21
Low Median Nerve Palsy
Kevin D. Plancher
History and Clinical Presentation
A 17-year-old girl presents following operative repair of a tendon with ulnar and median nerve injuries to the distal forearm. Her surgery was ∼1 year ago. She is now unable to achieve thumb abduction or metacarpal flexion, and she has noticed severe clawing of her digits. She has been in occupational therapy for 1 year. She would like to be able to grip wide-mouthed objects, as she was once able to do.
Physical Examination
The patient cannot oppose her thumb to the little finger. Her skin is supple and there is no contracture in her first digital web space.
PEARLS
- The EIP muscle belly must be freed from surrounding soft tissue completely so that when the tendon is transferred dorsally, the muscle fibers are not angulated.
- The use of the EIP in lieu of the FDS spares the tendon for use in an intrinsic transfer if necessary.
- No pulley is required for the Burkhalter transfer.
PITFALLS
- The EIP may not be sectioned distal to the sagittal band. Loss of independence of index MP joint extension may then occur with a small extension lag at the MP joint.
- If there is an injury to the ulna distal forearm, scar may cause adhesions as it is in the path of the transfer.
- This EIP transfer just reaches the site of insertion with little or no leftover tendon. Beware, and be prepared if the transfer is short.
Diagnostic Studies
Plain radiographs were read as normal. Nerve conduction and electromyogram (EMG) were performed and revealed a combined low median and ulnar nerve palsy.
Diagnosis
The thumb is key in providing strength for prehensile pinch and grasp. Opposition is a complex motion involving abduction, flexion, and rotation of the carpometacarpal (CMC) joint and flexion and rotations of the metacarpophalangeal (MP) joint. Median nerve palsy deprives the thumb of its ability to oppose. Restoration of opposition requires the presence of transferable functioning tendons and a thumb that has adequate mobility without contractures.
At the level of the wrist, the median nerve lies between the flexor carpi radialis (FCR) and the palmaris longus tendons. The nerve lies volar to the flexor pollicis longus and the flexor digitorum profundus. The nerve then enters the carpal tunnel beneath the transverse carpal ligament. In the carpal canal the nerve may begin to branch to supply the median-innervated hand intrinsic muscles.
Surgical Management (Burkhalter EIP Transfer)
This transfer of the extensor indicis proprius (EIP) to the abductor pollicis brevis (APB) was descried by Burkhalter in 1974 and is perfect for patients with an isolated thenar paralysis due to low or high median nerve injury. The transfer achieves excellent thumb abduction, pronation, and MP flexion.
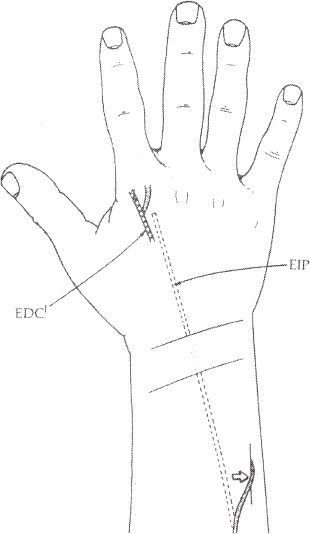
With the patient under either general or regional anesthetic, a tourniquet is applied to exsanguinate the operative extremity. The planned incisions are outlined and a longitudinal incision is made over the index MP joint. The EIP tendon is then identified ulnar to the extensor communis tendon (Fig. 21–1).
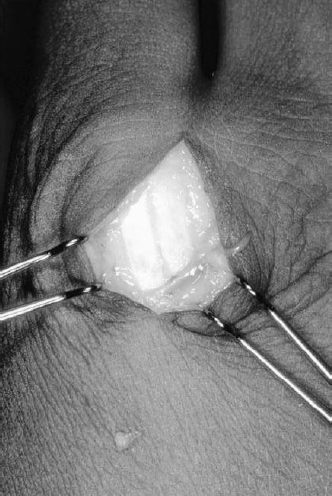
An incision is then made on the ulnar side of the EIP, through the sagittal band, and extended distally. A similar incision is made on the radial side, separating it from the extensor digitorum communis, and then connecting it to the distal incision on the ulnar side (Fig. 21–2). The sagittal band is repaired at this point in the operation to avoid an extensor lag.
Once the distal attachment of the EIP is released, a linear incision is made over the dorsal, ulnar aspect of the distal forearm and the deep fascia is divided longitudinally. The EIP tendon and muscle are identified and delivered to the proximal wound. If delivery is hampered by adhesions or connection of the EIP tendon in the dorsum of the hand, another incision may be required to free the tendon and muscle belly fully.
Once the EIP and muscle belly are freed, a small longitudinal incision is made just distal to the pisiform, and a subcutaneous tunnel is created across the forearm from the dorso-ulnar distal forearm incision to this second incision distal to the pisiform (Fig. 21–3A). Care should be taken to ensure that the tunnel is large enough to accept the muscle belly of the EIP or it may prevent full excursion of the donor tendon. The tendon can be passed through the tunnel using a tendon passer or hemostat.