Lesser Ray Deformities
PART 1 Deformities of the Intermediate Digits and the Metatarsophalangeal Joint
Dalton E. McGlamry
Louis A. Jimenez
Donald R. Green
Lesser ray deformities should be classified as a group of related conditions. In 1927, Schuster defined hammer toe as “… a deformity in which the proximal phalanx of one of the smaller toes is bent upward or is dorsiflexed at the metatarsophalangeal joint, and the median and distal phalanges are sharply bent downward, so that they form a more or less acute angle with the proximal phalanx” (1). Sometimes the distal phalanx is extended so it and the second phalanx form another angle. That definition provided some early insight into the deformities that involve the lesser rays. In fact, deformities of the lesser rays are complex and involve the interphalangeal joints, metatarsophalangeal joints, and the related tendon and ligamentous structures. Metatarsal and digital disorders are considered related conditions.
ETIOLOGY OF LESSER RAY DEFORMITIES
The causes of lesser ray deformities may be congenital or acquired. Genetic influences are responsible for many of the deformities of the lesser toes and metatarsophalangeal joints. Often, the genetic influence of a given structural foot type may not be recognized for many years until the deformity becomes manifest. Neuromuscular disorders are a major cause of multiple claw toes. Unquestionably, general biomechanical dysfunction has more to do with digital function than any other single factor.
BIOMECHANICS OF LESSER DIGITAL FUNCTION
To analyze digital function, the functional anatomy of the lesser toes must be discussed. This includes the role of the extrinsic muscles (muscles that originate outside the foot but insert into the foot), the intrinsic muscles (muscles that originate and insert within the foot), and the various joints and bony relationships within the foot and ankle. Muscles that cross more than one joint have multiple functions and affect activity across each level. The muscle direction, force, and relation to joint axis and range of joint motion are all modifying factors influencing the muscle activity.
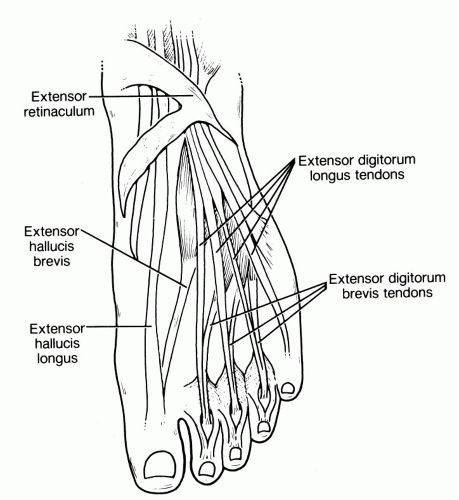
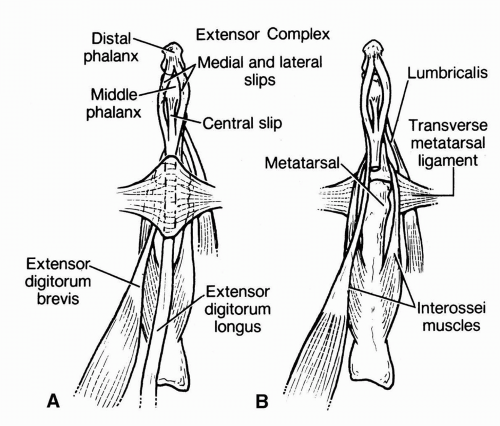
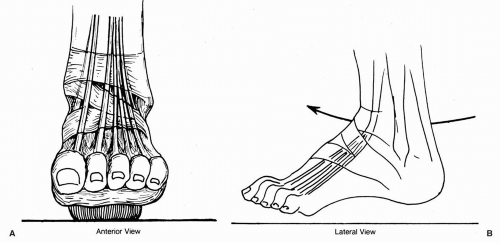
Muscles of primary concern in lesser digital function are the extensor digitorum longus, the extensor digitorum brevis, the flexor digitorum longus, the flexor digitorum brevis, the interossei (and the flexor digiti quinti brevis), the lumbricales, and the quadratus plantae. The extensor digitorum longus aids dorsiflexion of the lesser toes during the swing phase of gait and at heel contact (2). The extensor digitorum longus and brevis function in the propulsive phase of gait to stabilize the proximal phalanx against the metatarsal heads to prepare for foot lift and to dorsiflex the metatarsophalangeal joints (3). The extensor digitorum longus is an extrinsic muscle that originates from the anterior compartment of the leg. The tendon passes underneath the extensor retinaculum at the ankle, where it divides into four separate tendon slips (one going to each of the lesser toes) (Fig. 1).
