalanges can cause some gait deviation, depending on which toes have been amputated. A carbon-fiber plate might be required in the shoe to offset any shoe deformation at late stance, but care must be taken not to make the shank too stiff so that it adversely affects late stance phase during gait.11,40 Cosmetic toe prostheses may also be custom fabricated and may be used in conjunction with the existing arch support or independently. Using the contralateral toe as a model, the cosmetic toe filler may contain layers of color, and even hair, to enhance the appearance. Such a device might have minimal or no functional quality but can appear quite lifelike (Fig. 29-5). Single-ray resections at the second, third, fourth, or fifth metatarsal have been quite successful and leave a functional partial foot that may not need prosthetic intervention.43 Long-term observation of these patients is needed because the increased pressure under the remaining toes can lead to ulceration.10,39 Loss of the first ray leaves the foot somewhat less effective than with removal of the lateral rays because the foot does not balance well with the loss of the windlass mechanism, and the increased pressure under the remaining metatarsals can lead to further ulceration (Fig. 29-6).7,9,35 When removing two or more rays, especially on the medial side of the foot, prosthetic or orthotic intervention for gait, comfort, and protection of the remnant foot and appropriate footwear become essential. Removal of two central rays also narrows the foot significantly, makes wearing shoes difficult, and can increase the potential for skin breakdown (Fig. 29-7). Studies have shown an increase in callosities, ulceration, balance problems, and pain with multiple ray amputation.10,17,38 When the option is to remove several central or lateral rays or move to a higher amputation level (a transmetatarsal or Lisfranc amputation), the ray resection provides a more functional foot than a higher amputation does. When the option is to remove several medial rays or proceed with a transmetatarsal or Lisfranc amputation, the patient’s general health and activity level must be carefully considered before determining the appropriate level. (See the discussion of transmetatarsal amputation.) Custom-molded insoles may be used to distribute pressure evenly over the remainder of the foot after ray amputation to stabilize and protect the remaining foot. Softer, more conforming foam generally is used against the skin, whereas a firmer material is used for the base.25,26,37 Custom-made shoes may be required if significant function is lost after amputation or if the foot is severely misshapen and unable to fit into a standard shoe. Rocker-bottom soles are easily applied to shoes if ambulation becomes difficult or painful. Although rocker-bottom shoes have been advocated in many conditions such as this, their use is somewhat limited by the appropriate shoes, cosmesis, patient compliance (or lack thereof), and reimbursement issues. Transmetatarsal amputation was first described in 1855, but success at that time was limited. After the advent of antibiotics, this level of amputation was performed routinely in patients with limited gangrene, deformities of the toes, trauma to the forefoot, rheumatoid arthritis, or controlled infection.23 The residual limb is acceptable both in function and in cosmesis, despite the splaying of the metatarsals often present after surgery. Biomechanical evaluation of transmetatarsal amputations shows significantly greater plantar pressure when compared with intact feet, most likely because of the smaller surface area. In addition, increased forces have been noted at the distal end of the limb, and a significant lack of dynamic dorsiflexion during late stance has been recorded. This loss of stance-phase dorsiflexion may be associated with the missing ground reaction force at the distal end of the foot at late stance, leaving a functional equinus contracture17 with the potential ramifications of ulceration and distal limb pain. Therefore some form of protective footwear should be used in this population.17 Further, an intact or replanted tibialis anterior tendon is crucial to ensure proper support of the medial column. Achilles tendon lengthening should be considered for this population because current research has shown limited functional use of the gastrocnemius-soleus complex in patients with transmetatarsal amputation, regardless of the type of prosthesis they use.5,14,15 Any device designed for a transmetatarsal amputation must compensate for the loss of the later portions of stance phase and the loss of cosmesis, and it must allow appropriate footwear and a comfortable gait pattern. With the removal of the metatarsal heads, distal weight bearing is no longer practical. Therefore any prosthetic device not only must protect the cut ends of the bones, both distally and on the plantar surface, but also must resist the natural dorsiflexion moment of the prosthesis on the residual limb at late stance phase.15,19 The only devices shown to be effective in improving late stance-phase kinematics (kinetics and temporal spatial factors) are designs that control dorsiflexion and have a relatively stiff forefoot that will permit the amputee to walk such that the center of pressure extends beyond the end of the residual limb under loading. It appears that low-profile prostheses and orthoses have no impact on the movement of the center of pressure in late stance phase and thus can be considered to be biomechanically accommodative interventions that will not have the potential to affect step length (Fig. 29-8).5 A resistive force must be placed on the more proximal portion of the dorsum of the foot (through the shoe or prosthesis) or via an anteriorly directed force proximal to the calcaneus (Fig. 29-9). The late-stance dorsiflexion force can be overcome with a device that has an anterior strap proximal to the malleoli, as in an ankle–foot orthosis (AFO) design (Fig. 29-10). It is important that the foot plate be stiff enough to overcome the force needed to support the body in late stance but not so stiff that the third rocker is adversely affected and the patient is unable to roll over the foot. A rocker-bottom sole could be added to any shoe to allow a reduction of distal metatarsal pressure, if the patient is willing to use such a device (Fig. 29-11). Figure 29-11 Typical rocker-bottom sole added to a shoe to enhance late stance phase and reduce terminal pressures. A custom shoe insert with toe filler can accomplish these goals if the patient ambulates with a flatfoot gait (i.e., has no real heel strike or terminal stance) or uses the device in conjunction with a high-top or rocker-bottom shoe. The insert must be somewhat rigid and well padded around the distal end. The shoe must also be comfortable, especially around the proximal-anterior edge, because much pressure will be absorbed by this area during the latter portions of gait. The sole of the shoe must have some rigidity as well because a shoe that is too flexible increases pressure over the distal end of the limb and at the anterior-proximal edge of the shoe (Fig. 29-12).8 The Lange partial foot prosthesis was designed to combat some of the pitfalls of the previous devices. It is made of silicone with a carbon-fiber foot plate to resist the force at the later portions of the stance phase. The prosthesis has a posterior opening with a zipper and fits snugly around the proximal aspect of the calcaneus, offering resistance to late stance-phase pressures (Fig. 29-13). This design allows the proximal segment of the prosthesis to be flexible rather than rigid. The proximal edge may come up as high as necessary to assist in comfort, and this device usually fits into a standard shoe or sandal.
Lower Limb Prosthetics
Partial Foot Amputation
Selecting the Level of Amputation
Phalangeal Amputation
Surgical Considerations
Prosthetic and Biomechanical Considerations
Ray Amputation
Surgical Considerations
Prosthetic and Biomechanical Considerations
Transmetatarsal Amputation
Surgical Considerations
Prosthetic and Biomechanical Considerations

![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Lower Limb Prosthetics