Ligamentous Repair for Acute Scapholunate Dissociation
Steven F. Viegas
Indications and Contraindications
Acute scapholunate dissociation is the most frequently recognized carpal instability. The prime indication for workup and treatment of acute scapholunate dissociation is a history of a traumatic injury to the wrist that has occurred within 3 weeks of presentation in which the injury, physical findings, and radiographic studies are consistent with this condition.
A relative indication is a wrist initially evaluated at a later interval—3 weeks to 3 months after the injury. Trauma that occurred 3 months or longer before presentation is not categorized as acute, but is not a contraindication for treatment.
Radiographic or arthroscopic findings of arthritis in the radioscaphoid or capitolunate joint contraindicate treatment of the injury with the method described here.
Acute scapholunate dissociation that has other associated ligamentous disruptions or carpal fractures is a relative contraindication to the technique described here. There should be a high index of suspicion for ligamentous injury and possible carpal instabilities with any significant wrist injury, including distal radius fractures. The associated injuries do not preclude treating scapholunate dissociation in the same way, but it is necessary to assess scapholunate dissociation in light of other associated injuries and to modify the treatment plan appropriately.
Preoperative Planning
History and Physical Examination
The history reveals whether the magnitude of trauma was sufficient to result in injury to the ligaments of the wrist. Typically, the mechanism of injury that results in scapholunate dissociation is a hyperextension force to the wrist with concomitant forearm pronation and intracarpal supination.
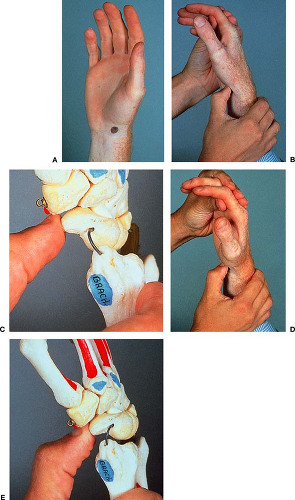
Focus the physical examination on both the injured and the uninjured extremities. The contralateral side provides an excellent normal baseline for the patient’s range of motion and level of constitutional ligamentous laxity. When attempting to assess whether acute scapholunate dissociation exists, elicit tenderness at the level of the scapholunate joint, particularly at its dorsal aspect, 1 cm
distal to Lister’s tubercle. The Watson test or scaphoid stress test is also useful to detect abnormal mobility of the scaphoid (1) (Fig. 19-1). Occasionally, during this test a painful, audible snap is elicited, which is diagnostic of this condition.
distal to Lister’s tubercle. The Watson test or scaphoid stress test is also useful to detect abnormal mobility of the scaphoid (1) (Fig. 19-1). Occasionally, during this test a painful, audible snap is elicited, which is diagnostic of this condition.
Radiographic Diagnosis
Obtain radiographs, including standard posteroanterior (PA), lateral, radial deviation, ulnar deviation, oblique, and anteroposterior (AP) supinated, clenched-fist radiographs of the wrist and hand. Obtain radiographs of the contralateral wrist for comparison. Significant scapholunate dissociation results in a carpal instability dissociative type of lesion that typically appears as a dorsal intercalated segment instability (DISI) pattern of carpal malalignment. This carpal instability pattern includes the following radiologic features:
Scapholunate gap: The intercarpal distance between the scaphoid and lunate on the AP radiograph is increased compared with the other intercarpal spacing. A scapholunate gap greater than 3 mm is considered diagnostic of scapholunate dissociation. The scaphoid gap has been called the Terry Thomas sign after the English film comedian’s dental diastema. In both biomechanical and clinical studies, the increase in scapholunate intercarpal distance has been most noticeable in the AP supinated, clenched-fist radiographic view (Fig. 19-2A).
Shortened scaphoid: The scaphoid assumes a flexed posture owing to its dissociation from the surrounding carpus. It appears foreshortened on PA and AP radiographic views.
Cortical ring sign: The flexed posture of the scaphoid results in an end-on view of the scaphoid tubercle/distal scaphoid and, therefore, a more prominently visualized, circular cortex of the scaphoid. A cortical ring to proximal pole distance of less than 7 mm is considered abnormal.
DISI pattern of the carpus: The scaphoid assumes a flexed and dorsally subluxed posture; the lunate assumes an extended and palmarly subluxed posture; and the capitate lies in a flexed posture (Fig. 19-2B).
Taleisnik’s V sign: When the scaphoid is flexed, the palmar edge of the scaphoid outline intersects with the palmar margin of the radius at a more acute angle than that observed in the normal wrist, in which is seen a more gentle, wider C-shaped pattern of intersection.
Scapholunate dissociation is observed alone or in combination with fractures. Carpal alignment is assessed routinely during the evaluation of distal radius fractures, including radial styloid fractures.
Arthrography
Arthrograms of the wrist, although helpful in identifying ligamentous injuries, do not reveal completely the magnitude of such disruption. Dissections of the wrist in cadavers demonstrate a 28% incidence of scapholunate interosseous disruption. In dissections in which both left and right wrists could be evaluated, it was noted that the presence of a scapholunate interosseous ligament disruption on one side was associated with a 66% incidence of disruption of this ligament on the contralateral side (2). These disruptions, however, were not typically associated with a significant instability of the carpal bones.
Although reasonable as part of the workup, a positive arthrogram is not considered pathognomonic for scapholunate dissociation, particularly in the older population. A secondary or relative dorsal intercalated segment instability deformity resulting from a displaced distal radius fracture can occur solely as a result of a distal radius fracture. The DISI pattern of deformity can result, even following a distal radius fracture, from radius malalignment, ligamentous disruption, or a combination of the two.
Arthroscopy
If a patient has a history, physical findings, and a diagnostic workup consistent with acute scapholunate dissociation, a manual examination under anesthesia and an arthroscopic examination (including proximal wrist and midcarpal joint examinations) may be helpful (see Chapter 2). Wrist arthroscopy helps to confirm whether the ligamentous disruption is acute in nature and to identify concomitant chondral or osteochondral lesions.
Arthroscopic examination of the wrist is a critical step in the workup of a patient when normal clinical and radiographic assessment of a patient’s ligament disruption is limited or impaired, as in a wrist with a concomitant distal radius fracture (see Chapter 2). An arthroscopic examination can exclude the presence of a ligament tear as well, as in the case of a wide scapholunate joint space, which can be a normal anatomic finding in a patient with a lunotriquetral coalition (3).
 Figure 19-2 An anteroposterior (AP), supinated, clenched-fist (A) and lateral radiograph view (B
Get Clinical Tree app for offline access
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree


|