Ligamentous Repair for Acute Lunate and Perilunate Dislocations
Robert M. Szabo
Craig C. Newland
Indications and Pathomechanics
Perilunate dislocations are a spectrum of injuries that can result in residual functional and anatomic deficits. Pitfalls exist in recognizing the injury. Early treatment with an understanding of the pathomechanics and relevant anatomy may improve outcomes.
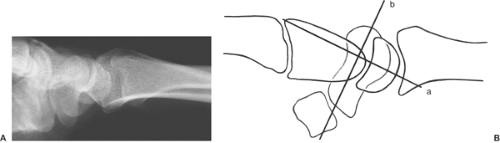
The typical presentation of an acute perilunate dislocation is swelling, pain, and deformity following acute trauma to the wrist. The primary dislocation occurs at the midcarpal joint where the capitate is usually displaced dorsally to the lunate (Figs. 22-1 and 22-2). When the capitate displaces, the scaphoid must either fracture or rotate. If no fracture occurs, the ligaments supporting the proximal pole of the scaphoid rupture, allowing dorsal rotation of the proximal pole, and a dorsal perilunate dislocation results. If the scaphoid fractures, the distal fragment moves with the capitate and distal carpal row and the proximal pole remains attached to the lunate, resulting in a dorsal transscaphoid perilunate dislocation.
It is estimated that 25% of perilunate dislocations are diagnosed late (1). After failure to recognize the radiographic abnormalities typical of this injury, the patient often presents to the emergency department or primary care provider and is treated for a wrist sprain. Failing to recognize the nature and extent of the injury will leave the patient with a chronic scapholunate dissociation. Treatment options for this chronic injury do not offer a good prognosis for maintaining long-term normal anatomic relationships within the carpus (2). Many of these patients develop degenerative arthritis.
The authors believe that all acute perilunate dislocations require surgery. Anatomic reduction of acute perilunate dissociations is difficult to achieve closed and cannot be maintained reliably by external immobilization alone. Adkinson and Chapman (3) noted that only 27% of acute perilunate dislocations managed by closed reduction and external immobilization retained their initial reduction.
An elevated index of suspicion should be aroused when the patient’s history indicates a high-energy mechanism of injury, and swelling with acute tenderness over the dorsal scapholunate interval is present. The differential diagnosis includes consideration of other forms of wrist injury, including fractures of the radius or other carpal bones, particularly the scaphoid, which may not be apparent on initial plain films. Although the pitfalls in diagnosis of a perilunate dislocation have been presented in the emergency medicine literature, missed diagnosis is still common even with a frankly abnormal plain film (4).
Acute rupture of the ligaments in the wrist usually occurs with closed trauma with an applied torque, often as a result of a motor vehicle accident, a fall from a height, or an athletic-related injury. Most commonly seen in adults, the injury also has been described in children (5,6). Almost any imaginable combination of radiocarpal and intercarpal dislocation has been described.
 Figure 22-1 Posteroanterior (PA) radiograph of a patient with an acute scapholunate dissociation. Notice the scapholunate gap of 4 mm (Terry Thomas sign) and the triangular shape of the lunate. |
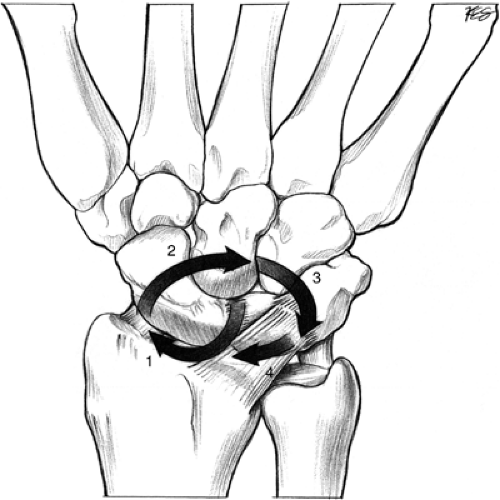
As described by Mayfield and Johnson (7) perilunate dislocations can be produced in the cadaver with forceful wrist dorsiflexion with a progression in severity that begins on the radial side of the carpus with a scapholunate diastasis. Progressive failure leads to dorsal dislocation of the scaphoid and distal row, leaving the lunate behind; then failure of the lunotriquetral ligament, and finally, palmar dislocation of the lunate into the carpal tunnel (7). Producing a series of scapholunate dislocations in cadavers, Mayfield identified a predictable sequence of progressive failure of ligamentous restraints (Fig. 22-3). He postulated a mechanism of injury involving wrist extension, ulnar
deviation, and intercarpal supination in combination producing the various patterns of injury observed. He also noted that hyperextension in pronation or supination neutral tended to produce a scaphoid fracture. The addition of ulnar deviation and intercarpal supination resulted in failure of the scapholunate interosseous ligament (SLIL) and radioscaphocapitate ligament (RSCL), or combined osseous and ligamentous injuries. The pattern of sequential failure begins on the radiopalmar wrist and extends to the ulnar and dorsal wrist (8,9,10).
deviation, and intercarpal supination in combination producing the various patterns of injury observed. He also noted that hyperextension in pronation or supination neutral tended to produce a scaphoid fracture. The addition of ulnar deviation and intercarpal supination resulted in failure of the scapholunate interosseous ligament (SLIL) and radioscaphocapitate ligament (RSCL), or combined osseous and ligamentous injuries. The pattern of sequential failure begins on the radiopalmar wrist and extends to the ulnar and dorsal wrist (8,9,10).
Variations include transradial styloid and transscaphoid perilunate dislocation. Extension of injury on the ulnar aspect can include disruption of the ulnocarpal ligaments and or an ulnar styloid fracture. The ligamentous injuries are referred to as lesser arc injuries and the transosseous injuries are referred to as greater arc injuries.
Volar perilunate fracture dislocations, the rare exception, are proposed to occur with hyperflexion (11). Transtriquetral perilunate dislocation would seem to imply the possibility that the injury may begin on the ulnar side of the carpus, a reverse greater arc pattern (12). Lunate fracture with ulnar-sided ligamentous injury with associated ulnar styloid fracture has also been described (13).
With a higher energy injury (e.g., an open injury) assume more structural damage than might be readily apparent (14). In such a case, in addition to the surgical technique describe below, consider stabilization of the ulnar carpus and or radiocarpal fixation. Failure to recognize and, where appropriate, internally fix the ulnar-sided ligament injury can lead to residual volar intercalated segment instability (VISI) deformity (15).
Not yet established is which intercarpal or radiocarpal ligaments requires direct repair and which heal just by restoring the osseous relationships. One goal of surgery is to reapproximate the osseous anatomy for a sufficient length of time so that the torn ligaments reestablish themselves and heal. Nevertheless, biomechanical structural properties of healed ligaments can lead to altered function, even with successful healing.
Although Mayfield noted structural heterogeneity of the palmar capsular ligaments, Kuhlmann et al. (16) further characterized the variability in the elastic modulus, elongation to failure, and ultimate tensile strength of these same ligaments. The heterogeneous nature of the ligamentous restraints and the multiple combinations of dorsiflexion, ulnar deviation, and intercarpal supination explain the wide spectrum of injuries seen clinically. Mayfield’s proposal of greater and lesser arc injuries with four stages of severity is a useful classification for operative planning. Recognizing that the less-severe injuries are part of a larger spectrum also provides needed emphasis on the importance of early diagnosis. The natural history of a stage I injury is not known, but a stage II injury left untreated will likely evolve by further attrition of weakened ligaments and altered mechanics into a scapholunate advanced collapse (SLAC) wrist pattern of arthritis.
Wrist ligaments vary with regard to the population of neural elements they contain. A particular preponderance of mechanoreceptors has been identified within the scapholunate interosseus ligament, dorsal intercarpal ligament, and dorsal radiocarpal ligament, suggesting a possible proprioceptive function in addition to their role as passive constraints to carpal motion (17). With injury, compromise of some aspect of this proprioceptive function presumably may result. The functional implications of such a deficit are uncertain.
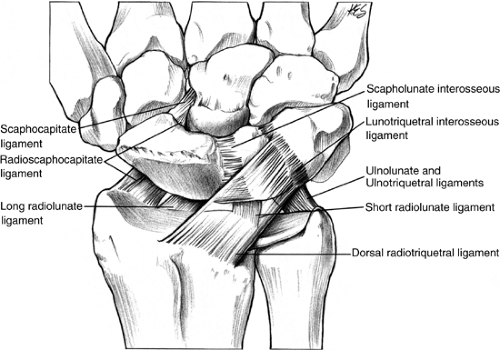
Appreciation of ligamentous anatomy is fundamental to treating instability injuries (Fig. 22-4). The palmar radial carpal ligaments consist of three strong components: the radioscaphocapitate, long radiolunate, and short radiolunate ligaments. The radioscaphocapitate ligament has three parts: radial collateral, radioscaphoid, and radiocapitate. These distinctions are made on the location of insertion, not on discrete anatomic divisions (18). The radioscaphocapitate ligament (RSCL) runs
from the radial styloid through a groove in the waist of the scaphoid ending in the palmar aspect of the capitate. This ligament acts as a fulcrum around which the scaphoid rotates. The RSCL is the only ligamentous connection between the radius and the scaphoid. The long radiolunate ligament (LRL) is parallel to the radioscaphocapitate ligament from the palmar rim of the distal radius to the radial margin of the palmar horn of the lunate. As the central radiocarpal ligament, it augments the scapholunate interosseous ligament palmarly. The LRL ligament and the palmar lunotriquetral interosseous ligament were thought to be in continuity and hence previously called the radiotriquetral ligament. Between the radioscaphocapitate and long radiolunate ligaments is an area of potential weakness over the capitate-lunate articulation known as the space of Poirier. In a stage IV perilunate dislocation, the lunate will dislocate palmarly through this space. The short radiolunate ligament originates from the palmar margin of the distal radius in the area of the lunate facet and inserts into the proximal palmar surface of the lunate. It is contiguous with palmar fibers from the triangular fibrocartilage complex (TFCC). The radioscapholunate ligament (ligament of Testut) once thought to be an important stabilizer of the scaphoid, is found between the long and short radiolunate ligaments. It is a neurovascular pedicle to the scapholunate interosseous ligament derived from the anterior interosseous and radial arteries and the anterior interosseous nerve (19). The ulnolunate and ulnotriquetral ligaments arise from the ulnar triangular meniscus of the wrist and insert on their respective carpal bones.
from the radial styloid through a groove in the waist of the scaphoid ending in the palmar aspect of the capitate. This ligament acts as a fulcrum around which the scaphoid rotates. The RSCL is the only ligamentous connection between the radius and the scaphoid. The long radiolunate ligament (LRL) is parallel to the radioscaphocapitate ligament from the palmar rim of the distal radius to the radial margin of the palmar horn of the lunate. As the central radiocarpal ligament, it augments the scapholunate interosseous ligament palmarly. The LRL ligament and the palmar lunotriquetral interosseous ligament were thought to be in continuity and hence previously called the radiotriquetral ligament. Between the radioscaphocapitate and long radiolunate ligaments is an area of potential weakness over the capitate-lunate articulation known as the space of Poirier. In a stage IV perilunate dislocation, the lunate will dislocate palmarly through this space. The short radiolunate ligament originates from the palmar margin of the distal radius in the area of the lunate facet and inserts into the proximal palmar surface of the lunate. It is contiguous with palmar fibers from the triangular fibrocartilage complex (TFCC). The radioscapholunate ligament (ligament of Testut) once thought to be an important stabilizer of the scaphoid, is found between the long and short radiolunate ligaments. It is a neurovascular pedicle to the scapholunate interosseous ligament derived from the anterior interosseous and radial arteries and the anterior interosseous nerve (19). The ulnolunate and ulnotriquetral ligaments arise from the ulnar triangular meniscus of the wrist and insert on their respective carpal bones.
The dorsal radiocarpal (DRC) ligament originates from the dorsal margin of the distal radius and extends ulnar obliquely and distally. Its radial fibers attach to the lunate and lunotriquetral interosseous ligament and the remainder inserts onto the dorsal tubercle of the triquetrum. The dorsal intercarpal (DIC) ligament originates from the triquetrum, extends radially and inserts onto the lunate, the dorsal groove of the scaphoid and the trapezium (20).
Preoperative Preparation
Initial Management
Overall assessment of the patient within the context of trauma resuscitation and triage may influence the surgical decision-making with regard to a perilunate dislocation. After performing a history and physical examination, closed reduction or temporary splinting may be all that is initially feasible. Every effort should be made to conduct an appropriate neurovascular examination. If the lunate is dislocated at the time of presentation, it is a priority to perform a reduction. The presence of an acute carpal tunnel syndrome when associated with a lunate dislocation heightens the urgency for prompt surgical intervention (21,22). If initial radiographs reveal a palmar dislocation of the lunate, closed reduction is undertaken under intravenous sedation. Place the hand in finger traps and apply 10 pounds of counter-traction. Extend the wrist with one hand, then gently push the lunate back into place with the thumb of the contralateral hand. Bring the wrist into neutral, remove the finger traps, and apply a well-padded plaster reinforced bulky hand dressing for patient comfort, immobilization, and elevation (23). Repeat radiographs to confirm reduction and evaluate the type and degree of injury. Measure the scapholunate interval on the posterioranterior (PA) film and the scapholunate angle on the lateral (Fig. 22-2). Compare with views of the opposite wrist.
Early surgical intervention offers the best prospect for restoring anatomy and avoiding complications. Surgical intervention for the perilunate dislocation can be delayed to the next day, or several days, allowing for the most experienced members of the surgical team to be available. Prompt recognition, accurate reduction, and stable internal fixation contribute to an optimal outcome; however, delayed surgical intervention can also result in a good outcome (24,25).
