Chapter 27 Lower limb orthoses for persons with spinal cord injury
Approximately 11,000 individuals in the United States sustain a spinal cord injury (SCI) every year. Between 220,000 and 285,000 individuals currently are living with an SCI.35–38,47,114 The average age at injury is 38 years; 78% of SCIs occur in men.35–3847 An estimated 54.1% of injuries occur in individuals between 16 and 30 years old.36,114,121 Primary causes of SCI include motor vehicle accidents, military- or paramilitary-related injuries, violence, sports, and falls.2,114,121
Pathophysiology
Level of injury
The most accepted and consistent means of SCI classification and measure of impairment is the International Standards for Classification of Spinal Cord Injury, written by the Neurological Standards Committee of the American Spinal Injury Association (ASIA).3 This examination allows a clinician to systematically examine the dermatomes and myotomes in order to determine the spinal cord segments affected by injury.
For the motor examination, a consensus of experts paired key motions with specific myotomes. Levels included muscles corresponding to myotomes C5–T1 in the upper limbs and L1–S1 in the lower limbs. Strength is graded on a six-point scale as follows: 0 is total paralysis, 1 is palpable or visible contraction, 2 is movement through the full range of motion (ROM) in a gravity eliminated position, 3 is movement through the full ROM against gravity, 4 is movement through the full ROM with moderate resistance, and 5 is movement through the full ROM with full resistance. The external anal sphincter is tested and graded based on the absence or presence of contraction around the examiner’s finger.
A very important but often misunderstood concept from the ASIA examination is the distinction of incomplete from complete SCI. A patient is classified as having an incomplete SCI if partial preservation of sensory and motor function is found below the neurological level and must include the lowest sacral segment (S4–S5).3,93 A person is classified as having a complete injury if he or she has no sensory or motor function in the lowest sacral segment. The definitions have changed since the Frankel Classification, so caution should be taken when comparing studies conducted before and those after 1996.3,44,93
Current issues
Protecting and/or maintaining a joint with an orthosis is the least controversial of goals. For example, if during the time of the injury a patient fractures the femur, then utilization of a knee immobilizer or fracture brace to protect the injured area is appropriate. For long-term maintenance of a joint, an orthosis can prevent contractures. In the early stages of an injury, a patient typically is in spinal shock and presents with flaccid lower limbs (hypotonicity).5 The foot falls into the plantarflexed position combined with inversion, producing an equinovarus position. As the patient emerges from spinal shock, typically 1 to 3 months after an injury, tone gradually intensifies. As tone increases, the lower limbs will experience muscle spasms into an extensor synergy, typically hip internal rotation, knee extension, ankle plantarflexion, and foot inversion. Therefore, there is a tendency both before and after spinal shock for the ankle to be in equinovarus. In a relatively short period of time, a patient can develop a plantarflexion contracture, which has detrimental effects on future transfers, ambulation, wheelchair positioning, and dressing. To prevent a plantarflexion contracture, the ankle should be held in a neutral position, which is easily accomplished using a prefabricated antifootdrop orthosis (Fig. 27-1).137,138 Regardless of the type of orthosis used, it must be well padded, and the feet must be checked frequently for pressure areas. Loss of sensation resulting from SCI places all patients who wear orthoses at high risk for developing pressure ulcers. Once the orthosis is removed, any redness should resolve after 20 minutes. With routine findings on skin examinations, wearing time is gradually increased.
For children with SCI, orthoses are vital for promoting normal bone alignment during growth. Areas that can indirectly impact the lower limb and frequently require orthotic interventions are the hips and spine. A level pelvis is vital for maintenance of an erect stable position for functional activities in sitting and for adequate distribution of sitting pressures for prevention of skin breakdown.17,41,80 From 80% to 98% of children injured before the age of skeletal maturity develop scoliosis.88,91 Early bracing of the spine may delay the age at which surgical intervention is required, and curves less than 20 degrees reduce the possibility of requiring a surgical fusion.99 Prescribing a thoracolumbosacral orthosis (TLSO) may serve several functions, including maintaining skeletal alignment that prevents the rapid progression of scoliosis, distributing seated pressures, providing trunk stabilization during functional activities, assisting with breathing, and increasing stability during upright mobility during ambulation.17,33,91,94,112,139 Of note, although a TLSO may aid in some activities, it has been shown to interfere with activities such as dressing, transfers, and wheelchair propulsion.22
In addition to scoliosis, hip subluxation/dislocations in injured children are a concern.128,160 In a review of 62 patients, McCarthy et al.98 found that 93% of patients injured before age 11 years had at least one hip subluxed or dislocated, compared to 9% of patients older than 11 years. Poor development of the hip results from a combination of decreased muscle tone, which is necessary for maintaining femoral head positioning, poor acetabular development resulting from the absence of weight bearing and muscle pull, and, for patients with spasticity, the constant positioning of the hip in adduction and internal rotation. To facilitate proper femoral head/acetabular positioning while supine, an abduction pillow can be used to maintain hip abduction.19 When sitting in the wheelchair, a patient should be positioned with the pelvis facing forward and the femurs in slight abduction, which can be facilitated by use of an abduction pommel. Similarly, when sitting upright or playing on the floor, children should be encouraged to circle sit and to avoid side sitting.57 Side sitting encourages a windswept deformity with one limb maintaining an adducted and internally rotated position, which encourages subluxation of the femoral head.
The most controversial use of lower limb orthoses, also referred to as (hip)–knee–ankle–foot orthoses [(H)KAFOs], in patients with SCI is for functional mobility. Frequently, the primary goal of an acutely injured individual is to “walk again.” After an injury, patients must quickly come to the realization that the ability to stand and achieve mobility (“walking”) is significantly reduced, if not impossible. Being upright and returning to mobility symbolize recovery or the “appearance of recovery” to many patients. When presenting the options of bracing for upright mobility to a patient, it is the responsibility of the health care provider to discuss their use to ensure that the patient’s expectations are realistic.102,155,161,162 Although no evidence indicates that being upright promotes neurological recovery, some evidence indicates that (H)KAFOs have perceived psychological, social, and possible physiological benefits.21,42,76–78,86,96,132,152,155
To guide clinicians who work with patients having SCI, the American Paraplegia Society has created clinical practice guidelines based on outcomes studies and expert clinical judgments for patients with motor complete SCI at 1 year after injury.26 These outcome-based practice guidelines, available through the Paralyzed Veterans Association, should be used by clinicians throughout their practice. The guidelines suggest using a stander for individuals with injuries above T1. For injuries at T1 and below, either a stander or orthoses for therapeutic or functional activities are an option.26
Walking patterns
The walking pattern a patient hopes to achieve plays an important role in orthotic selection. The two main walking patterns are reciprocal stepping (step to/step through) and swing through/swing to.5,146 In the former, patients move each limb independently; in the latter, patient move both lower extremities simultaneously. Depending on the patient’s physical condition, either pattern can be accomplished with a standard walker, rolling walker, or crutches. In a step-to/step-through pattern, the patient shifts weight laterally and uses body position or the mechanics of a brace to advance the contralateral limb. For a swing-through/swing-to pattern, the patient lifts the entire body weight and uses momentum and body positioning to simultaneously advance both legs.
Types of orthoses
Knee–ankle–foot orthosis
A KAFO is used to provide stability at the knee and ankle while indirectly affecting hip stability through ground reaction forces. It typically is prescribed for individuals who have little to no quadriceps strength. A KAFO consists of leather or thermoplastic thigh and calf bands attached to metal uprights joined by a footplate. The most common KAFO is the Scott-Craig KAFO or a variant of the Scott-Craig KAFO.89,136 In a patient with paraplegia, maximal stability in standing with a KAFO is achieved with the ankle positioned in neutral or dorsiflexion, the knees locked in extension, and the hips passively positioned in extension. In this position, sometimes referred to parastance, an extension moment is created at the hips, which prevents the individual from folding forward while hip extension is passively maintained by the anterior capsular ligaments of the hip (Fig. 27-2).5,133,146 However, when the patient ambulates, the hips transition through flexion, and crutches or other assistive aids are essential for stability.
Hip–knee–ankle–foot orthosis
A hip–knee–ankle–foot orthosis (HKAFO) is an orthosis whose components stabilize or lock the hip, knee, and ankle. The typical HKAFO is a pair of KAFOs linked above the hip with either a pelvic band, lumbosacral orthosis, or TLSO. An individual may require a hip component because of the level of injury; hip flexion, knee flexion, or ankle plantarflexion contractures; poor balance; or decreased motor control. The hip section provides significant stability in the transverse plane and, if the hip joints are locked, also provides sagittal plane stability. When the hips are locked, individuals will commonly use a swing-to or swing-through gait.133 Some patients are able to unlock the hips to achieve a reciprocal gait pattern using body positioning and weight shifting. A hip guidance orthosis (HGO), also known as the Orthotic Research and Locomotor Assessment Unit (ORLAU) Parawalker, is an example of an HKAFO with free-moving hip joints that allow a reciprocal gait pattern.18,130,131,152
A reciprocating gait orthosis (RGO) is an HKAFO that uses a mechanical system that connects the two sides of the brace by an isocentric bar (IRGO), double cable (LSU RGO from Louisiana State University), or single push/pull cable system (advanced RGO [ARGO] developed by Hugh Steeper Ltd.).40,70,109,167 Regardless of the mechanism, the patient achieves a reciprocal gait by shifting body weight forward and laterally while extending the hips and upper trunk. In theory, the hip extension of the weight leg enables the orthosis mechanism to advance the unweighted leg. Unlike a swing-through gait that requires users to lift body weight plus the weight of the orthosis, the RGO relies on weight shifting and orthotic mechanics for mobility. Although it has been suggested that RGOs are less energy demanding than standard (H)KAFOs, the evidence is not conclusive.27,157,165 Furthermore, some authors have questioned the usefulness of the linkage system in driving the hip into flexion during the swing-through phase of gait; but they do suggest that the RGO system may increase stability by limiting hip flexion of the stance leg or bilateral hip collapse during double support.28,29,62
Two orthoses in development that have expanded on the basic RGO are the hip and ankle linked orthosis (HALO) and the stance control orthosis (SCO).46,127 The HALO is a cable system that links both ankle joints with a medial hip joint. The linkage of the ankles by way of a pulley system results in assistance of the swinging leg when the contralateral ankle is flexed. The design maintains parallel alignment of the feet to the ground, reducing the need for excessive pelvic rotation.46 The SCO has knee joints, thus providing stability during stance but free motion of the knee during swing through. The developers of the SCO suggest combining their design with the IRGO concept in an attempt to decrease the energy required during gait for the SCI population.
Progressive upright mobility bracing
Initially, some individuals are unable to achieve a parastance with KAFOs alone and therefore require an (H)KAFO, such as an RGO. Eventually, as strength, coordination, or balance improves or contractures reduce, the hip component can be modified or removed, progressing the individual to less bracing. Having an RGO or HKAFO with a detachable superior section allows an individual to experience the advantage and disadvantage of the different gait patterns (swing through or reciprocal) without and with hip stabilization. After trying each option, the individual can decide what brace and gait pattern works best for him or her.52,155,161,168
Treatment recommendations
When considering orthoses for upright mobility, first and foremost the clinician must understand the patient’s expectations and motivation. Expectations must be realistic. Patients, particularly those with higher-level injuries, should understand that the substitution of orthoses for upright mobility rather than utilization of a wheelchair is the exception rather than the rule.43,56,90,129,155 Patients may accomplish limited indoor functional mobility with bracing and in most cases (with assistance and time) can continue to use upright mobility for therapeutic benefits.43,90,124 Patients and caregivers must understand that upright mobility is not a treatment of spinal cord injury. During semistructured interviews before starting gait training, some caregivers have expressed the “hope” that using braces would “wake up” the spinal cord and promote recovery (personal communication, senior author). On the other hand, other interviewees did not expect neurological recovery but viewed upright mobility as another important step in the rehabilitation process. These patients/caregivers expressed to the coauthor (R.C.) that even if they did not have long-term use of the braces, at least they knew they could do it.
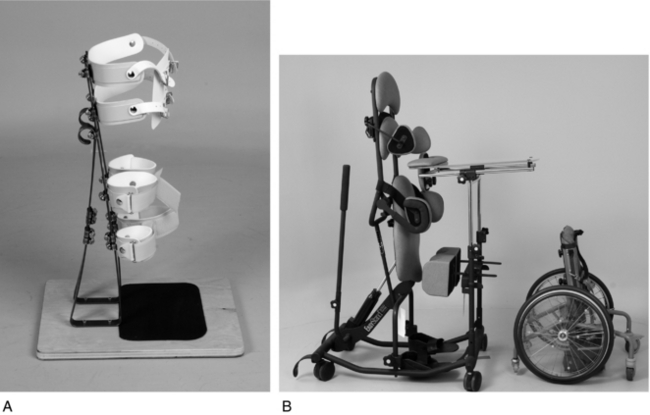
For patients who are interested in being upright for psychological and physiological benefits but are not interested in mobility, the most appropriate device may be a stander.56,124,150 For children, several options are available. A custom stander, such as the L-frame (Fig. 27-3, A), can be ordered. The parapodium and swivel standers can provide the ability to be upright with limited mobility using a footplate or an oval bottom.147,162 By using assistive devices, patients can move slowly, leaning their body to one side and rotating the trunk to the opposite side. The Rabbit, an appliance in which a patient is strapped into a stander and has large wheelchairlike wheels for mobility, is another option. (Fig. 27-3, B). For children and adults, standing can be accomplished with commercially available standers. These standers have either a seat into which the patient transfers or straps to secure the pelvis so that the patient can stand positioned directly from the wheelchair. A hydraulic pump on the side of the stander aids transition to the upright posture (Fig. 27-3, B).
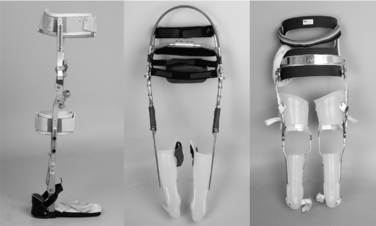
To help the patient understand the limitations of custom orthoses for upright mobility, a thorough interview and physical examination are required. During the interview, the clinician should determine why the patient wants to be upright and what he or she hopes to accomplish. For example, consider an athletic patient with a T9 injury and no significant comorbidities. If this patient’s goal is spontaneity of activities for short distances, using lightweight KAFOs that can be hidden under clothing may be appropriate. On the other hand, if the patient is interested in using the orthoses for limited function and prefers a reciprocating gait pattern, then a Parawalker or RGO may be more suitable. To ensure understanding of the pros and cons of orthosis use, patients should talk to peers who have used braces in the past. Videos will help patients visualize the different assistive devices used, gait patterns, and appearance of orthoses. Temporary adjustable KAFOs and/or trial ARGO are another option (Fig. 27-4).134
If orthopedic considerations are minimal, spasticity should be assessed next. Standing may reduce the severity of spasticity. In contrast, movement may trigger a patient’s spasticity, preventing safe advancement of the lower limbs. If spasms are severe, antispasticity medications are an option.1 Lastly, patients who have not been upright for many weeks are at risk for hypotension. A hypotensive patient can adjust to the upright position by graduated use of a tilt table and compressive elastic garments.
Orthotic management
Sagittal plane
At the foot, custom molding the device to the foot is best. Placing the orthosis in the shoes is cosmetically more appealing, allows the orthoses to be worn with a variety of shoes, and facilitates donning of the orthoses (Fig. 27-5). Care should be taken to ensure adequate arch support is provided to prevent excessive foot pronation. Without arch support, excessive pronation increases both forefoot and calcaneal valgus, increasing pressure on the head of the fifth metatarsal and the lateral calcaneous.116 A second option is a steel stirrup riveted to the shoe. A third option, used primarily with the Parawalker and some pediatric RGOs, is a broad external footplate that attaches directly to the two metal supports. The broad base of support will increase standing stability. Because the device is worn external to the shoe, it can be donned and doffed with ease.130,165 Regardless of the footwear, during initial training a small rocker sole can facilitate toe-off.
At the ankle, options range from a custom solid molded AFO to a variety of joints that attach metal uprights to the foot insert or stirrups. Although a solid AFO maximizes pressure distribution and stability, it minimizes motion of the ankle. Using adjustable ankle joints, dorsiflexion can be adjusted to aid in maintaining parastance. Furthermore, ankle adjustment can be made if the patients gains or loses ROM over time.11 It has been suggested that special modifications to a patient’s shoe may increase walking speed and step length.153
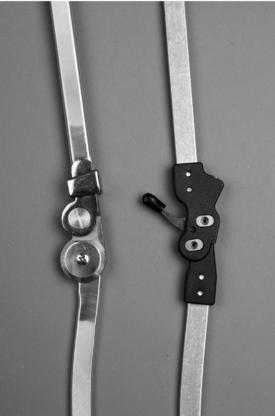
For sagittal stability at the knee, several options are available. The most common type of joint is a ring-type drop lock that the patient pushes down over the orthotic knee joint (Fig. 27-6, left). Another common lock is the Step Lock (Steplock OTS Corp., Weaverville, NC) which ratchets into position and is released with a lever (Fig. 27-6, right). A pawl lock automatically locks the knee when fully extended and is released by upward pressure. Some orthoses are made with the pawl locks attached by a metal “bail” behind the knee (Fig. 27-6).141 Using the bail, patients can back up to a chair, apply upward pressure to the bail, and release the locks to allow sitting. With the bail some caution is necessary over tight trousers or adductor spasticity, which can accidentally trigger the unlocking mechanism. A mechanical locking mechanism is unnecessary in patients with sufficient quadriceps strength. A posteriorly offset knee join keeps the knee stable in standing because the orthotic joint axis is posterior to the anatomical knee axis. Caution is warranted with posteriorly offset knee joints because an improper weight shift or standing on a downgoing ramp can destabilize the knee. A more advanced knee joint with gas-filled struts is available with ARGOs.70 This joint assists with the upward motion during sit-to-stand transfers and provides assistance with deceleration from standing to sitting (Fig. 27-4, center). New knee joints are being introduced into clinical use that allow for limited knee flexion during gait or have computers that control stability.48,127,158
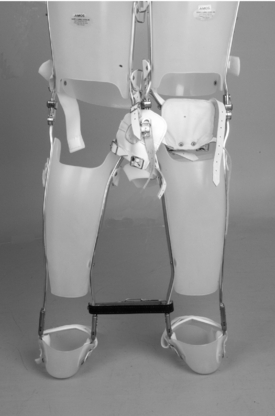
At the hip, sagittal stability is required for patients who have hip flexion contractures and therefore are unable to achieve the parastance. As for the knee, the most common hip joint is a pair of drop locks attached to a pelvic band. If more trunk stability is required, a custom lumbosacral orthosis or TLSO section can be added. For patients with an RGO, a trunk section is necessary to engage the reciprocating mechanism in stance (Fig. 27-4, right). Although the hip component will increase standing stability, the addition of a hip section can make donning and doffing the brace cumbersome.76 Abduction hinges with locks will control hip adduction and increase the ease of donning/doffing and bowel/bladder management (Fig. 27-7).
Transverse plane stability
Orthotic stability in the transverse plane typically is achieved by connecting the legs of the orthoses, which can be done at or below the hip. The hip sections can be linked with a pelvic band for increased stability in the transverse plane. If sagittal stability at the hip is not an issue, the hip joints can remain unlocked, allowing a reciprocal gait pattern as in the HGO. Reported benefits of the HGO are its lateral stiffness, which prevents adduction during swing through of the free limb, and broad footplates, which encourage stability during double limb stance.130,148 A patient with a hip obliquity due to scoliosis or hip subluxation will have difficulty maintaining parallel alignment of the lower limbs and thus may benefit from some type of connected hip section. It has been suggested that children, whose Y-ligaments are more pliable, may have trouble maintaining a stable parastance and would benefit from a pelvic section.102 Transverse stability also can be achieved by linking each leg below the hip by using a spreader bar; however, a spreader bar does eliminate the possibility of a reciprocal gait (Fig. 27-8). For a reciprocal gait without transversing the hip, KAFO sections can be linked with a single medial hinge joint such as the walkabout orthosis (WO) or the Primewalk orthosis.103–105153
Current research
Orthoses
An individual with an SCI who learns about bracing for ambulation frequently assumes that the braces will allow functional ambulation, replacing the wheelchair. Unfortunately, for most patients (particularly those with lesions above T12), this goal is unrealistic because of the physiological demands of ambulation with orthoses.12,20,49,60,164 Gordon and Vanderwalde49 conducted one of the first studies quantifying energy expenditure in neurologically impaired patients. They concluded that the high-energy costs are prohibitive for ongoing ambulation. They ended their study by concluding that “paraplegic ambulation ranges from moderate to hard work and must be judiciously prescribed.” Confirming the decreased efficiency of paraplegic ambulation, Cerny20 compared the energy required for level walking with KAFOs to wheelchair propulsion in patients with paraplegia. He found that subjects traveled at more than twice the velocity at a statistically lower physiological cost when using a wheelchair as compared to walking. Comparing published metabolic measures for paraplegic brace ambulation to noninjured subject walking, he found that velocity was half, with the rate of oxygen uptake increased by 50%. Furthermore, the respiratory quotient was 0.12 higher than normals, indicating increased dependency on anaerobic energy production. When compared to paraplegic wheelchair propulsion, the subject’s heart rate, oxygen uptake, and respiratory quotient mirrored normal walking with only 2% to 6% increase. He confirmed earlier reports that the energy expenditure during paraplegic ambulation was nine times greater than that of normals.24,101 Merkel et al.101 found that for higher-level injury (C8–T3), energy per meter during ambulation was 25 times that of normals. Looking at more functional tasks with KAFOs, Miller et al.107 compared energy expenditure of patients with SCI to normals while negotiating different architectural barriers found in a typical environment, such as ramps, stairways, narrow corridors, and multiple turns. They found that, depending on the task, the energy cost per meter was up to 15 times that of noninjured subjects. Their studies support what patients discover, namely, that functional mobility in a wheelchair is more efficient than walking with braces.20,43,56,90,129,155
More recent studies suggest that adding the hip component has reduced overall energy costs. Nene et al.118,119 studied energy costs in 10 subjects with T4–9 spinal lesion who used the Parawalker (HGO) and compared their results to the published literature on KAFOs. They found that braces that crossed the hips increased the users’ velocity of ambulation and reduced energy cost. Improvement in gait efficiency with HGOs may make ambulation a realistic active activity in patients with mid- to high-level injuries. In a comparison of HGO to RGOs, Banta et al.8 found that HGOs produced a more efficient gait and a greater walking velocity. Whittle et al.165 studied a group of 18 patients who trained with both HGOs and RGOs. Their report did not look at energy costs but rather a series of tasks and self-reported ease of use. At the end of the study, of the 16 patients, 12 chose to continue with their RGOs and 4 with the HGOs. Ease of donning and doffing was reported with use of HGOs, whereas the RGOs were preferred for their appearance and stability when standing. In another study comparing within the same patient, Katz et al.79 compared the energy efficiency of patients with myelodysplasia who were using an HKAFO or an RGO. They found the mean oxygen cost was 1.5 mL/kg/m with the HKAFO and 0.73 mL/kg/m with the RGO. Patients were faster with the RGO than with the HKAFO (14.6 m/min and 11.9 m/min, respectively). Using braces in the community setting, several patients commented that the RGO was easier to manage on rough terrain. At the end of the study, seven of the eight subjects preferred to continue use of the RGO. In a comparison of the LSU RGO and the IRGO, Windchester et al.167 examined energy cost using the physiologic cost index (PCI, calculated by dividing the difference between walking and resting heart rate by velocity). They found in four subjects with paraplegia that PCI was significantly lower for IRGO compared to RGOs and concluded that energy costs were lower for the IRGO.
Comparing IRGOs to the WO, Harvy et al.53 also found lower metabolic demands with the RGOs. In their randomized cross-over study of 10 patients with complete T9–12 paraplegia, oxygen cost was essentially twice as much with the WO (range 3.95–4.91) compared to the IRGOs (range 1.6–1.8).53 Furthermore, the IRGOs resulted in a faster more independent gait among patients.55 Regardless of the advantages of the IRGOs over the WO, both orthoses were used mainly for therapeutic purposes only once every 1 to 2 weeks.54
It is clear from the literature that metabolic efficiency does necessarily translate to the primary outcome of long-term orthotic use. In addition to metabolic economy, the independence, cosmesis, reliability, and cost (as described by Stallard et al.149) are crucial to the successful design of an orthosis. A wide range of long-term orthotic use has been reported in the literature. Major et al.92 reviewed the charts of 42 patients older than 16 years who were prescribed the Parawalker. Their cohort included patients with myelomeningocele and traumatic or acquired SCI. They found 59.5% compliance with the braces after 71 months. This finding supports a report by Moore and Stallard,108 who found that Parawalker use at an average follow-up of 34.4 months was 64% in 50 adult patients with spinal lesions. This finding is similar to a previously reported study with a shorter follow-up period of 20 months that found 85% (17/20 patients) Parawalker use.152 Franceschini et al.43 examined the outcomes of 74 patients with SCI. In this multicenter study with much shorter follow-up of 6 months, reported orthosis use was 68%. The majority of patients reported using their orthosis for functional gait or therapeutic exercise. The authors found correlations between functional ambulation and age, level of lesion, stair climbing ability, duration of training, and lapse of orthosis use. They suggested that by discharge from the hospital, the patient should use the orthosis 5 to 6 hours per day indoors and outdoors and should be able to climb some stairs.43 Jaspers et al.69 found a similarly high rate of use. In their report of 14 patients, 85% who were prescribed ARGOs continued their use after 3.3 years of follow-up.
Although these results are encouraging, lower proportions of use also have been reported.25,42,43,56,61,106,129,132,150,155,161 Robb et al.129 followed 22 patients with L3–4 and above paraplegia (mostly spina bifida) who were randomly prescribed either an RGO or an HGO. At 1 year, regardless of type of orthotic assigned, none of the participants were scored as wheelchair users on the Hoffner scale. At follow-up of all participants at 5 years, orthosis used dropped to 45%, and after another 5 years was 23%. Similar to previously published work, the HGO required fewer repairs than RGOs.90 Using a mailed questionnaire, Eng et al.42 found that 30% of respondents participated in some form of standing activity, mostly for therapeutic than for functional purposes. Subjective benefits of standing included a “feeling of well-being, looking others in their eye, reduction of spasticity, improved circulation, digestion, breathing, sleep, pain, and bowel/bladder function.” Their reported outcomes may actually be lower as they had a response rate of only 35%.42 In another study, 85 patients given an RGO from 1986 to 1993 were sent questionnaires regarding orthotic use. In this study, nonresponders or unreachable patients were classified as nonusers.155 After a mean follow-up of 5.4 years, only 29% were classified as orthosis users. In this study, higher use was associated with function independence and age.155 Scivoletto et al.135 examined the outcomes of orthotic use based on social, physical, and psychological factors in patients with SCI who received gait training with RGOs. After 1 year, 56% of patients continued using their RGO. Similar to previous studies, they found associations with nonuse because of difficulty during functional activities such as donning/doffing, car transfers, outdoor ambulation, and stair climbing. Examining psychological outcomes, they found that nonusers had higher frequency values over the mean in the extroversion scale for the Eysenck Personality Questionnaire. This study underscores the importance of not only trying to make an orthosis more energy efficient but also exploring the expectations, motivations, and goals of the patients.135
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree