Lower Leg, Ankle, and Foot
At least 80% of the general population has foot problems, but these problems can often be corrected by proper assessment, treatment, and, above all, care of the feet. Lesions of the ankle and foot can alter the mechanics of gait resulting in movement impairments and, as a result, cause stress on other lower limb joints, which in turn may lead to pathology in these joints.1
The foot and ankle combine flexibility with stability because of the many bones, their shapes, and their attachments. The lower leg, ankle, and foot have two principal functions: propulsion and support. For propulsion, they act like a flexible lever; for support, they act like a rigid structure that holds up the entire body.
Although the joints of the lower leg, ankle, and foot are discussed separately, they act as functional groups, not as isolated joints. As the terminal part of the lower kinetic chain, the lower leg, ankle, and foot have the ability to distribute and dissipate the different forces (e.g., compressive, shearing, rotary, tensile) acting on the body through contact with the ground.2 This is especially evident during gait. In the foot, the movement occurring at each individual joint is minimal. However, when combined, there normally is sufficient range of motion (ROM) in all of the joints to allow functional mobility as well as functional stability. For ease of understanding, the joints of the foot are divided into three sections: hindfoot (rearfoot), midfoot, and forefoot.
Applied Anatomy
Hindfoot (Rearfoot)
Tibiofibular Joint.
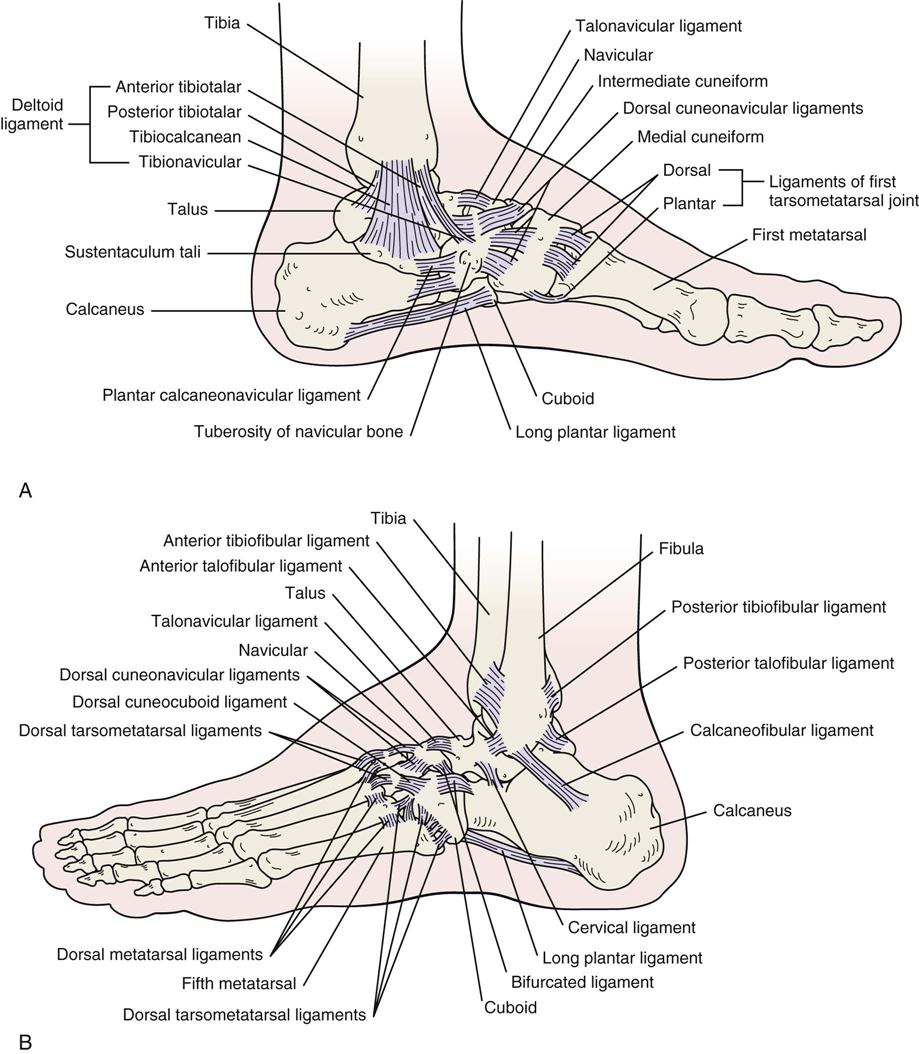
The inferior (distal) tibiofibular joint is a fibrous or syndesmosis type of joint. It is supported by the anterior tibiofibular, posterior tibiofibular, and inferior transverse ligaments as well as the interosseous ligaments (Figure 13-1). The movements at this joint are minimal but allow a small amount of spread (1 to 2 mm) at the ankle joint during dorsiflexion. This same action allows the fibula to move up and down during dorsiflexion and plantar flexion. Dorsiflexion at the ankle joint causes the fibula to move superiorly, putting stress on both the inferior tibiofibular joint at the ankle and the superior tibiofibular joint at the knee. The fibula carries more of the axial load when it is dorsiflexed. On average, the fibula carries about 17% of the axial loading.3 The joint is supplied by the deep peroneal and tibial nerves.
Talocrural (Ankle) Joint.
The talocrural joint is a uniaxial, modified hinge, synovial joint located between the talus, the medial malleolus of the tibia, and the lateral malleolus of the fibula. The talus is shaped so that in dorsiflexion it is wedged between the malleoli, allowing little or no inversion or eversion at the ankle joint. The talus is approximately 2.4 mm (0.1 inch) wider anteriorly than posteriorly. The medial malleolus is shorter, extending halfway down the talus, whereas the lateral malleolus extends almost to the level of the subtalar joint. The joint is supplied by branches of the tibial and deep peroneal nerves.
The talocrural joint is designed for stability, especially in dorsiflexion. In plantar flexion, it is much more mobile. This joint is responsible for the anterior-posterior (dorsiflexion-plantar flexion) movement that occurs in the ankle-foot complex. Its close packed position is maximum dorsiflexion, and its capsular pattern is more a limitation of plantar flexion than of dorsiflexion. This joint is most stable in the dorsiflexed position. The resting position is 10° of plantar flexion, midway between maximum inversion and maximum eversion. The talocrural joint has one degree of freedom, and the movements possible at this joint are dorsiflexion and plantar flexion.
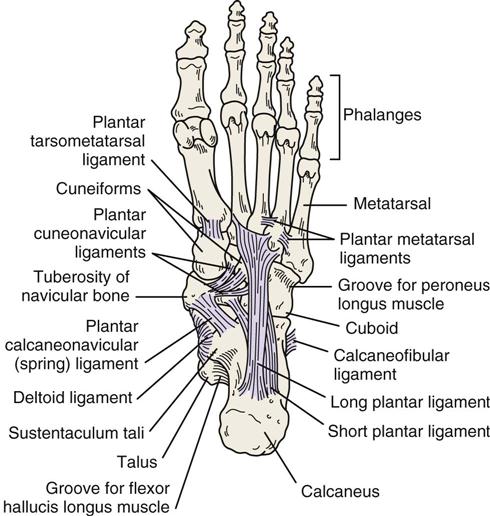
On the medial side of the joint, the major ligament is the deltoid or medial collateral ligament, which consists of four separate ligaments: the tibionavicular, tibiocalcanean, and posterior tibiotalar ligaments superficially, all of which resist talar abduction, and the anterior tibiotalar ligament, which lies deep to the other three ligaments and resists lateral translation and lateral rotation of the talus. On the lateral aspect, the talocrural joint is supported by the anterior talofibular ligament, which provides stability against excessive inversion of the talus; the posterior talofibular ligament, which resists ankle dorsiflexion, adduction (“tilt”), medial rotation, and medial translation of the talus; and the calcaneofibular ligament, which provides stability against maximum inversion at the ankle and subtalar joints. The anterior talofibular ligament is the ligament most commonly injured by a lateral ankle sprain, followed by the calcaneofibular ligament.
Subtalar (Talocalcanean) Joint.
The subtalar joint is a synovial joint having three degrees of freedom and a close packed position of supination. Supporting the subtalar joint are the lateral talocalcanean and medial talocalcanean ligaments. In addition, the interosseous talocalcanean and cervical ligaments limit eversion.
The movements possible at the subtalar joint are gliding and rotation. With injury to the area (e.g., sprain, fracture), this joint and the talocrural joint often become hypomobile, partially because the talus has no muscles attaching to it. Medial rotation of the leg causes a valgus (outward) movement of the calcaneus, whereas lateral rotation of the leg produces a varus (inward) movement of the calcaneus. The axis of the joint is at an angle of 40° to 45° inclined vertically and 15° to 18° to the sagittal plane.
Midfoot (Midtarsal Joints)
In isolation, the midtarsal joints allow only a minimal amount of movement. Taken together, however, they allow significant movement to enable the foot to adapt to many positions without putting undue stress on the joints. Chopart joint refers collectively to the midtarsal joints between the talus-calcaneus and the navicular-cuboid.
Talocalcaneonavicular Joint.
The talocalcaneonavicular joint is a ball-and-socket synovial joint with 3° of freedom. Its close packed position is supination, and the dorsal talonavicular ligament, bifurcated ligament, and plantar calcaneonavicular (spring) ligament support the joint (see Figure 13-1; Figure 13-2). Movements possible at this joint are gliding and rotation.
Cuneonavicular Joint.
The cuneonavicular joint is a plane synovial joint with a close packed position of supination. The movements possible at this joint are slight gliding and rotation.
Cuboideonavicular Joint.
The cuboideonavicular joint is fibrous, its close packed position being supination. The movements possible at this joint are slight gliding and rotation.
Intercuneiform Joints.
The intercuneiform joints are plane synovial joints with a close packed position of supination. The movements possible at these joints are slight gliding and rotation.
Cuneocuboid Joint.
The cuneocuboid joint is a plane synovial joint with a close packed position of supination. The movements of slight gliding and rotation are possible at this joint.
Calcaneocuboid Joint.
The calcaneocuboid joint is saddle shaped with a close packed position of supination. Supporting this joint are the bifurcated ligament, the calcaneocuboid ligament, and the long plantar ligaments. The movement possible at this joint is gliding with conjunct rotation.
Forefoot
Tarsometatarsal Joints.
The tarsometatarsal joints are plane synovial joints with a close packed position of supination. The movement possible at these joints is gliding. Taken together, these joints are referred to as Lisfranc joint.4
Intermetatarsal Joints.
The four intermetatarsal joints are plane synovial joints with a close packed position of supination. The movement possible at these joints is gliding.
Metatarsophalangeal Joints.
The five metatarsophalangeal joints are condyloid synovial joints with 2° of freedom. Their close packed position is full extension. Their capsular pattern is variable for the lateral four joints and more limitation of extension than flexion for the hallux (big toe); their resting position is 10° of extension. The movements possible at these joints are flexion, extension, abduction, and adduction.
Interphalangeal Joints.
The interphalangeal joints are synovial hinge joints with 1° of freedom. The close packed position is full extension, and the capsular pattern is more limitation of flexion than of extension. The resting position of the distal and proximal interphalangeal joints is slight flexion. The movements possible at these joints are flexion and extension.
Patient History
It is important to take a detailed and complete history when assessing the lower leg, ankle, and foot. In addition to the questions listed under the “Patient History” section in Chapter 1 the examiner should obtain the following information from the patient:
2. What was the mechanism of injury? What was the position of the foot at the time of the injury? Ankle sprains occur most often when the foot is plantar flexed, inverted, and adducted, with injury to the anterior talofibular ligament, anterolateral capsule, and possibly the distal tibiofibular ligament.5,6 This same mechanism can lead to peroneal tendon injury, a malleolar or talar dome fracture, and sinus tarsi syndrome.7,8 Figure 13-3 outlines some of the common mechanisms of injury to the ankle. Table 13-1 outlines the West Point Sprain Grading System that can be used to determine the severity of ankle sprains.9 With injury to the lateral ligaments, the structures (articular surfaces) may be damaged on the medial side owing to compression leading to medial as well as lateral pain.10 In fact, if the lateral ligaments are completely torn and the capsule disrupted, medial pain may predominate. Anterolateral pain without a history of trauma may be the result of anterior impingement especially after injury to the anterior talofibular ligament. Lin et al.11 developed a clinical prediction rule for ankle impingement (see the following box) that would preclude the need for magnetic resonance imaging (MRI). The impingement may be due to thickening of the joint capsule and/or bone spurs adjacent to the anterior talocrural joint.12 Achilles tendinosis or paratenonitis often arises as the result of overuse, increased activity, or change in a high-stress training program. Osteochondral lesions most commonly occur with trauma and may accompany ankle sprains and fractures with symptoms being exacerbated by prolonged weight bearing or high impact activities.13 A dorsiflexion injury, accompanied by a snapping and pain on the lateral aspect that rapidly diminishes, may indicate a tear of the peroneal retinaculum.14 Taunton et al.15 list some causes of overuse injuries in the lower limb.
4. Was the patient able to continue the activity after the injury? If so, the injury is probably not too severe, provided there is no loss of stability. Inability to bear weight, severe pain, and rapid swelling indicate a severe injury.14 Walking is compatible with a second-degree sprain; pain with running usually indicates a first-degree injury.16
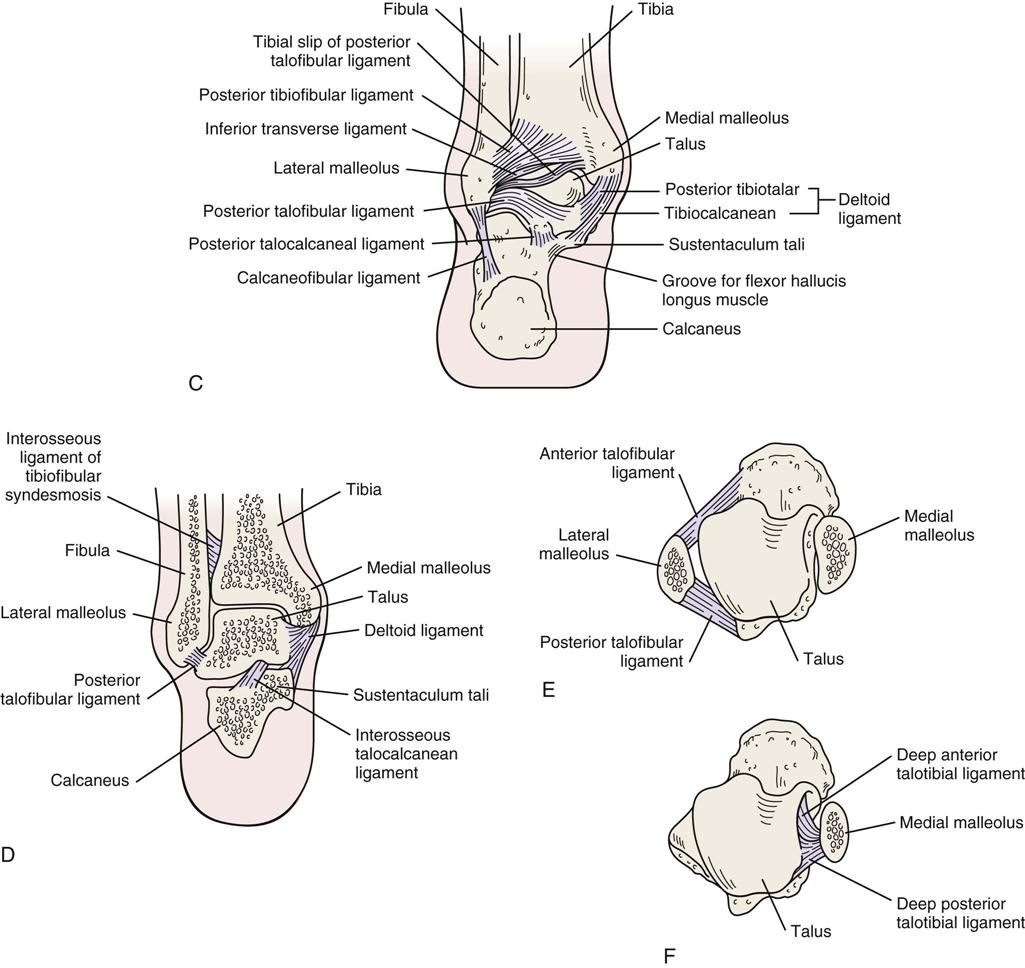
5. Was there any swelling or bruising (ecchymosis) (Figure 13-4, A)? How quickly and where did it develop? This question can elicit some idea of the type of swelling (e.g., blood, synovial, purulent) and whether it is intracapsular or extracapsular. Figure 13-4, B, shows “skate bite” in which there is swelling over the extensor tendons of the foot caused by irritation from doing up stiff ice skates too tight.
6. Are symptoms improving, becoming worse, or staying the same? It is important to know the type of onset (macrotrauma, microtrauma) and the duration and intensity of symptoms (acute, subacute, chronic). Edwards et al.17 outlined some of the chronic causes of leg pain in athletes.
7. What are the sites and boundaries of pain or abnormal sensation? The examiner should note whether the pattern is one of a dermatome, a peripheral nerve, or another painful structure. If pain and other physical findings are “out of proportion” to what would normally be expected with injury especially in the rearfoot/talar region, a more diligent examination including extra radiographic images of the talus and calcaneus may be necessary.18
10. Where is the pain? Does the patient indicate a specific location or area? For example, with shin splints (medial tibial stress syndrome) or a compartment syndrome (acute or chronic type), the patient usually indicates a diffuse area.19–22 With a stress fracture, the area of pain tends to be more specific. Anterolateral ankle impingement demonstrates anterolateral ankle joint tenderness, anterolateral ankle joint swelling (extracapsular), pain with force dorsiflexion and eversion, pain with single leg squat, pain with activities, and possible absence of ankle instability.11 Peroneal tendon problems show posterolateral pain and may be associated with lateral ankle instability.23 Plantar fasciitis is the most common cause of heel pain on the antero-medial aspect of the heel.24 It may be accompanied by a heel spur (see Figure 13-135, C), which is the result of the plantar fasciitis.
14. For active people, especially runners or joggers, the following questions should also be considered25:
a. How long has the patient been running or jogging?
b. On what type of terrain and surface does the patient train?
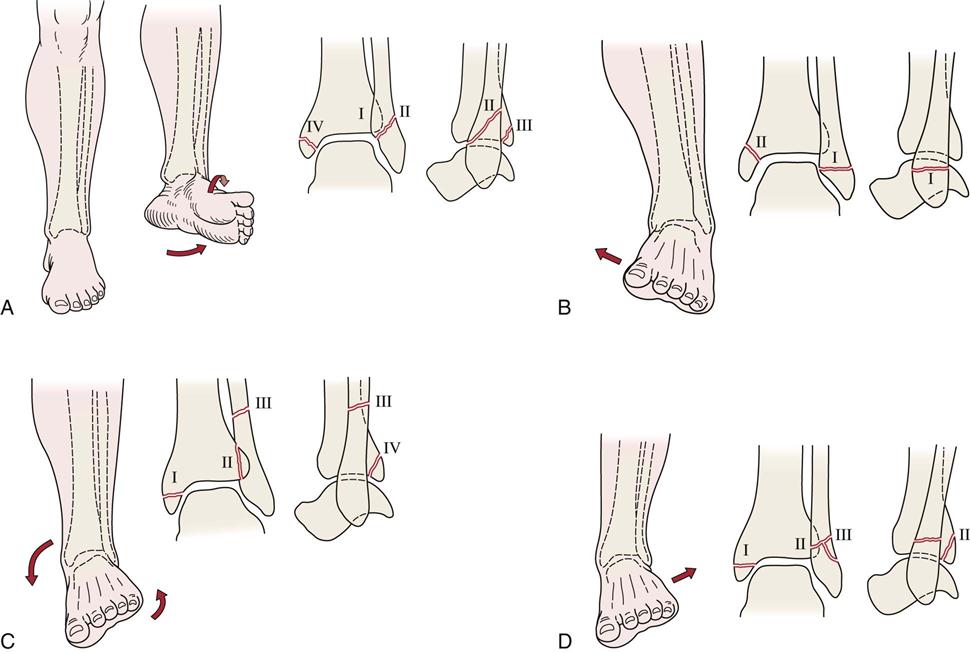
A, Supination-lateral rotation injury. Lateral rotation forces applied to a supinated foot initially result in rupture of the anterior tibiofibular ligament (stage I). As the forces continue, a short oblique fracture of the distal portion of the fibula occurs (stage II). Stage III involves a fracture of the posterior aspect of the tibia. Stage IV is a fracture of the medial malleolus. B, Supination-adduction injury. Adduction forces applied to a supinated foot initially result in a traction or avulsion fracture of the distal portion of the fibula or rupture of the lateral ligaments (stage I). As forces continue, fracture of the medial malleolus or rupture of the deltoid ligament occurs (stage II). The fibular fracture is typically transverse, and that of the medial malleolus is oblique or nearly vertical. C, Pronation-lateral rotation injury. Forces of lateral rotation applied to a pronated foot initially result in rupture of the deltoid ligament or fracture of the medial malleolus (stage I). As forces continue, the anterior tibiofibular ligament is ruptured (stage II). A high fibular fracture (stage III) and fracture of the posterior tibial margin (stage IV) are the final stages in this mechanism of injury. D, Pronation-abduction injury. The first two stages of this injury are identical to those of the pronation-external rotation fracture complex. Stage III is a transverse supramalleolar fibular fracture that may be comminuted laterally. (Redrawn from Resnick D, Kransdorf MJ: Bone and joint imaging, Philadelphia, 2005, WB Saunders, pp. 867–868.)
TABLE 13-1
The West Point Ankle Sprain Grading System
| Criterion | Grade I | Grade II | Grade III |
| Location of tenderness | Anterior talofibular ligament | Anterior talofibular ligament and calcaneofibular ligament | Anterior talofibular ligament, calcaneofibular ligament and posterior talofibular ligament |
| Edema and ecchymosis | Slight and local | Moderate and local | Significant and diffuse |
| Weight-bearing ability | Full or partial | Difficult without crutches | Impossible without significant pain |
| Ligament damage | Stretched | Partial tear | Complete tear |
| Instability | None | None or slight | Definite |
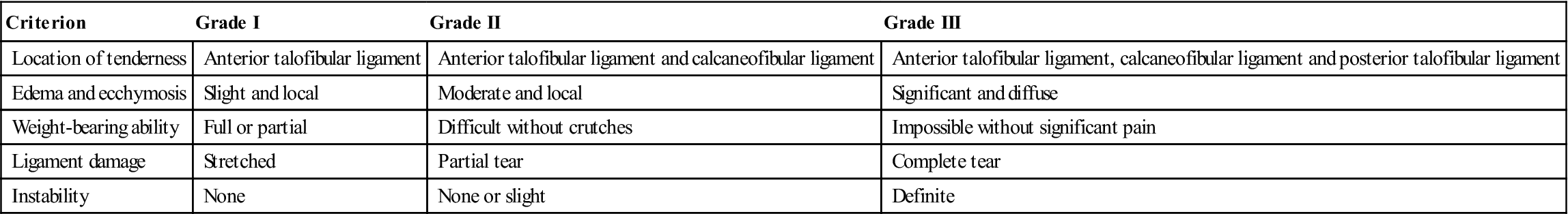
From Dutton M: Dutton’s orthopedic examination, evaluation and intervention, ed 3, New York, 2012, McGraw Hill. Data from Gerber JP, et al: Persistent disability associated with ankle sprains: a prospective examination of an athletic population. Foot Ankle Int 19:653–660, 1998.
Observation
Observation of the foot is extensive. Because of the stresses the foot is subjected to and because it, like the hand, can project signs of systemic problems and disease, the examiner should carefully and meticulously inspect the foot.
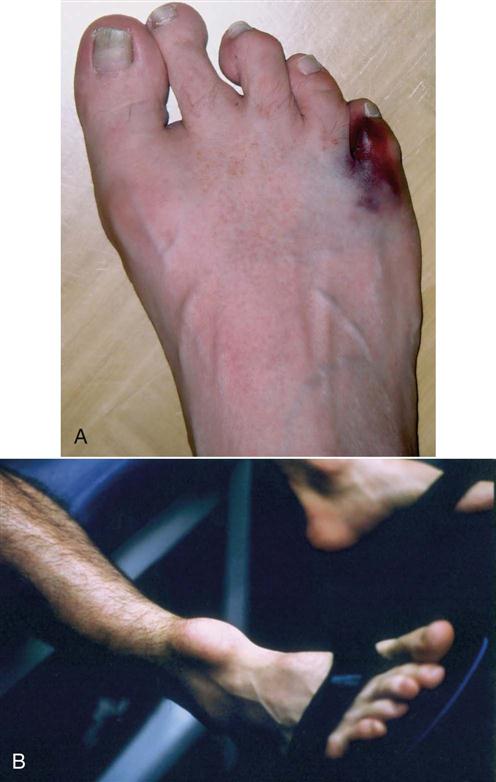
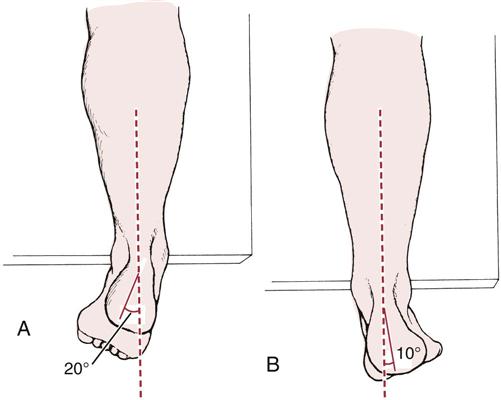
When performing the observation, the examiner should remember to compare the weight-bearing (closed-chain) with the non–weight-bearing (open-chain) posture of the foot.26 During open-chain motion, the talus is considered fixed; during closed-chain motion, the talus moves to help the foot and leg adapt to the terrain and to the stresses that are applied to the foot. Even though the calcaneus is touching a surface in closed-chain movement, for descriptive purposes, it is still considered to be moving. The weight-bearing stance of the foot shows how the body compensates for structural abnormalities (Figure 13-5). The non–weight-bearing posture shows functional and structural abilities without compensation (Figure 13-6). The observation includes looking at the patient from the front, from the side, and from behind in the weight-bearing (standing) position and from the front, from the side, and from behind in the sitting position with the legs and feet not bearing weight. The examiner should note the patient’s willingness and ability to use the feet. The bony and soft-tissue contours of the foot should be normal, and any deviation should be noted. Often, painful callosities may be found over abnormal bony prominences. The examiner should note any scars or sinuses.
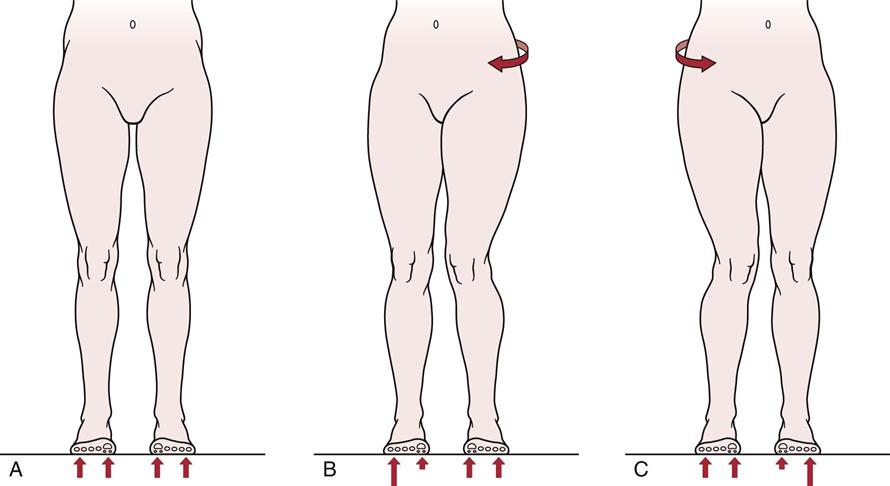
Weight-Bearing Position, Anterior View
With the patient in a standing position, the examiner should observe whether the patient’s hips and trunk are in normal position. Excessive lateral rotation of the hip or rotation of the trunk away from the opposite hip elevates the medial longitudinal arch of the foot, whereas medial rotation of the hip or trunk rotation toward the opposite hip tends to flatten the arch (Figure 13-7). Medial rotation of the hip can also cause pigeon toes, which is a condition more commonly associated with medial tibial torsion or rotation. If the iliotibial band is tight, the tightness may cause eversion and lateral rotation of the foot.
The examiner should also look at the tibia to note any local or general bone swelling (Figure 13-8). Does the tibia have a normal shape, or is it bowed? Is there any torsional deformity? The medial malleolus usually lies anterior to the lateral malleolus. Pigeon toes, or toe-in deformity, result from a medial tibial torsion deformity; it does not constitute a foot deformity (Table 13-2).
TABLE 13-2
Causes of Toeing-In and Toeing-Out in Children
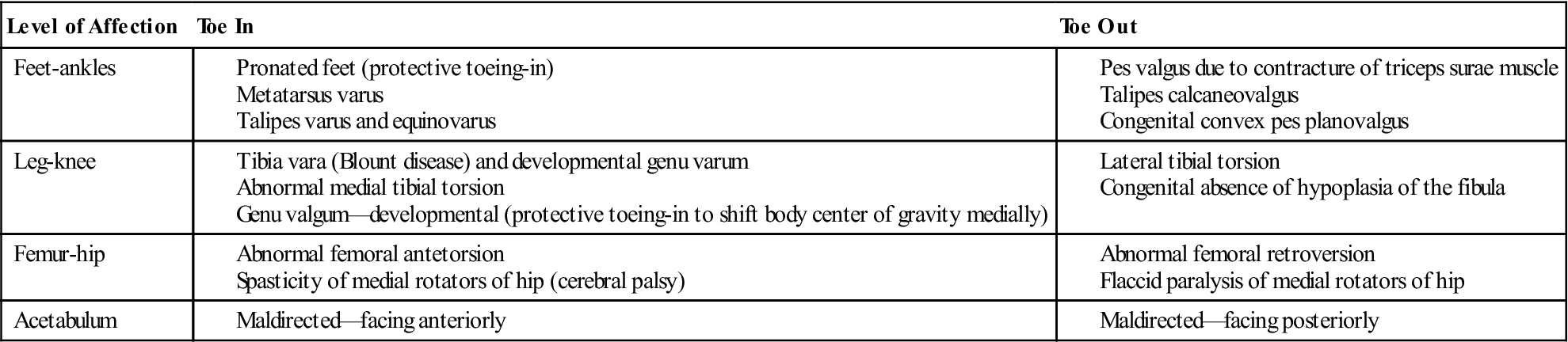
From Tachdjian MO: Pediatric orthopedics, Philadelphia, 1990, WB Saunders, p. 2817.
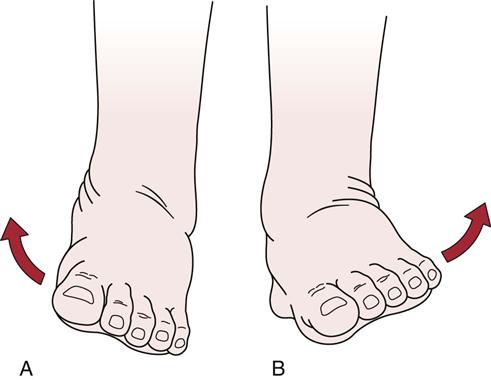
Figure 13-9 shows the anterosuperior view of the feet in the weight-bearing stance. The examiner should note whether there is any asymmetry, malalignment (Table 13-3), or excessive supination or pronation of the foot. Supination of the foot involves inversion and outward rotation of the heel, adduction of the forefoot with inward rotation at the tarsometatarsal joints to maintain contact with the ground and outward rotation at the midtarsal joints, and plantar flexion at the subtalar joint and midtarsal joints so that the medial longitudinal arch is accentuated (Figure 13-10, A). In addition, along with lateral rotation of the talus, there is lateral rotation of the leg in relation to the foot (Figure 13-11). Supination of the foot causes the proximal aspect of the tibia to move posteriorly. It is required during propulsion to give rigidity to the foot and requires less muscle work than pronation.
TABLE 13-3
Malalignment About the Foot and Ankle
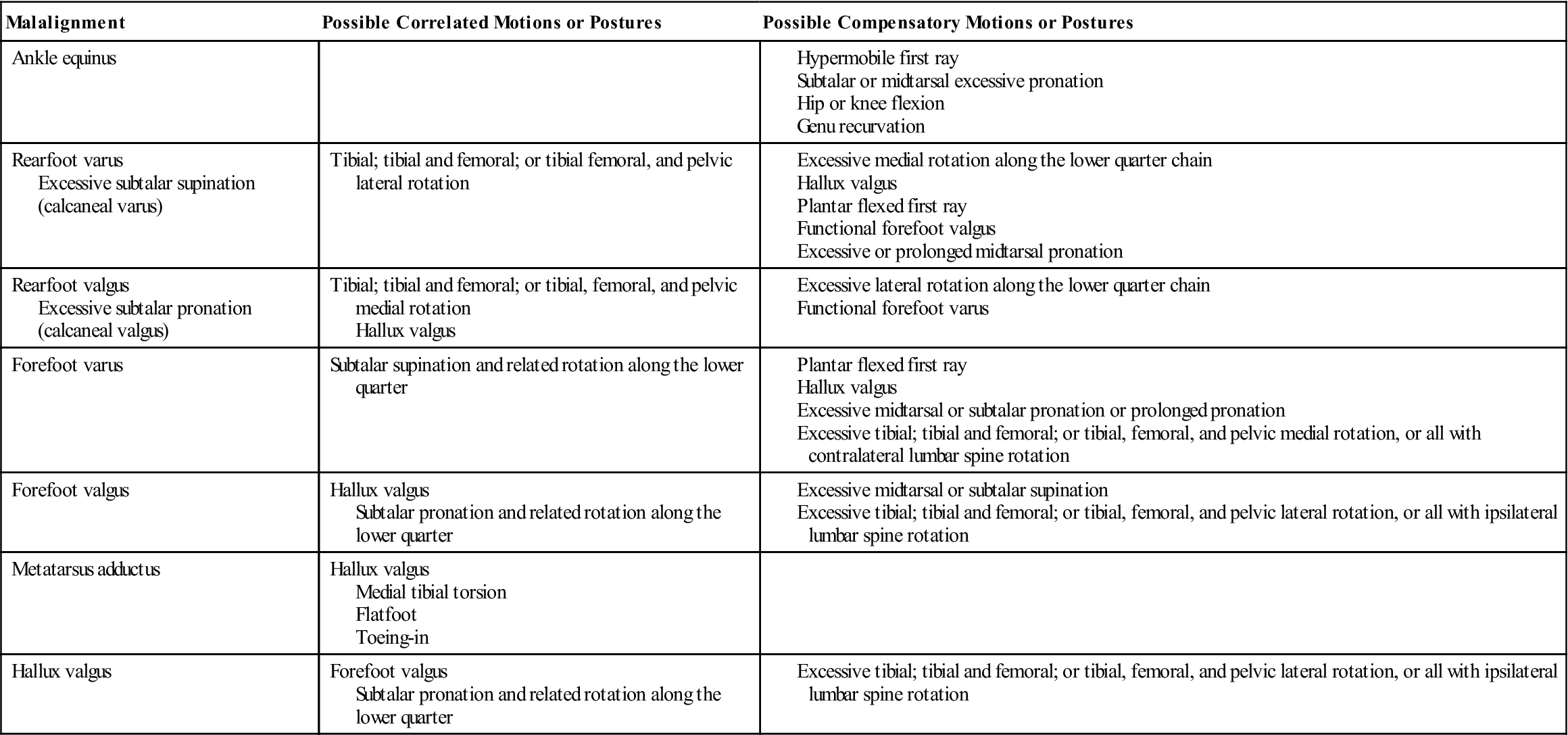
From Riegger-Krugh C, Keysor JJ: Skeletal malalignment of the lower quarter: correlated and compensatory motions and postures. J Orthop Sports Phys Ther 23:166, 1996.
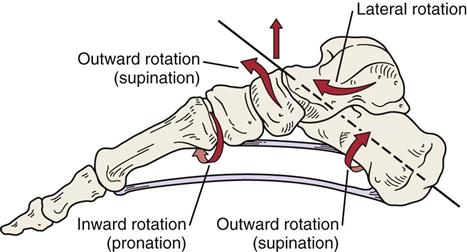
The rear foot and midfoot outwardly rotate (supinate) and the forefoot inwardly rotates (pronates) on the midfoot. As foot is plantar flexed, plantar fascia becomes tight along with ligaments to provide stable foot for push off. (Modified from Richardson JK, Iglarsh ZA, editors: Clinical orthopedic physical therapy, Philadelphia, 1994, WB Saunders, p. 513.)
Pronation of the foot involves eversion and inward rotation of the heel, abduction of the forefoot with outward rotation at the tarsometatarsal joints and inward rotation at the midtarsal joints, and medial rotation of the talus causing medial rotation of the leg in relation to the foot, and dorsiflexion of the subtalar and midtarsal joints (Figure 13-12), resulting in a decrease in the medial longitudinal arch (Figure 13-10, B). This movement causes the proximal aspect of the tibia to move anteriorly. The pronated foot has greater subtalar motion than the supinated foot and requires more muscle work to maintain stance stability than the supinated foot. The foot is much more mobile in this position.
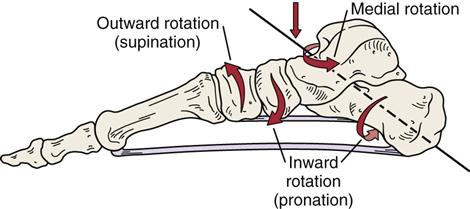
The rear foot and midfoot inwardly rotate (pronate) and the forefoot outwardly rotates (supinates) on the midfoot. Plantar fascia and plantar ligaments become taut as they absorb the ground reaction forces. (Modified from Richardson JK, Iglarsh ZA, editors: Clinical orthopedic physical therapy, Philadelphia, 1994, WB Saunders, p. 513.)
The definitions used in this chapter are the ones preferred by orthopedists and podiatrists. Anatomists and kinesiologists, such as Kapandji, refer to inversion as a combination of adduction and supination and to eversion as a combination of abduction and pronation.27 Lipscomb and Ibrahim28 and Williams and Warwick29 have defined supination and pronation as opposite the terms just mentioned. Because of the confusion in terminology concerning the terms supination and pronation, readers of books and articles on the foot must be careful to discern exactly what each author means.
In the infant, the foot is normally pronated. As the child matures, the foot begins to supinate, accompanied by development of the medial longitudinal arch. The foot also appears to be more pronated in the infant because of the fat pad in the medial longitudinal arch.
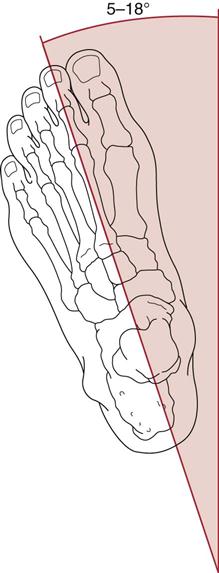
The examiner should note how the patient stands and walks. Normally, in standing, 50% to 60% of the weight is taken on the heel and 40% to 50% is taken by the metatarsal heads. The foot assumes a slight toe-out position. This angle (the Fick angle) is approximately 12° to 18° from the sagittal axis of the body, developing from 5° in children (Figure 13-13).30 Asymmetrical or excessive lateral rotation of the foot may be due to acetabular retroversion, femoral retrotorsion or femoral head neck abnormalities31 (see Chapter 11). During movement, the foot is subjected to high loading, and pathology may cause the gait to be altered. The cumulative force to which each foot is subjected during the day is the equivalent of 639 metric tons in a person who weighs approximately 90 kg, or the equivalent of walking 13 km per day.
When weight-bearing, if the relation of the foot to the ankle is normal, all of the metatarsal bones bear weight, and all of the metatarsal heads lie in the same transverse plane. The forefoot and hindfoot should be parallel to each other and to the floor. The midtarsal joints are in maximum pronation, and the subtalar joint is in neutral position. The subtalar and talocrural joints should be parallel to the floor. Finally, the posterior bisection of the calcaneus and distal one third of the leg should form two vertical, parallel lines.32
If the examiner has noted any asymmetry in standing, the examiner should place the talus (or foot) in neutral (see the “Special Tests” section) to see if the asymmetry disappears. If the asymmetry is present in normal standing, it is a functional asymmetry. If it is still present when the foot is in neutral, it is also an anatomical or structural asymmetry, in which case a structural deformity is probably causing the asymmetry. Leg-heel and forefoot-heel alignment (see the “Special Tests” section) may also be checked, especially if asymmetry is present.
The examiner should note whether the patient uses a cane or other walking aid. Use of a cane in the opposite hand diminishes the stress on the ankle joint and foot by approximately one third.
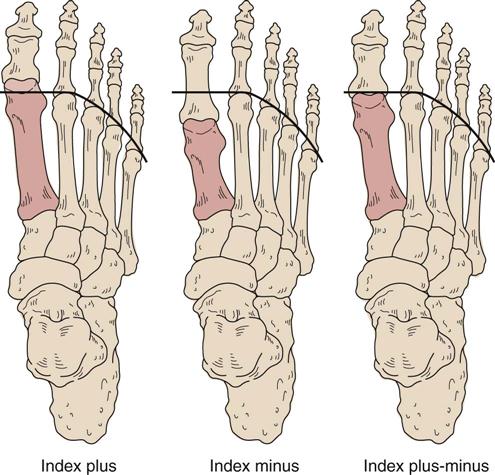
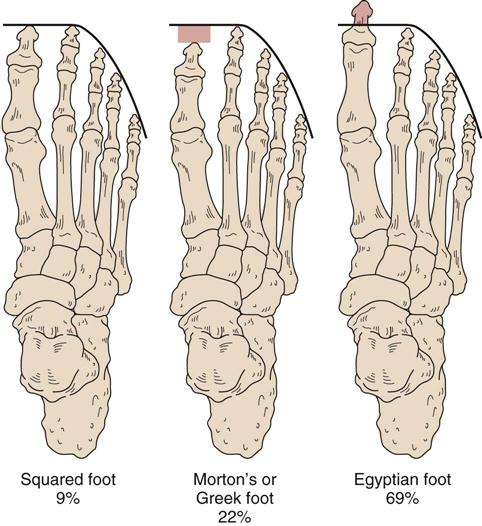
Any prominent bumps or exostoses should be noted, as should any splaying (widening) of the forefoot. Splaying of the forefoot and metatarsus primus varus is more evident in weight-bearing. There are three types of forefoot,33 based on the length of the metatarsal bones (Figure 13-14):
1. Index plus type: The first metatarsal (1) is longer than the second (2), with the others (3, 4, and 5) of progressively decreasing lengths, so that 1 > 2 > 3 > 4 > 5. This can result in an Egyptian type foot (Figure 13-15).
2. Index plus-minus type: The first metatarsal is equal in length to the second metatarsal, with the others progressively diminishing in length, so that 1 = 2 > 3 > 4 > 5. This results in a squared type foot (see Figure 13-15).
3. Index minus type: The second metatarsal is longer than the first and third metatarsals. The fourth and fifth metatarsals are progressively shorter than the third, so that 1 < 2 > 3 > 4 > 5. This results in a Morton’s or Greek type foot (see Figure 13-15).
The examiner should note whether the toenails appear normal. Older individuals have more brittle nails. The examiner should look for warts, calluses, and corns. Warts are especially tender to the pinch (but not to direct pressure), but calluses are not. Plantar warts also tend to separate from the surrounding tissues, but calluses do not. Corns are similar to calluses but have a central nidus. They may be hard (on outside or upper aspect of toes) or soft (between toes) because of moisture.
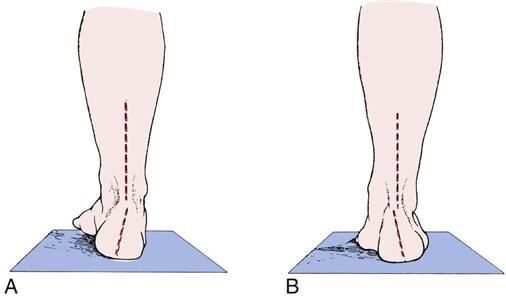
Any swelling or pitting edema within the Achilles tendon, ankle, and foot should be noted (Figure 13-16). If there is any swelling, the examiner should note whether it is intracapsular or extracapsular. Swelling above the lateral malleolus may be related to a fibular fracture or disruption of the syndesmosis (“high” ankle sprain).34,35 This injury takes a long time to heal and may involve the anterior and/or posterior tibiofibular ligament as well as the ligaments of the talocrural joint. Swelling posterior to the lateral malleolus may indicate peroneal retinacular injury. Lateral ankle sprains initially swell distal to the lateral malleolus, but swelling may spread into the foot if the capsule has been torn (Table 13-4).14 The examiner should also check the patient’s gait for the position of the foot at heel strike, at foot flat, and at toe off. The gait cycle is described in greater detail in Chapter 14.

A, Note pattern of pitting edema on top of the left foot. B, The swelling is intracapsular, as indicated by swelling on both sides of the left Achilles tendon. C, Extracapsular swelling. D, Midtarsal swelling. E, Synovial thickening (not swelling) because of repeated ankle sprains. F, Achilles swelling.