Imaging
Standard PA and lateral projections of the wrist may be all that is needed in the way of imaging. Current practices vary widely to when more sophisticated imaging is warranted in the assessment of an acute wrist injury. Magnetic resonance imaging (MRI) and or computed tomography (CT) scanning are considered acutely in 10% of institutions surveyed with clinical suspicion of an acute scaphoid fracture and the standard two plain films are normal (26). A principal concern with an acute injury is establishing whether there are partial or complete ligament tears. MRI or CT arthrography has an increased sensitivity for detecting partial ligament and TFCC injuries compared with MRI alone. In the acute setting, an MRI has equivalent sensitivity in identifying a complete tear (27).
On the plain films, the lateral projection should be analyzed for the position of the lunate. With a perilunate dislocation, the lunate may appear palmarly subluxated or dislocated, and may be flipped 180 degrees to its normal orientation. The capitate is likely to be collinear with the radius, although it may lie dorsal. Radiographs corroborate a gross disturbance of carpal relationships (Figs. 22-1 and 22-2).
The PA projection should be analyzed for a disruption of Gilula’s lines, although with caution as these arcs may be normally disrupted in ulnar and radial deviation (28,29). A radiograph in gravity traction or with a small weight may facilitate evaluation just as it may effectively unmask a scapholunate dissociation when plain films are normal (30).
With a congenital lunotriquetral coalition, exercise caution in interpreting what seems to be a wide scapholunate interval because this may likely be a normal variation (31).
In a dorsal perilunate dislocation, the lateral radiograph shows the longitudinal axis of the capitate dorsal to the longitudinal axis of the radius and the proximal pole of the scaphoid rotated dorsally. Look for a dorsal intercalated segmental instability (DISI) pattern reflecting abnormal resting relationships between the lunate and the scaphoid. DISI is defined by an increased scapholunate angle on the lateral projection, which results as the scaphoid assumes a flexed posture in response to joint contact forces that are no longer resisted by the disrupted ligamentous constraints of the radioscaphocapitate ligament and volar scaphotrapeziotrapezoid ligaments, and the scapholunate interosseous ligament. The resting posture of the lunate is influenced by the intact lunatotriquetral ligaments, which tend to draw the lunate into dorsiflexion following the helicoid surface of the triquetral-hamate joint. A scapholunate angle greater than 70 degrees on a neutral lateral is taken as abnormal (normal = 47 degrees; >60 degrees is of concern). This measure relies on a neutral axis with regard to radial and ulnar deviation when taking the film. In a lunate dislocation, the longitudinal axis of the capitate tends to be nearly or actually colinear with that of the radius, and the lunate is displaced palmarward (“spilled tea cup” sign) (32). On the PA film, the lunate may appear triangular and the scaphoid foreshortened. A scapholunate interval of greater than 2 mm is considered abnormal (Terry Thomas sign).
Transscaphoid and transcapitate fractures, as well as radial styloid and ulnar styloid fractures, are recognized variants of this injury pattern. The transscaphoid perilunate dislocation is the most common pattern (1). When a transscaphoid transtriquetral injury is present allowing screw fixation of both the scaphoid and the triquetrum, the prospects for early motion are improved (33). Fracture of the proximal pole of the capitate can be surprisingly subtle. This injury can be obscure, even though the proximal pole fragment is flipped 180 degrees with the articular surface facing distally (34). Oblique films or tomograms are necessary if the head of the capitate cannot be clearly visualized (35). Palmar and radial displacement of the proximal pole of the scaphoid from the scaphoid fossa is diagnostic of a scaphoid dislocation rather than perilunate dislocation. The lack of an intact ligamentous hinge distally or interposition of soft tissue (torn ligaments) may prevent successful restoration of anatomy with closed reduction (36).
When a scaphoid fracture and a scapholunate interosseous ligament injury are both present, the prognosis is poor. Primary scaphoid excision and four-corner fusion might be considered as offering the most expeditious return to function (37).
Dissociative ligamentous lesions are common with distal radius fracture with an estimated incidence of 40%. The high prevalence has been documented by arthroscopic studies. The prognosis has generally been taken as relatively benign; however, radiographic studies have shown an increasing tendency toward loss of carpal height, implying that the long-term prognosis may not be as good (38).
Surgical Technique
Place the patient supine on the operating room table with a tourniquet placed around the upper arm. Either general anesthesia or axillary block is administered. Although reduction and percutaneous pin fixation under direct arthroscopic visualization is advocated by some (39
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree