CHAPTER 83 Loose Bodies
INTRODUCTION
First described in the knee by Ambroise Paré32 in 1558, loose bodies occur in the elbow with a frequency second only to that in the knee.33 As in other joints, it is sometimes difficult to distinguish with certainty between ossification centers and acquired lesions (Box 83-1).5
ACCESSORY OSSIFICATION
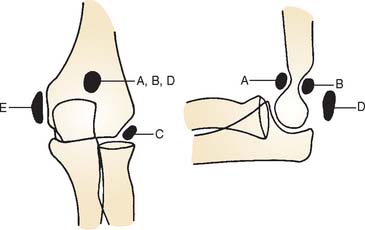
Confusion with acquired processes is caused by accessory ossicles that occur at the elbow as normal variations. Three sites for accessory ossicles about the elbow have been described: distal to the medial epicondyle; proximal to the tip of the olecranon (the patella cubiti); and in the olecranon fossa (the os supratrochleare dorsale8) (Fig. 83-1).
MEDIAL EPICONDYLE ACCESSORY OSSICLE
An accessory ossicle to the medial epicondyle19 is sometimes seen as a smooth, rounded ossification just distal to this structure. Because calcification can follow injury to the medial collateral ligament, whether the radiographic lesion reflects a traumatic or a congenital insult is often confusing,40 possibly more than at any other site. However, a discrete, rounded, smooth ossicle in patients who have no history of injury to this region suggests an accessory structure (Fig. 83-2). An irregular or misshapen medial epicondyle suggests a traumatic origin. Nevertheless, the formation of a fully developed medial epicondyle does not necessarily prove the diagnosis, because in a child, the medial epicondyle can remodel and appear normal in later years.

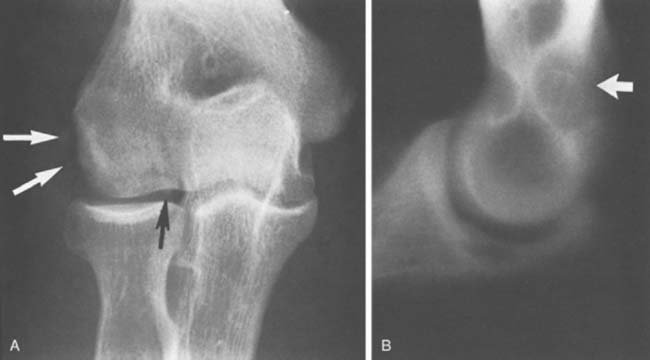
FIGURE 83-2 A, The occurrence of a smooth ossicle at the inferior aspect of the medial epicondyle without a history of injury represents an accessory ossicle. B, An earlier medial epicondyle fracture may have the same appearance, but the epicondyle may remodel in young patients (see Chapter 16). Note the loose bodies in the olecranon fossa.
PATELLA CUBITI
The so-called patella cubiti is rare but has been thoroughly described in earlier literature,16,20,37 and a thorough review has been presented by Habbe.16 This ossicle occurs in the triceps tendon near its insertion and is considered a true sesamoid bone.21 The proximal position is so characteristic in appearance that there should be little doubt about its origin (Fig. 83-3A). This structure should be distinguished from an avulsed olecranon apophysis, which appears farther distal (see Fig. 83-3B), and from a calcified olecranon bursa. Because of its superficial location, this ossicle may be subject to direct trauma and even fracture,4 but the injury generally responds to symptomatic treatment. Confusion with a fractured olecranon spur may exist.
OS SUPRATROCHLEARE DORSALE
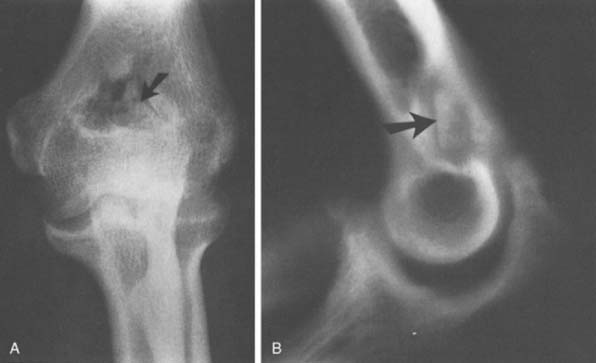
The radiographic density observed in the olecranon fossa has been a source of controversy. Characteristically, the ossicle has a smooth and round or oval shape that is often best seen in the lateral projection but is also demonstrated in the anteroposterior view (Fig. 83-4). In early descriptions of this entity it was considered to be a form of osteochondritis dissecans of the trochlea.29 The precise origin of this osseous structure is still the subject of some discussion, and trauma is often blamed.2 The supposed mechanism of injury is that with hyperextension, impaction of the tip of the olecranon into the olecranon fossa may cause a spur to develop at the tip of the olecranon. Conceivably it can be dislodged, form a nidus and grow into the characteristic os supratrochleare. Certainly, this mechanism has been implicated in the formation of loose bodies in the olecranon fossa (Fig. 83-5).39 The problem has been discussed in detail and clarified by Obermann and Loose, who concluded that the os supratrochleare dorsale is most likely a congenital accessory bone.30 Rather than being caused by trauma, it is subject to injury that produces secondary chondrometaplasia and resulting symptoms. When this occurs, the ossicle may look damaged and have an irregular margin.
Thus, the distinction between an ossicle caused by trauma and an existing one subjected to trauma remains obscure (see Fig. 83-5). Regardless of the source, the treatment is obvious. Mere radiographic evidence of the osseous density does not imply that it needs to be removed. If it is painful owing to injury caused by hyperextension or a direct blow, symptomatic treatment should resolve the pain. If catching, locking, or persistent pain is present, the ossicle is easily excised through a limited posterolateral incision or, preferably, arthroscopically (see Chapter 38).31
ACQUIRED LOOSE BODIES
Loose or pedunculated cartilaginous or osseocartilaginous bodies are believed to originate from a small nidus.33 The sequence of morphologic alterations that ensue is common to all free bodies, regardless of their origin.25 Surface proliferation of chondroblasts and osteoblasts nourished by the synovial fluid creates a laminar or layered effect that is seen in about 87% of such bodies that are predominantly cartilaginous and in 80% of those that are predominantly osseous (Fig. 83-6).25The growth process continues as long as the free or pedunculated body is exposed to the synovial fluid.
ETIOLOGY
Our understanding of intra-articular loose bodies has been much enhanced by the work of Milgram.24–26 By clinical findings and presentation, acquired free or pedunculated bodies can be divided into three groups: (1) osteochondral fractures, (2) degenerative disease of the articular surface, and (3) a proliferative disorder of the synovium, synovial chondromatosis. Milgram25 defines three types of cartilage associated with loose bodies based on their supposed site of origin: (1) articularcartilage cells, (2) osteophytic cells from a proliferating osteophyte in a degenerative joint, and (3) lobular cartilage from the synovial lining cell. Pathologically, these loose bodies can originate from a joint fracture, from degenerative osteophytes, or de novo as a proliferative disease of the synovium.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree