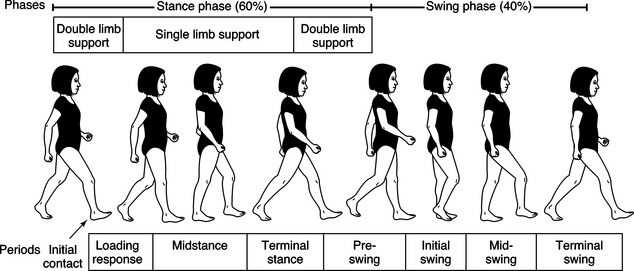
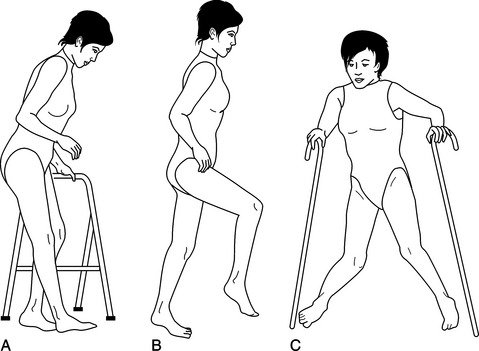
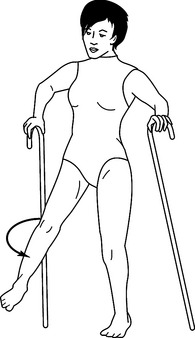
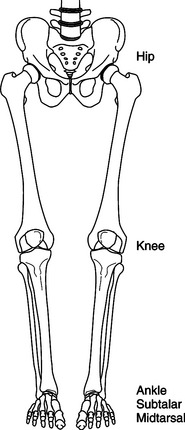
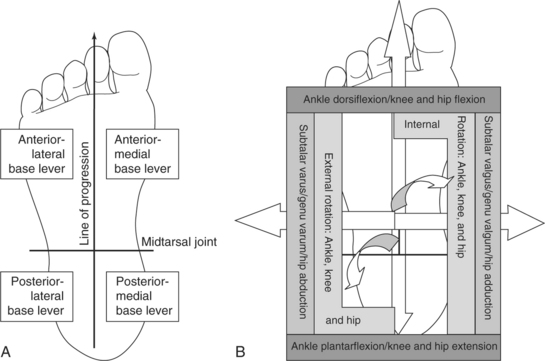
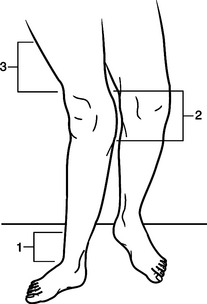
CHAPTER 17 Deanna J. Fish, MS, CPO, Michael Lohman, MEd, OTR/L, CO, Dulcey G. Lima, OTR/L, CO and Karyn Kessler, OTR/L 1 Describe the general purposes and basic functions of lower extremity orthoses. 2 Understand normal gait and pathological gait. 3 Describe the biomechanical principles of lower extremity orthoses. 4 Describe the basic design principles of lower extremity orthoses. 5 Understand the relationship between structure (i.e., anatomic alignment) and function (i.e., walking ability). 6 Understand basic terminology used in lower extremity orthotic prescriptions. 7 Describe various components and materials commonly used in the fabrication of lower extremity orthoses. 8 Recognize commonly prescribed foot, ankle/foot, knee, knee/ankle/foot, hip, and hip/knee/ankle foot orthoses. 9 Outline the role of the occupational therapist in the orthotic treatment program. 10 Summarize short- and long-term orthotic treatment objectives. 11 Understand the importance of a multidisciplinary team approach. Biomechanical and gait considerations are irrelevant when the lower extremity orthosis is rejected because it is too difficult to apply, interferes with activities of daily living, or is designed without consideration of individual strengths and weaknesses. With pediatrics, lower extremity orthoses can impact occupational performance differently and may be focused on the development of balance and equilibrium as a foundation for skill development and motor milestone acquisition. A lower extremity orthosis to position the hips may provide a stable base of support and help the child sit for longer periods of time to facilitate independent eating or writing skills. The same orthosis may not provide sufficient mobility for crawling and transitional movements unless it is designed to address these functional skills as well. An orthosis is generally identified as any orthopedic device that improves the function or structure of the body. Evidence of orthotic applications has been found as early as 2750 BCE [Bunch and Keagy 1976]. Excavation sites have uncovered mummies with various splints still intact. Historically, increased focus and advancements in orthotic design have centered on civil strife and periods of war. Today, continued advancements in the ever-expanding world of technology promote the development of new orthotic designs, materials, and components. The four basic functions of an orthosis include support and alignment, prevention or correction of deformity, substitution for or assistance of function, and reduction of pain. An orthosis is designed to address any one or all of these basic functions. Additional indications for lower extremity orthotic intervention are listed inBox 17-1. Prescription criteria for lower limb orthoses are based on a thorough pre-orthotic evaluation of the person. Components of this evaluation process are listed inBox 17-2. Observational gait assessment (OGA) is performed with the person wearing shorts and a snug T-shirt. This allows the observer to relate the function of the lower limbs to the stability of the upper torso. Walking trials are performed with the person barefoot and then with any existing orthosis or ambulation aids being used. Biomechanics laboratories can offer a detailed analysis to assist in evaluation of the person’s gait deviations with the use of force plates and high-speed cameras. However, these facilities are sparse and the cost of such a procedure is often prohibitive. Individual goals, motivation, and available social support contribute to the success of any orthotic program. Walking is a complex series of muscular interactions that manipulate the skeletal structures in specific sequential and reciprocal patterns. As a result, normal walking occurs in a mechanically effective and energy-efficient manner (Figure 17-1). The gait cycle consists of heel-strike to ipsilateral heel-strike of the same limb, covering periods of double and single limb support as well as swing. The gait cycle can be further divided into eight specific phases: initial contact, loading response, mid-stance, terminal stance, pre-swing, initial swing, mid-swing, and terminal swing [Perry 1992]. Critical events occur at each phase of gait to enhance stability and encourage functional mobility. Extensive texts are available on this topic, which is not the focus of this chapter. Therefore, a brief summary is presented in the following as it relates to lower extremity orthotic treatment programs. Limb stability is one of two basic components of walking. Each lower limb, in turn, must be effectively aligned and controlled to accept the transfer of body weight, support and balance the entire body mass independently, and then transfer the weight to the contralateral limb as it comes in contact with the ground. Sixty percent of the gait cycle is spent in periods of single and double limb support, when one and then both lower limbs support the body weight. Limb advancement is the second basic component serving to help translate the body mass forward and is dependent on the support provided by the contralateral stance limb. Swing phase accounts for 40% of the gait cycle. These actions occur reciprocally while maintaining forward momentum of the body through space with minimal metabolic costs. A pathologic gait pattern often develops secondary to neuromuscular deficits, joint instabilities, pain, disease processes, congenital involvements, and many other conditions (Figure 17-2). Excessive or insufficient joint motions occur and lead to exaggerated or inhibited movements of the body throughout the gait cycle. The normal walking speed of the individual will also be affected. Increases in energy costs tend to promote decreased walking speeds and further increases in energy costs. Most persons acquire a pattern of walking that serves a functional rather than an efficient purpose, when compared with normal parameters. For example, when dorsiflexion capabilities at the ankle are lost, a person experiences a drop-foot condition. The toes drag on the ground during swing phase and contact first with the ground during the loading phase. Persons will adopt a gait pattern that provides ground clearance for the plantar-flexed foot during swing phase. This is accomplished by excessive hip and knee flexion (i.e., steppage gait) or by excessive hip circumduction (Figure 17-3). Both of these compensations achieve a functional result; specifically, ground clearance during swing phase. Although these compensations occur without conscious thought and may allow for ambulation, the need for an orthosis is supported by increased energy costs and safety concerns. Although such clinically observable gait deviations detract from effective and efficient gait, some dysfunctional motions are more notably difficult to compensate for in a functional manner. Hyperextension (or “back knee”) is such a condition. This occurs as the knee moves in the posterior direction during mid-stance, often secondary to weakness of the quadriceps and/or posterior calf muscle groups. Without hyperextension, the person experiences uncontrolled knee flexion and collapse. As a side note, a plantar-flexion contracture is often noted upon examination as either the primary cause or result of the posterior knee moment and serves to limit tibial advancement over the base of support during stance phase. Genu recurvatum (Figure 17-4) is the long-standing result of hyperextension, when permanent damage to the posterior soft-tissue structures of the knee has occurred. This gait disruption affects the efficiency of gait because the lower extremity is forced posteriorly as the body mass is attempting to move anteriorly over the limb. Working at odds, large truncal deviations are noted and energy costs increase dramatically. Additional orthotic considerations include weight, cost, adjustability, ease of application, cosmesis (appearance), maintenance, and the necessary training required to ensure successful outcomes [Bunch et al. 1985, Kottke and Lehmann 1990]. These factors should be discussed thoroughly by the rehabilitation team and the individual before a final orthotic design is determined. All five major joints (mid-tarsal, subtalar, talocrural, knee, and hip) of the lower extremities exhibit triplanar joint motion (Figure 17-5). Still, they work together during walking to allow progression of the body in the desired direction. These motions occur largely through the sagittal plane, specifically hip and knee flexion with ankle dorsiflexion and plantar flexion. Alignment of skeletal joint levers is a critical component of efficient and effective ambulation. Mechanically speaking, the foot can be divided into anterior and posterior portions, with the mid-tarsal joint serving as the connection (Figure 17-6). Through mechanical leverage, the long anterior lever is used to control ankle dorsiflexion, knee flexion, and hip flexion. The short posterior lever limits ankle plantar flexion, knee extension, and hip extension. Medially, the first metatarsal ray and the medial heel act as medial levers to support proximal joint structures and prevent subtalar valgus and genu valgum, limit hip adduction, and discourage excessive internal rotation of the entire limb. The fifth metatarsal ray and the lateral heel serve as lateral levers to prevent subtalar varus and genu varum, limit hip abduction, and discourage excessive external rotation of the entire limb. The base levers of the foot are similar in concept to the foundation of a house. A square and true foundation always provides the best support. An unstable base of support has the potential to create larger moments of instability at proximal joint structures. For example, a pronated (flat) foot has clinically observable features: hind-foot valgus, mid-foot collapse, and forefoot abduction. Mechanical assessment reveals a loss of the anterior-medial forefoot and posterior-medial hind-foot base levers. Therefore, the ankle joint is subjected to excessive dorsiflexion, internal rotation, and medial displacement; the knee is subjected to flexion, internal rotation, and valgum moments; and the hip joint is subjected to flexion, internal rotation, and adduction moments. An effective orthotic design that returns joint stability and proper alignment to the mid-tarsal and subtalar joints will serve to effect positive alignment changes at the ankle, knee, and hip joints. As mentioned earlier, the application of force is used to effect angular changes at deviated joints. A three-point force system (Figure 17-7) effects an alignment change with two forces working in opposition to a counterforce (or fulcrum). The counterforce is positioned on the convex side of the joint deviation, close to the joint requiring an angular change. The opposite two forces are positioned proximal and distal to the counterforce, on the side of the joint concavity. The greater the linear distance between opposing forces the less pressure is required to maintain the angular correction. More challenging material selection processes involve competition between factors. The client may desire a lightweight, flexible, inexpensive, easily fabricated device to reduce foot drop. These material selections, however, will not address the underlying problems of a severe osteoarthritic ankle, which may necessitate selections the client finds unacceptable. At times, material selection focuses on a single factor that supercedes all other considerations. To reduce hypertrophic scarring that accompanies severe burns, it is essential that a continuous hard smooth surface be applied 24/7 to achieve the clinical outcome of scar prevention/reduction. The terminology for lower extremity orthoses is based on the anatomic area affected by the orthosis. An arch support or shoe insert is called a foot orthosis (FO). An orthosis designed to address drop-foot is called an ankle/foot orthosis (AFO). The orthoses may be further defined by descriptive terms such as rigid FO or thermoplastic AFO, or may be designated by the function performed such as ground reaction AFO or stance-control KAFO. Consistency in terminology ensures effective communication within the rehabilitation team. Standard abbreviations for lower limb orthoses are listed inTable 17-1. Table 17-1 Standard Abbreviations for Lower Limb Orthoses Lower extremity splints, fabricated using components that are easily assembled, may also have metal attachments. They are assembled using hand tools normally available in the splinting lab. Splints used for smaller body parts such as the arms, hands, neck, and sometimes the lower leg can be changed fairly easily as the client moves through the rehabilitation process. Some rehabilitation centers use low-temperature materials to fabricate full body splints for postoperative positioning. However, working with large sheets of plastic that easily stick together is quite cumbersome and technically demanding.
Lower Extremity Orthotics
Role of the Occupational Therapist
Definition and Historical Perspective
Purpose and Basic Function
Basic Biomechanical Principles
Walking Requirements
Normal Gait
Pathologic Gait
Functional Motions (Compensations)
Dysfunctional Motions (Detractors)
Orthotic Design Principles
Joint Alignment
Joint Stability
Three-point Force Systems
Components and Materials
Orthotic Terminology
ABBREVIATION
NAME
O
Orthosis
F
Foot
A
Ankle
K
Knee
H
Hip
FO
Foot orthosis
AFO
Ankle/foot orthosis
KO
Knee orthosis
KAFO
Knee/ankle/foot orthosis
HO
Hip orthosis
HKAFO
Hip/knee/ankle/foot orthosis
Duration of Use
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Musculoskeletal Key
Fastest Musculoskeletal Insight Engine