Low back pain is a common problem among young athletes. These individuals are at risk for significant structural injuries or nonmechanical problems that can be associated with their symptoms. Any athlete who has severe, persisting, or activity-limiting symptoms must be evaluated thoroughly. Clinicians must have a working knowledge of the developmental issues, injury patterns, and particular conditions that may affect a given athlete and be able to work with patients in addition to families, coaches, trainers, and others involved in the care and training of the injured athlete.
Treating adolescent athletes who have low back pain (LBP) can be a challenging clinical undertaking. From a medical standpoint, adolescents cannot be thought of as merely young adults. The demographics of spinal injury in adolescents are different from those in adults, and some clinical conditions are essentially unique to the adolescent population. The ongoing growth of adolescents introduces variables into care that are not present in the management of adults. Distinct physiologic and cultural issues also affect the diagnosis and management of spinal disorders in adolescents. To treat these athletes appropriately, clinicians must have a working knowledge of spine development, injury patterns and frequencies, and the conditions that are of particular concern in these athletes while being able to manage these conditions over time. Clinicians also must be aware of the psychosocial issues affecting young athletes and be able to work with parents, coaches, and others involved in the ongoing training, support, and performance of the athlete.
The growing spine
The spine in children and adolescents has some distinct structural differences that affect the nature of injury. The nucleus pulposus of a child’s spine is relatively more hydrophilic than of an adult, resulting in more effective force absorption and a more central distribution of force transfer to the adjacent vertebrae. The composition of the nucleus pulposus begins to change as early as age 7 or 8 years, and the force distribution of the disc moves more peripherally . The vertebrae each have three primary ossification centers: one in the vertebral body and two in the vertebral arch. The latter typically fuse by 2 to 6 years, and failure of fusion results in a spina bifida occulta . Growth of the vertebral body occurs by way of the physes associated with the vertebral end plate. The vertebral end plate is composed of hyaline cartilage adjacent to the nucleus pulposus and physeal cartilage adjacent to the vertebral body. The physeal cartilage consists of a ring apophysis and an end plate physis. The ring apophysis surrounds the periphery of the vertebral body and accounts for growth of vertebral body breadth. It begins to ossify at 7 or 8 years old. The end plate physis accounts for the vertical growth of the vertebral body. These physes begin to fuse with the vertebral body at about age 14 to 15 years, with final closure occurring around age 21 to 25 years . Biomechanical studies have indicated that the bony strength of the vertebrae, particularly the neural arch, can increase into the fourth or fifth decade of life .
There are several aspects of this developmental pattern that are important in understanding injury to the young spine. The more central distribution of force by way of the nucleus pulposus combined with a relatively weak vertebral end plate may account for the relatively high frequency of end plate herniations of disc material (also termed Schmorl’s nodes) that occur in children and adolescents compared with adults. The physes themselves may be vulnerable during development, leaving adolescents at risk for apophyseal ring fractures. The relative strength of the intervertebral disc compared with that of the adjacent bone may also account for the relative reduction in rates of discogenic injuries seen in adolescents compared with adults . The incomplete bony maturation present in the neural arch also likely contributes to the occurrence of pars fractures in adolescents.
Demographics
LBP is a common occurrence in adolescents, in general, but athletes participating in a number of sports may be at a more substantial risk of pain and structural injury than age-related peers. In general-population studies, the lifetime prevalence of LBP by the midteenage years is 50% or more, with point or 1-year prevalence rates of 17% to 50% . The prevalence of LBP increases with age throughout childhood, and a number of studies have reported higher rates of LBP in girls than in boys, although this is not a uniform finding . The connection between physical activity and LBP is somewhat unclear because studies tend to differ in their findings in this regard . A study that used an accelerometer to objectively assess activity levels in children and adolescents, however, found no association between LBP and physical activity . A number of studies have identified an association between depression or other emotional problems and LBP in adolescents . A large-scale twin study also identified LBP in adolescence as a significant risk factor for LBP as an adult .
The findings in studies of adolescent athletes vary some by sport. Kujala and colleagues noted significantly higher rates of LBP in female gymnasts and figure skaters and in male hockey and soccer players compared with nonathletes (45% versus 18% over 3 years). Sward and colleagues noted that 79% of the male gymnasts they studied had a history of LBP compared with 38% of control subjects. In another study, Sward and colleagues assessed wrestlers, gymnasts, and soccer and tennis players and found that 65% of these athletes had a history of LBP, with male gymnasts having the highest frequency (85%). LBP has also been reported to be a significant problem in golfers, rowers, and rugby players, among others .
Numerous investigators have also documented high rates of structural abnormalities on imaging studies of young athletes in some sports. In their study on male gymnasts, Sward and colleagues found thoracolumbar disc degeneration on MRI in 75% of the gymnasts compared with 31% of control subjects, Schmorl’s nodes in 71% of the gymnasts compared with 44% of the control subjects, and injuries to the ring apophysis in 17% of the gymnasts compared with none of the control subjects. Similarly, Goldstein and colleagues found much higher rates of various structural abnormalities on MRI studies of elite gymnasts compared with elite swimmers. Bennett and colleagues studied elite female gymnasts with MRI and found apophyseal injuries in almost half and disc degeneration in over 60%. Iwamoto and colleagues noted structural abnormalities on plain radiographs in over 60% of the high school and collegiate football players they evaluated in one study and in 74% of the rugby players assessed in another study. A number of studies (discussed later) have also shown much higher rates of spondylolysis in high-level adolescent athletes compared with studies in the general population . Despite high levels of structural abnormalities on plain films and high rates of reported LBP for young athletes competing in a number of sports, longer-term follow-up studies on many of these athletes do not show any significant increased risk for ongoing LBP into adulthood compared with the general population .
Demographics
LBP is a common occurrence in adolescents, in general, but athletes participating in a number of sports may be at a more substantial risk of pain and structural injury than age-related peers. In general-population studies, the lifetime prevalence of LBP by the midteenage years is 50% or more, with point or 1-year prevalence rates of 17% to 50% . The prevalence of LBP increases with age throughout childhood, and a number of studies have reported higher rates of LBP in girls than in boys, although this is not a uniform finding . The connection between physical activity and LBP is somewhat unclear because studies tend to differ in their findings in this regard . A study that used an accelerometer to objectively assess activity levels in children and adolescents, however, found no association between LBP and physical activity . A number of studies have identified an association between depression or other emotional problems and LBP in adolescents . A large-scale twin study also identified LBP in adolescence as a significant risk factor for LBP as an adult .
The findings in studies of adolescent athletes vary some by sport. Kujala and colleagues noted significantly higher rates of LBP in female gymnasts and figure skaters and in male hockey and soccer players compared with nonathletes (45% versus 18% over 3 years). Sward and colleagues noted that 79% of the male gymnasts they studied had a history of LBP compared with 38% of control subjects. In another study, Sward and colleagues assessed wrestlers, gymnasts, and soccer and tennis players and found that 65% of these athletes had a history of LBP, with male gymnasts having the highest frequency (85%). LBP has also been reported to be a significant problem in golfers, rowers, and rugby players, among others .
Numerous investigators have also documented high rates of structural abnormalities on imaging studies of young athletes in some sports. In their study on male gymnasts, Sward and colleagues found thoracolumbar disc degeneration on MRI in 75% of the gymnasts compared with 31% of control subjects, Schmorl’s nodes in 71% of the gymnasts compared with 44% of the control subjects, and injuries to the ring apophysis in 17% of the gymnasts compared with none of the control subjects. Similarly, Goldstein and colleagues found much higher rates of various structural abnormalities on MRI studies of elite gymnasts compared with elite swimmers. Bennett and colleagues studied elite female gymnasts with MRI and found apophyseal injuries in almost half and disc degeneration in over 60%. Iwamoto and colleagues noted structural abnormalities on plain radiographs in over 60% of the high school and collegiate football players they evaluated in one study and in 74% of the rugby players assessed in another study. A number of studies (discussed later) have also shown much higher rates of spondylolysis in high-level adolescent athletes compared with studies in the general population . Despite high levels of structural abnormalities on plain films and high rates of reported LBP for young athletes competing in a number of sports, longer-term follow-up studies on many of these athletes do not show any significant increased risk for ongoing LBP into adulthood compared with the general population .
A general approach to the adolescent athlete who has low back pain
Any young athlete presenting with LBP who is unable to participate in his or her chosen sport because of pain needs to be thoroughly assessed for the presence of significant underlying pathology. Not only are these individuals at risk for a number of structural injuries given their age and activity levels but they are also at risk for a number of “nonmechanical” causes of LBP associated with their age, including disc space infections, neoplasms, inflammatory conditions, and developmental disorders of the spine . The development of a rational diagnostic strategy is contingent on understanding the pertinent risks for a given individual; however, vigilance and a certain degree of compulsion are necessary to keep working through potential causes of pain to exclude the more concerning options, particularly when common structural issues are not identified or when athletes are not responding as expected to what seems to be appropriate treatment.
A comprehensive history is the initial step in the evaluation of all young athletes who have LBP. A number of potential risk factors for spinal injury or LBP in athletes have been identified, although some remain controversial. These risk factors include prior low back or lower-extremity injuries, incomplete rehabilitation of prior injuries, decreased endurance, lower-extremity muscle imbalance, high number of hours of participation per week, and the occurrence of stressful life events. Additional proximate causal factors associated with sports-related injury may include the individual mechanics and skill level associated with sports performance, training patterns, and equipment or facility problems . The mode of onset, severity, and progression over time of the individual’s symptoms provide useful insight into potential causes. Symptoms that remain relatively mild for an extended period of time before presentation may be suggestive of less significant structural injuries or more indolent underlying processes, whereas more severe, acute, or progressive symptoms may suggest a more substantial structural injury or a rapidly progressive process such as infection. The nature of an athlete’s specific sport may also predispose that individual to particular problems, and the timing of injury or pain in relation to the competitive season or training cycle may be relevant for diagnosis and treatment.
Distinctions should also be made regarding additional characteristics of the symptoms. Axial LBP without lower-extremity symptoms should be viewed differently from a presentation that includes leg pain or neurologic dysfunction. The latter symptoms suggest the presence of nerve root or spinal cord involvement, which would make a diagnosis like spondylolysis without spondylolisthesis or an apophyseal injury seem less likely. Bilateral leg pain should suggest bilateral foraminal involvement (such as might be seen with a significant spondylolisthesi), central canal stenosis (such as might be seen with a disc herniation in the setting of a congenitally small spinal canal), or a spinal cord process. Lower-extremity symptoms may also arise from a number of nonspinal sources that should be considered, including diagnoses such as stress fractures, compartment syndrome, or musculotendinous injuries. Pain at night is often thought to be suggestive of an infectious or neoplastic process . The location of the back pain can significantly affect the differential diagnosis. Thoracic or thoracolumbar pain may be associated with discogenic processes or Scheuermann’s kyphosis but uncommonly associated with spondylolysis. Low lumbar pain may have many potential causes, including disc or bony sources, whereas sacral pain may be more associated with conditions such as sacroiliitis or a sacral stress fracture, although disc, bone, and nerve root processes in the lower lumbar spine may also result in pain in the sacral region. The presence or absence of associated symptoms can also be helpful in refining the differential diagnosis. Fever, lethargy, weight loss, rashes, headaches, and similar symptoms raise concern for significant systemic processes, including infection and malignancy . Morning stiffness or additional joint symptoms may suggest a diffuse inflammatory process.
A thorough history is followed by a comprehensive physical examination structured to identify significant pathology, to work through the differential diagnosis, and to aid in the development of further diagnostic and treatment plans. The physical examination should always include an examination of lumbopelvic motion, palpation of the spine and related structures, and a neurologic examination. It is important to assess a number of other factors in injured athletes, including lower-extremity alignment and function, gait and balance, specific provocative maneuvers, and components of the relevant “kinetic chain” of motion for that athlete. Clearly, other components of a comprehensive physical examination need to be included as medically appropriate. Consideration needs to be given to the potential for significant structural injury, including fracture, and the examination should always be modified appropriately for a given patient to elicit essential information while avoiding further harm.
Spinal imaging is often crucial to establishing a specific diagnosis. Clinicians must be familiar with the strengths and limitations of the different imaging modalities that are available and be comfortable with directly assessing the images. Given the relative sensitivities and specificities of the various diagnostic options, appropriate decisions need to be made regarding which studies are to be obtained, and the findings need to be interpreted in light of the history and physical examination before arriving at a diagnostic conclusion. Imaging strategies (discussed later) may be different for various clinical concerns.
Treatment of adolescent athletes involves a number of specific considerations. The state and demands of physiologic development of the athlete need to be taken into consideration when planning physical training. The psychosocial environment of an injured athlete may also pose challenges for treatment, and the psychologic impact of injury can be difficult for athletes and their families. The use of medications may be problematic. There are limited to no data on the effects on children and adolescents of a number of medications commonly used to manage pain in adults. Care needs to be taken regarding weight and age in prescribing medications to young athletes, and clinicians need to be aware of any potential conflicts with substance use policies that may apply to an athlete’s given sport or level of competition. It is unfortunate that there are high rates of use of ergogenic aids and performance-enhancing supplements among adolescent athletes, which introduce the potential for medication interactions, among other problems . The use of these supplements, legal or illegal, may not necessarily be reported to clinicians routinely, and the likelihood of this seems even lower when specific questions regarding their use are not asked.
Specific conditions
There are a number of specific clinical entities that are particularly important to understand in managing young athletes who have LBP. These conditions include spondylolysis, spondylolisthesis, discogenic injuries, and Scheuermann’s kyphosis.
Spondylolysis and spondylolisthesis
Spondylolysis should be considered a diagnostic possibility in almost every adolescent athlete who has significant LBP. In a study by Micheli and Wood , spondylolysis was the most frequent diagnosis made in adolescent athletes presenting to a sports medicine clinic with LBP. The term spondylolysis refers to a defect in the pars interarticularis of the vertebral arch. Spondylolisthesis is a separate but related term referring to the anterior displacement of a vertebral body on the one subjacent to it ( Fig. 1 ). Spondylolysis and spondylolisthesis are most frequently viewed under the categorization proposed by Wiltse and colleagues , in which the term isthmic spondylolysis is used to identify patients who have sustained a lesion in the pars. It is generally believed that the pars lesion in isthmic spondylolysis represents a fatigue fracture of the bone, and most pars lesions identified (85%–95%) occur at L5 . In a study of 4243 young athletes who had LBP, Rossi and Dragoni found that about one half of those who had spondylolysis also had concurrent spondylolisthesis. Significant progression of an associated spondylolisthesis is uncommon. There are data to indicate that sports participation does not increase the risk of progression of a low-grade slip . When slip progression occurs, it is usually does so during the adolescent growth spurt, typically without any symptoms, and affected individuals need to be monitored radiographically through adolescence.
Studies in the general population have shown pars lesions to be a relatively common finding. Fredrickson and colleagues prospectively studied 500 first-grade students with plain radiographs and found an overall prevalence of spondylolysis of 4.4% at age 6 years. All of these lesions occurred without any symptoms. This number increased to 5.2% by age 12 years and to 6% by adulthood. Roche and Rowe studied 4200 cadaveric spines and found an overall prevalence of 4.2%. The numbers are different in athletes, however, with large-scale studies of adolescent athletes showing rates of 8% to 14% . Athletes participating in certain sports have much higher frequencies of spondylolysis than others. Some of the sports with the highest reported frequencies of pars lesions include gymnastics, weight lifting, throwing track and field sports, diving, wrestling, cricket, and crew . Sports that involve frequent flexion/extension motions of the lumbar spine, particularly when combined with rotation, may place athletes at more risk for pars fractures.
History and physical examination can be helpful in establishing the diagnosis, although by definition, spinal imaging is essential. Symptomatic spondylolysis typically presents with axial LBP without radiation into the legs. The pain can come on acutely after a specific traumatic event (or even a relatively mundane event) or may progress gradually over time. The pain is usually worsened by activity and improves with rest. It is common to see the symptoms begin toward the end of one sports season, subside after the season, and then return when the athlete starts training for the next season. The pain can lateralize to the side of the lesion or be more generalized in the low back. Leg pain, paresthesias, or neurologic loss are not consistent with isolated spondylolysis and should suggest the presence of spondylolisthesis or other diagnoses in young athletes. There are no pathognomonic findings on physical examination for a pars lesion. The one-legged hyperextension maneuver (in which the patient stands on one leg and leans backward) has been proposed as a means of identifying the presence of a pars lesion, but a recent study on this test concluded that it was relatively unhelpful and had low sensitivity and specificity .
A number of diagnostic imaging modalities are available for evaluating the pars in an athlete who has suspected spondylolysis, and significant controversy exists regarding the optimal imaging strategy. Given the relatively high prevalence of asymptomatic pars lesions in adolescent athletes, it is not enough just to visualize a pars lesion. Ideally, the pars defect needs to be identified as the source of pain, and information on the potential for the lesion to heal should be obtained. In practical application, this means that multiple imaging studies are usually required to diagnose and treat athletes who have spondylolysis.
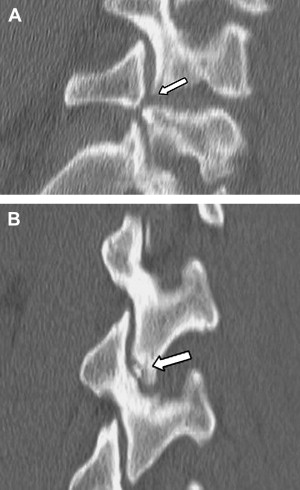
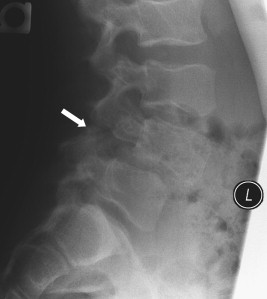
Plain radiography has been used in diagnosing pars lesions for some time and is the basis for diagnosis and follow-up in a large number of published studies. Nuclear imaging with bone scan with or without single-photon emission CT (SPECT), CT, and MRI have been shown to be more sensitive than plain radiography in the identification of pars lesions . Typically, spondylolysis appears on plain radiographs as a lucency in the area of the pars (see Fig. 1 ). On oblique films, this lesion is characteristically described as a fracture “in the neck of the Scotty dog.” In current use, the ability to identify and follow a spondylolisthesis may actually be the most important role of plain films in managing adolescents who have spondylolysis.
Radionuclide imaging, particularly SPECT, can be very helpful in the diagnostic evaluation of adolescent athletes who have LBP. Numerous studies have shown bone scan and SPECT to be more sensitive than plain radiography in the diagnosis of spondylolysis, and they appear to be superior to MRI and CT in this regard . There are multiple studies that have shown that a positive bone scan or SPECT correlates with a symptomatic pars lesion , making SPECT a particularly useful screening tool in adolescent athletes who have LBP. A significant limitation in the use of radionuclide imaging, however, is specificity. Not all of the abnormalities seen in the posterior elements of adolescents on SPECT or bone scan represent pars lesions . Additional imaging, particularly with CT, is generally required to clarify the bony abnormality in a patient who has a positive SPECT study ( Fig. 2 A, B and Fig. 3 A).