With the exception of Rhode Island, all states require high school athletes to undergo a preparticipation examination. These examinations may vary from state to state, however. This article covers the basics of the history, physical examination, special tests, and issues surrounding clearance for various diagnoses.
Each year over 7 million high school students participate in school-sponsored sports programs . With the exception of Rhode Island, all states require a high school athlete to undergo a preparticipation examination (PPE); however, there is no uniform national standard regarding this common evaluation. In addition, states vary greatly as to who is allowed to perform the PPE. A few states allow clinicians other than physicians, including nurse practitioners, chiropractors, and physician assistants, to complete the examination and necessary paperwork.
The primary goal of the PPE is to make sports participation as safe as possible. The PPE attempts to identify any life-threatening (eg, cardiovascular defects) or potentially disabling conditions (eg, cervical stenosis) that may place a young athlete at risk on the playing field. Second, it aims to identify any orthopedic conditions that may predispose to injury (eg, shoulder instability) or medical conditions that may be worsened by sports participation (eg, exercise-induced asthma). A third major objective of the PPE is to fulfill state and local legal requirements for scholastic sports participation.
Several secondary objectives may be attained, depending on the specific goals and available resources of the medical staff, school, or community. These potential secondary goals include assessment of general health, fitness and performance assessment (eg, body composition, flexibility), and counseling on health-related matters. Studies indicate that a large number of adolescents use the PPE as their yearly health maintenance examination . Therefore some clinicians advocate that the PPE serve other purposes including screening for high-risk behaviors, violence and safety issues, tobacco/drug and alcohol use, sexuality, and emotional issues. Adolescent screening questionnaires, available from the American Medical Association at www.ama-assn.org/ama/pub/category/1980.html , may be used to help identify issues requiring further follow-up. Finally, simply notifying the parent(s) of the limitations of a screening PPE may encourage future follow-up care with the primary care physician.
Timing and location
The timing, location, and skill sets of the examiner(s) all impact the effectiveness of the PPE. Ideally, the examination should be done at least 4 to 6 weeks before the start of the sports season to allow time to address and correct any identified problems. The PPE typically is performed in one of two settings: an office-based examination by a primary care physician, or a mass screening station examination using multiple examiners. Each method has its own strengths and weakness, and it is important for examining physicians to anticipate the potential disadvantages of the method used ( Table 1 ) . With the athlete and/or parents’ permission, anticipated medical problems and treatment plans should be discussed with sideline medical personnel, including coaches and athletic trainers.
| Advantages | Disadvantages | |
|---|---|---|
| Office-based | Established doctor–patient relationship | Variability of sports medicine interest and knowledge |
| Follow-up care | Limited communication with team staff | |
| Private setting | Limited access | |
| Personal health counseling | Cost | |
| Communication with parents | ||
| Station-based | Can use multiple specialized personal | Incomplete past medical history |
| Time-efficient | No prior physician–patient relationship | |
| Cost-efficient | Lack of privacy | |
| School-based station examination can include coaches and athletic trainers. | Lack of continuity/follow-up issues | |
| Communication with school | Communication with parents |
The history
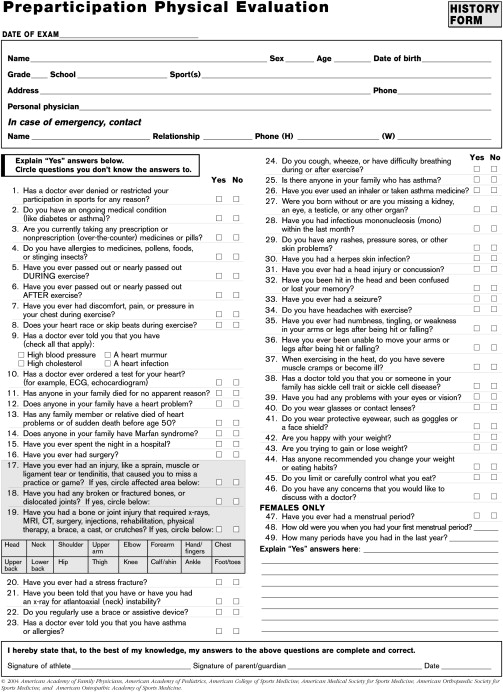
The most sensitive part of the evaluation is a thorough history. The history alone identifies approximately 75% of problems that may affect participation . Several medical organizations (American Academy of Pediatrics [AAP], American Academy of Family Physicians, AMSSM, AOSSM and AOASM) have published a monograph on the PPE (available at http://www.aap.org/bookstore/ ), which includes the medical history that is most pertinent to the young athlete. Previous studies have shown that an adolescent’s recall about his or her past medical history is often incomplete . Ideally, these forms should be completed by the parent first and then by the student athlete to respect privacy and obtain an accurate history ( Fig. 1 ).
The past medical history should focus on past surgeries and major illnesses or chronic medical conditions that may be worsened by training and competition. Questions regarding previous illness or conditions should focus on hospitalizations or emergency room visits, adequacy of control of symptoms, and any current functional deficits. Athletes who have well-managed medical conditions, such as diabetes, asthma, and seizure, can participate in sports safely. The AAP has published extensive guidelines regarding medical conditions and sports participation. Table 2 highlights these guidelines, as does the section on medical clearance later in this article.
| Condition | May participate |
|---|---|
| Atlantoaxial instability (instability of the joint between cervical vertebrae 1 and 2) | Qualified yes |
| Explanation: Athlete needs evaluation to assess risk of spinal cord injury during sports participation. | |
| Bleeding disorder | Qualified yes |
| Explanation: Athlete needs evaluation. | |
| Cardiovascular disease | |
| Carditis (inflammation of the heart) | No |
| Explanation: Carditis may result in sudden death with exertion. | |
| Hypertension (high blood pressure) | Qualified yes |
| Explanation: Those with significant essential (unexplained) hypertension should avoid weight and power lifting, body building, and strength training. Those with secondary hypertension (hypertension caused by a previously identified disease) or severe essential hypertension need evaluation. The National High Blood Pressure Education Working group defined significant and severe hypertension. | |
| Congenital heart disease (structural heart defects present at birth) | Qualified yes |
| Explanation: Those with mild forms may participate fully; those with moderate or severe forms or who have undergone surgery need evaluation. The 26th Bethesda Conference defined mild, moderate, and severe disease for common cardiac lesions. | |
| Dysrhythmia (irregular heart rhythm) | Qualified yes |
| Explanation: Those with symptoms (chest pain, syncope, dizziness, shortness of breath, or other symptoms of possible dysrhythmia) or evidence of mitral regurgitation (leaking) on physical examination need evaluation. All others may participate fully | |
| Heart murmur | Qualified yes |
| Explanation: If the murmur is innocent (does not indicate heart disease), full participation is permitted. Otherwise, the athlete needs evaluation (see congenital heart disease and mitral valve prolapse). | |
| Cerebral palsy | Qualified yes |
| Explanation: Athlete needs evaluation. | |
| Diabetes mellitus | Yes |
| Explanation: All sports can be played with proper attention to diet, blood glucose concentration, hydration, and insulin therapy. Blood glucose concentration should be monitored every 30 minutes during continuous exercise and 15 minutes after completion of exercise. | |
| Diarrhea | Qualified no |
| Explanation: Unless disease is mild, no participation is permitted, because diarrhea may increase the risk of dehydration and heat illness. See fever. | |
| Eating disorders | Qualified yes |
| Anorexia nervosa | |
| Bulimia nervosa | |
| Explanation: Patients with these disorders need medical and psychiatric assessment before participation. | |
| Eyes | Qualified yes |
| Functionally one-eyed athlete | |
| Loss of an eye | |
| Detached retina | |
| Previous eye surgery or serious eye injury | |
| Explanation: A functionally one-eyed athlete has a best-corrected visual acuity of less than 20/40 in the eye with worse acuity. These athletes would suffer significant disability if the better eye were seriously injured, as would those with loss of an eye. Some athletes who previously have undergone eye surgery or had a serious eye injury may have an increased risk of injury because of weakened eye tissue. Availability of eye guards approved by the American Society for Testing and Materials and other protective equipment may allow participation in most sports, but this must be judged on an individual basis. | |
| Fever | No |
| Explanation: Fever can increase cardiopulmonary effort, reduce maximum exercise capacity, make heat illness more likely, and increase orthostatic hypertension during exercise. Fever may rarely accompany myocarditis or other infections that may make exercise dangerous. | |
| Heat illness, history of | Qualified yes |
| Explanation: Because of the increased likelihood of recurrence, the athlete needs individual assessment to determine the presence of predisposing conditions and to arrange a prevention strategy. | |
| Hepatitis | Yes |
| Explanation: Because of the apparent minimal risk to others, all sports may be played that the athlete’s state of health allows. In all athletes, skin lesions should be covered properly, and athletic personnel should use universal precautions when handling blood or body fluids with visible blood. | |
| Human immunodeficiency virus infection | Yes |
| Explanation: Because of the apparent minimal risk to others, all sports may be played that the athlete’s state of health allows. In all athletes, skin lesions should be covered properly, and athletic personnel should use universal precautions when handling blood or body fluids with visible blood. | |
| Kidney, absence of one | Qualified yes |
| Explanation: Athlete needs individual assessment for contact, collision, and limited-contact sports. | |
| Liver, enlarged | Qualified yes |
| Explanation: If the liver is acutely enlarged, participation should be avoided because of risk of rupture. If the liver is chronically enlarged, individual assessment is needed before collision, contact, or limited-contact sports are played. | |
| Malignant neoplasm | Qualified yes |
| Explanation: Athlete needs individual assessment. | |
| Musculoskeletal disorders | Qualified yes |
| Explanation: Athlete needs individual assessment. | |
| Neurologic disorders | |
| History of serious head or spine trauma, severe or repeated concussions, or crainotomy. | Qualified yes |
| Explanation: Athlete needs individual assessment for collision, contact, or limited-contact sports and also for noncontact sports if deficits in judgment or cognition are present. Research supports a conservative approach to management of concussion. | |
| Seizure disorder, well-controlled | Yes |
| Explanation: Risk of seizure during participation is minimal | |
| Seizure disorder, poorly controlled | Qualified yes |
| Explanation: Athlete needs individual assessment for collision, contact, or limited-contact sports. The following noncontact sports should be avoided: archery, riflery, swimming, weight or power lifting, strength training, or sports involving heights. In these sports, occurrence of a seizure may pose a risk to self or others. | |
| Obesity | Qualified yes |
| Explanation: Because of the risk of heat illness, obese persons need careful acclimatization and hydration. | |
| Organ transplant recipient | Qualified yes |
| Explanation: Athlete needs individual assessment. | |
| Ovary, absence of one | Yes |
| Explanation: Risk of severe injury to the remaining ovary is minimal. | |
| Respiratory conditions | |
| Pulmonary compromise, including cystic fibrosis | Qualified yes |
| Explanation: Athlete needs individual assessment, but generally, all sports may be played if oxygenation remains satisfactory during a graded exercise test. Patients with cystic fibrosis need acclimatization and good hydration to reduce the risk of heat illness. | |
| Asthma | Yes |
| Explanation: With proper medication and education, only athletes with the most severe asthma will need to modify their participation. | |
| Acute upper respiratory infection | Qualified yes |
| Explanation: Upper respiratory obstruction may affect pulmonary function. Athlete needs individual assessment for all but mild disease. See fever. | |
| Sickle cell disease | Qualified yes |
| Explanation: Athlete needs individual assessment. In general, if status of the illness permits, all but high exertion, collision, and contact sports may be played. Overheating, dehydration, and chilling must be avoided. | |
| Sickle cell trait | Yes |
| Explanation: It is unlikely that persons with sickle cell trait have an increased risk of sudden death or other medical problems during athletic participation, except under the most extreme conditions of heat, humidity, and possibly increased altitude. These persons, like all athletes, should be carefully conditioned, acclimatized, and hydrated to reduce any possible risk. | |
| Skin disorders (boils, herpes simplex, impetigo, scabies, molluscum contagiosum) | Qualified yes |
| Explanation: While the patient is contagious, participation in gymnastics with mats; martial arts; wrestling; or other collision, contact, or limited-contact sports is not allowed. | |
| Spleen, enlarged | Qualified yes |
| Explanation: A patient with an acutely enlarged spleen should avoid all sports because of risk of rupture. A patient with a chronically enlarged spleen needs individual assessment before playing collision, contact, or limited-contact sports. | |
| Testicle, undescended or absence of one | Yes |
| Explanation: Certain sports may require a protective cup. |
∗ This table is designed for use by medical and nonmedical personnel. “Needs evaluation” means that a physician with appropriate knowledge and experience should assess the safety of a given sport for an athlete with the listed medical condition. Unless otherwise noted, this is because of variability of the severity of the disease, the risk of injury for the specific sports.
The history
The most sensitive part of the evaluation is a thorough history. The history alone identifies approximately 75% of problems that may affect participation . Several medical organizations (American Academy of Pediatrics [AAP], American Academy of Family Physicians, AMSSM, AOSSM and AOASM) have published a monograph on the PPE (available at http://www.aap.org/bookstore/ ), which includes the medical history that is most pertinent to the young athlete. Previous studies have shown that an adolescent’s recall about his or her past medical history is often incomplete . Ideally, these forms should be completed by the parent first and then by the student athlete to respect privacy and obtain an accurate history ( Fig. 1 ).