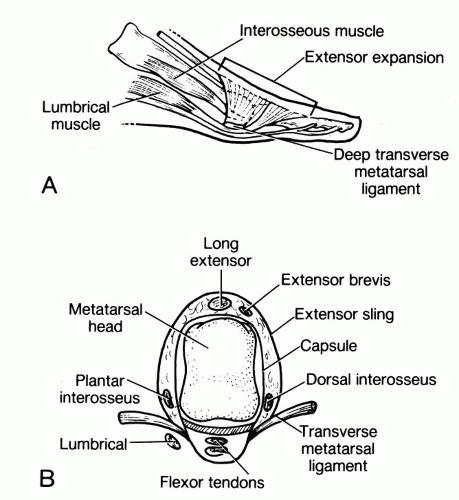
At the level of the metatarsophalangeal joint, each tendon provides multiple medial and lateral fibrous extensions that unite plantarly to encircle the proximal phalanx (Fig. 2). The more proximal fibrous extensions are oriented vertically to the extensor tendon and encircle the metatarsophalangeal joint. Plantarly, the fibers unite with the capsule, the deep transverse metatarsal ligament, and the flexor tendon sheath.
The more distal fibrous extensions have oblique fiber directions and extend from near the metatarsophalangeal joint to the head of the proximal phalanx (4,5).
The more distal fibrous extensions have oblique fiber directions and extend from near the metatarsophalangeal joint to the head of the proximal phalanx (4,5).
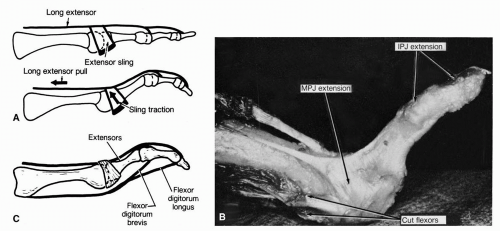
The extensor digitorum brevis muscle belly originates from the dorsolateral aspect of the calcaneus. Three individual tendon slips arise and course to the corresponding second, third, and fourth toes. (There is no extensor digitorum brevis to the fifth toe.) The extensor digitorum brevis tendons approach the lesser metatarsophalangeal joints from the lateral side and combine with the extensor digitorum longus tendon slip to form the extensor expansion to the lesser toes. The extensor tendon complex divides into three slips, with the center slip inserting dorsally into the middle phalanx. The medial and lateral wings rejoin to insert into the dorsum of the distal phalanx. Occasionally, the extensor digitorum brevis tendon serves as a separate lateral wing of this extensor expansion (Fig. 3). Medial and lateral fibrous extensions of the extensor tendon are also known as the hood apparatus. This hood apparatus is part of the sling mechanism, which, by wrapping around the base of the proximal phalanx, can lift the proximal phalanx like a sling. The extensor apparatus has no specific attachments into the proximal phalanx.
The pull of the long or short extensor tendons creates a significant dorsiflexion of the proximal phalanx at the metatarsophalangeal joint by the sling mechanism. Most of the force is directed into the sling; not much force is conveyed onto the proximal interphalangeal joint or the distal interphalangeal joint (4,5) (Fig. 4). The flexor digitorum brevis and longus are placed on stretch when the metatarsophalangeal joint is dorsiflexed. This exerts a passive pull on the proximal and the distal interphalangeal joints. This plantarflexion force at these joints can provide the final influence to complete a hammer toe deformity. Thus, the force of the extensors exerts a relatively small passive plantarflexory force on the proximal or distal interphalangeal joints.
The extensor digitorum longus functions not only on the digits, but also across the ankle joint, thus creating ankle joint dorsiflexion, and across the subtalar and midtarsal joints, thus creating pronation. The extensor digitorum longus is one of the primary dorsiflexors of the foot at the ankle, along with the extensor hallucis longus and the tibialis anterior.
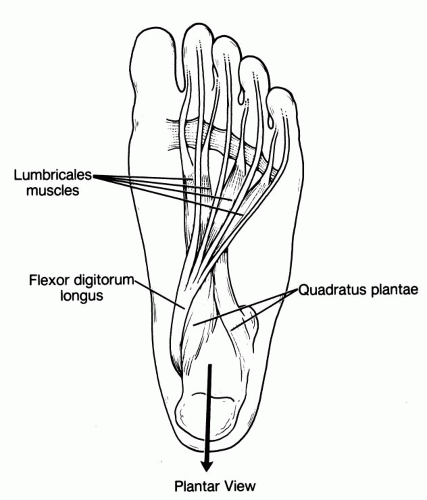
The flexor digitorum longus and brevis muscles function together in aiding plantarflexion of the lesser digits during the stance phase of gait (3). They primarily create a plantarflexory force on the interphalangeal joints. The flexor digitorum longus is an extrinsic muscle that originates from the deep posterior compartment of the leg. The tendon passes underneath the flexor retinaculum on the medial side of the foot. It divides into four separate tendon slips within the second layer of musculature of the plantar aspect of the foot. Each of these tendons runs to a lesser digit. The quadratus plantae muscle originates from the plantar calcaneus and inserts into the conjoined tendon of the flexor digitorum longus. Four small lumbricales muscles originate from the medial aspect of each flexor digitorum longus tendon slip and insert into the corresponding digits (Fig. 5).
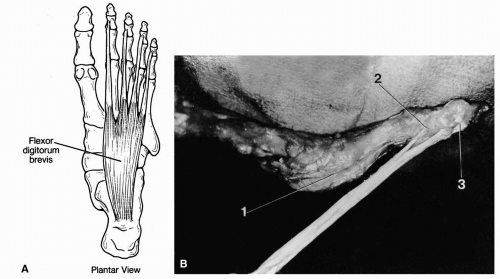
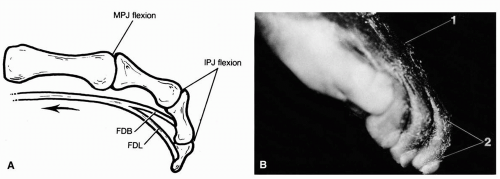
The flexor digitorum brevis muscle originates from the plantar aspect of the calcaneus in the first layer (most superficial layer) of the plantar muscles. Four individual muscle tendon slips arise and course to each of the corresponding lesser digits. The long and short flexor tendons pass plantar to the metatarsophalangeal joint in a groove created by the thickened plantar capsule. At the level of the proximal phalanx, the flexor digitorum brevis tendon splits into two segments to allow the flexor digitorum longus tendon to penetrate the tendon, to become more superficial and to insert into the distal phalanx. The two segments of the flexor digitorum brevis tendon insert together more proximally into the base of the middle phalanx (3,4) (Fig. 6).
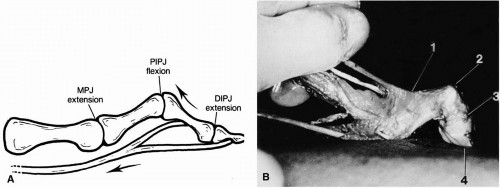
The pull of the flexor digitorum longus and brevis muscles creates significant plantarflexory force at the interphalangeal joints (Fig. 7). However, the flexors primarily function during the stance phase of gait with the toes on the ground (2). In a weight-bearing situation, a strong plantarflexory force remains at the interphalangeal joint, but because the phalanges cannot be plantarflexed through the ground, the retrograde force may cause dorsiflexion at the metatarsophalangeal joint (Fig. 8). When the flexor digitorum brevis is the primary plantarflexory force, plantarflexion occurs strongly at the proximal interphalangeal joint, and the strong plantarflexory force at the distal interphalangeal joint is absent. This may yield a contracted toe with the distal interphalangeal joint hyperextended. When the flexor digitorum longus is active, force is generated primarily at the distal interphalangeal joint. A strong secondary force occurs at the proximal interphalangeal joint. This leads to a contracted toe with the distal interphalangeal joint plantarflexed (4).
The flexor digitorum longus is an extrinsic muscle, and it functions not only on the digits but also across the ankle joint, the subtalar joint, and the midtarsal joint. The flexor digitorum longus has a vector of force that can aid in plantarflexion of the ankle, deceleration of the forward motion of the leg, supination of the subtalar and midtarsal joints, and external rotation of the leg (3).
The dorsal and plantar interossei and the flexor digiti quinti brevis are discussed together. These eight intrinsic muscles seem to function as four sets of muscles (one pair of muscles for each lesser digit). The dorsal interossei are bipennate muscles that originate from the adjacent sides of the corresponding metatarsals. The first dorsal interosseous muscle originates from the first and second metatarsal shafts and inserts medially into the second toe. The dorsal interossei in the second, third, and fourth intermetatarsal spaces originate from the adjacent sides of the corresponding lesser metatarsals and insert laterally into digits 2, 3, and 4 (6) (Fig. 9A).
The plantar interossei are unipennate muscles that originate from the plantar medial aspect of the metatarsal shaft of the digit into which they insert. The plantar interossei insert medially into the third, fourth, and fifth digits. The flexor digiti quinti brevis is a unipennate muscle that originates from the lateral plantar aspect of the fifth metatarsal shaft and inserts laterally into the fifth digit (Fig. 9B).
Thus, eight small muscles originate from the metatarsal shafts. One muscle inserts medially and one laterally into each lesser toe (Fig. 9C). These tendons insert into the plantarmost medial or lateral aspect of the base of the proximal phalanx (Fig. 10A). The tendons also insert into the plantar pad or plate (a glenoid cartilaginous cap inferior to the metatarsal head). The transverse intermetatarsal ligament, the capsular tissues, the strands of the plantar fascia, and the extensor hood apparatus also insert here (Fig. 10B). Sarrafian and Topouzian indicated that some attachments of these tendons into the extensor sling mechanism are usually present (5), although Jarrett and associates did not find any significant attachments of this nature (4).
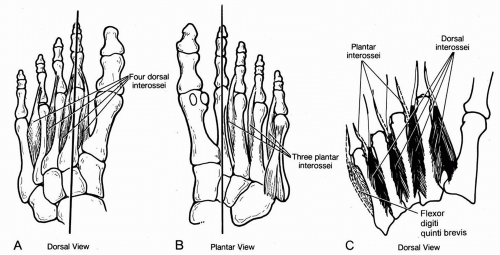 FIG. 9. A: Dorsal view of the four dorsal interossei. B: Plantar view of the three plantar interossei. C: Dorsal view of the four sets of muscles (including the flexor digiti quinti brevis). |
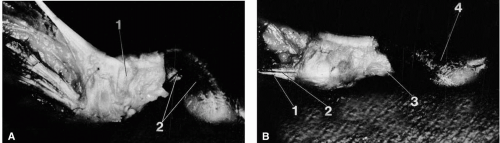
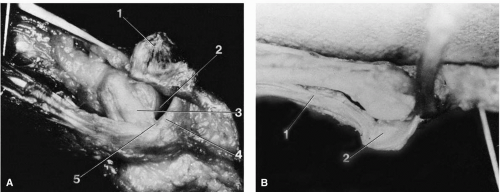 FIG. 10. A: The interossei insert into the plantarmost base of proximal phalanx and into the plantar “plate.” The fibers are superficial to the capsule of the metatarsophalangeal joint and deep to the vertical fibers of the extensor apparatus. 1, Extensor expansion (reflected); 2, metatarsal head; 3, collateral ligament; 4, base of proximal phalanx; 5, insertion interossei. B: Interossei tendons (1) merge with the plantar capsule and glenoid plate (2) of the lesser metatarsophalangeal joints. |
In discussing the forces and the functions of these four sets of muscles, we call the muscles collectively interossei. The interossei function as stabilizing muscles in the transverse plane. When force is applied to the medial interossei, the toes adduct and slightly plantarflex. When force is applied to the lateral interossei, the toes abduct and plantarflex. When force is applied to each set of interossei on both sides of the respective digits, the toe is stabilized in the transverse plane and is plantarflexed at the metatarsophalangeal joint (Fig. 11).
Because the interossei function during the stance phase of gait, the proximal phalanx cannot be plantarflexed through the ground (2). However, a simultaneous pull of the interosseous muscles does neutralize or limit the dorsiflexory forces that occur at the metatarsophalangeal joint during gait. Normal, unopposed forces generated by the flexor digitorum longus and brevis muscles produce the contracted lesser toe in a weight-bearing situation. However, this stance-phase metatarsophalangeal joint dorsiflexion does not occur in a normal foot. Mild, passive buckling at the metatarsophalangeal joint created by the flexor digitorum longus and brevis muscles is easily neutralized by the interosseous muscles if these muscles gain mechanical advantage. When the interossei function before contraction of the short flexors, a rigid beam effect is created within the toe. The long flexors cross many joints, and the interossei function after they begin their stance-phase activity but well before completion of that activity (2). This normally eliminates the stance-phase contraction of the lesser toes (Fig. 12).
The lumbricales are four small muscles that have an unusual tendon origin. Most muscles originate from bone. Each of the lumbricales originates from the medial side of the corresponding flexor digitorum longus slip to the lesser toe. They course beneath (plantar to) the deep transverse metatarsal ligament and insert medially into the base of the proximal phalanx and the oblique portion of the extensor hood apparatus. These muscles have not as yet been recorded electromyographically in gait (2, 3, 4). Therefore, their action in gait is theoretic at present.
Although the muscles are extremely small, they have a good mechanical advantage to create plantarflexion of the proximal phalanx with a mild adduction component. The lumbricales dorsiflex the proximal and distal interphalangeal joints through the extensor sling apparatus (4). An additional unique force is generated by the contraction of the lumbricales on their movable origin, the tendon of the flexor digitorum longus.
When a muscle contracts, the forces occur in both directions to cause contraction. However, if muscles originate from immobile bone, the cumulative pull is all directed toward the tendon. Because the lumbricales arise from tendon, the resultant forces are placed on the flexor digitorum longus tendon, on the insertions into the proximal phalanx, and on the extensor sling (Fig. 13). Thus, the flexor digitorum longus muscle-tendon complex is put on stretch proximally and is relaxed distally. This creates slack in the flexor digitorum longus tendon distally. Pull on the extensors alone creates more than 90 degrees of lesser metatarsophalangeal joint dorsiflexion.
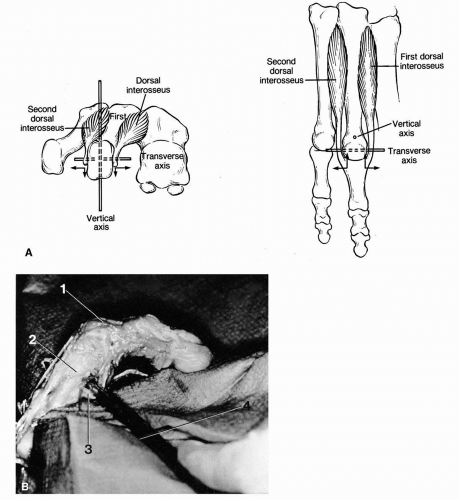 FIG. 11. A: The interossei can create force around the vertical axis or horizontal axis of the metatarsophalangeal joint. When both interossei are active, motion around vertical axis is neutralized (stabilization without transverse plane motion). However, a plantarflexory force is created. B: Metatarsophalangeal plantarflexion (1) results when the force is applied to both interossei simultaneously. 2, Metatarsal; 3, simultaneous pull of both interossei by a hemostat. |
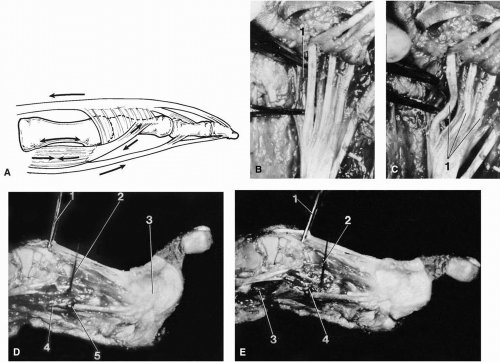 FIG. 13. A: Diagram depicting the normal physiologic contraction of the lumbricales muscle that results in a proximally directed pull on the lumbricales tendon. This causes plantarflexion at the metatarsophalangeal joint and dorsiflexion of the interphalangeal joints by a sling mechanism. Distally directed pull is also placed on the long flexor tendon (FDL), thus reducing flexor’s passive deforming force that occurs with long extensor (EDL) contraction. B: Two hemostats are used to simulate contraction of the small first lumbricales muscle (1). C: As the hemostats are pulled together (simulating contraction), slack is created on the corresponding FDL tendon distally (1). D: Unchecked pull of the EDL results in excessive dorsiflexion at the metatarsophalangeal joint. Note the pin (2) in the metatarsal and the suture marker (5) in the lumbricales muscle (4). 1, Pull on FDL; 2, pin marker in the metatarsal; 3, extensor expansion (sling). E: Significant limitation of metatarsophalangeal joint dorsiflexion is created when the lumbricales muscle is activated before creating the same force on the extensors as demonstrated in D. Note that suture marker (4) on lumbricales muscle (3) is proximal to needle marker. 1, Pull on the EDL; 2, pin marker in the metatarsal. |
When the flexors are intact, a passive plantarflexion at the proximal and distal interphalangeal joints occurs. This is not normally seen in gait. Pulling by the lumbricales before the initiation of force on the extensors allows only the normal 20 to 40 degrees of dorsiflexion at the metatarsophalangeal joints. The lumbricales neutralize the passive plantarflexory force of the flexors. Furthermore, if the lumbricales do stabilize the metatarsophalangeal joint in the swing phase of gait, the extensor digitorum longus can function as a primary dorsiflexor of the foot at the ankle. The lumbricales create an early end range of motion of the lesser metatarsophalangeal joints and allow direction of the extensor digitorum longus forces toward the ankle joint at an early and effective time during the gait cycle. The lumbricales appear well positioned to function in unison with the extensors. This theory of the
function of the lumbricales adds logic to the function of the extensor digitorum longus as a primary dorsiflexory force at the ankle joint.
function of the lumbricales adds logic to the function of the extensor digitorum longus as a primary dorsiflexory force at the ankle joint.
Because the hand is a non-weight-bearing structure, direct analogies between it and the foot are not always acceptable. The anatomic similarities of the lumbricales and the interossei of the hand and foot argue well for the validity of some correlation. That the hand lumbricales function in unison with the hand extensors lends further support to this theory (7).
In summary, the lumbricales create plantarflexion of the metatarsophalangeal joint, dorsiflexion of the proximal and distal interphalangeal joints, distal slack in the flexor digitorum longus tendon, and a slight adductory force. This action limits the excessive swing-phase contraction of the toes that would otherwise be created by the extensor tendons. Excessive dorsiflexion of the metatarsophalangeal joints would be limited. The mild abduction created by the extensor digitorum brevis muscle would also be neutralized by the mild adduction force of the lumbricales. Plantarflexion of the distal interphalangeal and proximal interphalangeal joints by the passive pull of the flexors would be resisted by the dorsiflexory force created at the proximal and distal interphalangeal joints. This is accomplished by the sling mechanism and by the slack created in the tendons of the flexor digitorum longus. Thus, the theory of Jarrett and associates (4), that the lumbricales function in unison with the extensors during the swing phase of gait to prevent the excessive dorsiflexion of the metatarsophalangeal joint in the normal foot, is logical and probably correct. This theory must await further electromyographic analysis of gait, including the lumbricales, to obtain confirmation.
The quadratus plantae muscle originates from the inferior surface of the calcaneus with two muscle bellies. The smaller medial muscle belly originates from the medial surface of the calcaneus, and the larger belly originates from the lateral inferior surface of the calcaneus. The quadratus plantae forms a wide tendinous lateral proximal insertion into the flexor digitorum longus tendon at the level of division into its four slips (6). The quadratus plantae muscle provides proximal stability to both the lumbricales and the flexor digitorum longus (3).
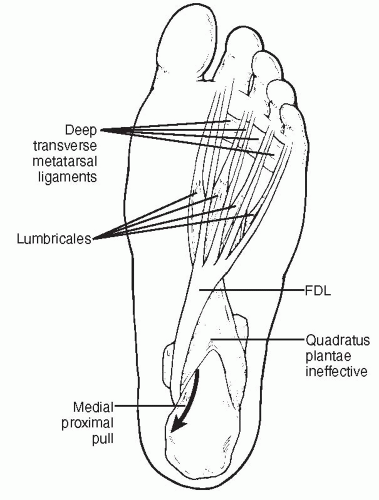
The quadratus plantae also functions to straighten the medial proximal pull of the flexor digitorum longus. The quadratus plantae muscle pulls laterally and proximally and, coupled with the medial proximal forces of the flexor digitorum longus, creates a resultant vector of force that is more or less a straight proximal pull (3). When the quadratus plantae loses its mechanical advantage, the resultant medial proximal pull by the flexor digitorum longus creates an adductovarus pull to the fifth toe and, to a lesser extent, to the fourth and third toes. The direction of force of the flexor digitorum longus to the second toe is primarily a proximal force with little to no medial pull. Consequently, the pull on the second toe is primarily a straight digital contraction force in the sagittal plane (3) (Fig. 14).
The static structures surrounding the lesser metatarsophalangeal joints have not been discussed in detail. These structures are important in limiting severe momentary disruptive forces that could otherwise lead to dislocation of the joints. However, these structures slowly adapt in a contracted or lengthened state according to Wolff’s law in response to chronic deforming forces. These structures include the collateral ligaments, the capsular structures, the transverse metatarsal ligaments, and the plantar fascia. The transverse pedis (the transverse head of the adductor hallucis) arises in part from the deep transverse ligament as well as from the plantar metatarsal ligaments of the third, fourth, and fifth toes. This may give a dynamic component to these soft tissue structures. The flexor digitorum brevis muscle, the adductor hallucis muscle, and the abductor digiti quinti muscle all arise in part from the plantar fascia. This may also confer a dynamic component to the plantar fascia (6,8).
PATHOMECHANICS
Hammer toe syndrome occurs when the normal delicate balance of power surrounding the lesser metatarsophalangeal
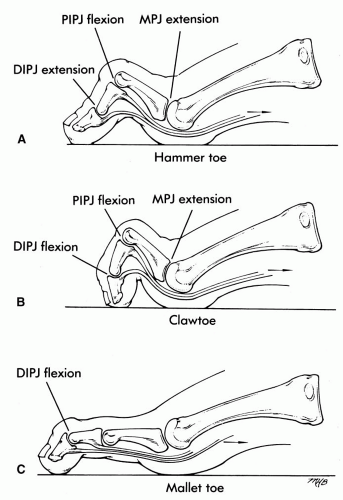
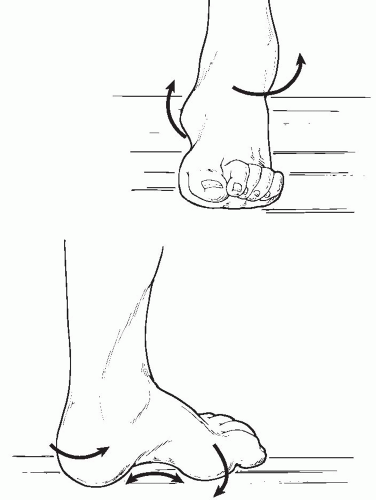
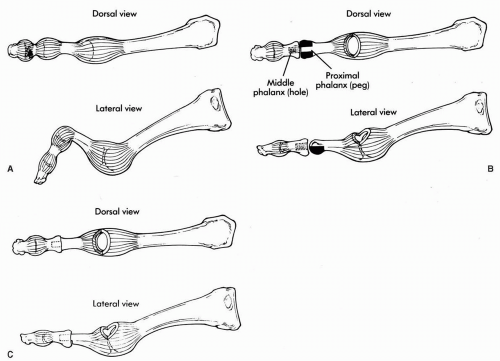
joints is lost. The hammer toe can manifest itself in several different ways, including the classic hammer toe, claw toe, or mallet toe (Fig. 15). The cause of this abnormal digital function is variable, but it falls into three major categories: flexor stabilization, flexor substitution, and extensor substitution.
joints is lost. The hammer toe can manifest itself in several different ways, including the classic hammer toe, claw toe, or mallet toe (Fig. 15). The cause of this abnormal digital function is variable, but it falls into three major categories: flexor stabilization, flexor substitution, and extensor substitution.
Flexor Stabilization
Flexor stabilization occurs in a pronated foot in the late-stance phase of gait when the flexor digitorum longus or brevis muscles have gained mechanical advantage over the interossei. There is often an associated adductovarus of the fifth toe and possibly the fourth toe because the quadratus plantae muscle usually loses its mechanical advantage as well, so the long flexor tendons pull on those toes at an angle. The flexors can gain mechanical advantage over the interossei in several ways. The first is most commonly associated with the flexible pes planovalgus deformity with excessive subtalar joint pronation. Pronation of the subtalar joint allows hypermobility and unlocking of the midtarsal joint and leads to hypermobility of the forefoot. The flexors fire earlier and stay contracted longer than normal in gait, in an attempt to stabilize the osseous structures of the forefoot (9). These muscles are usually ineffective in stabilizing the forefoot. However, the flexors usually are effective in overpowering the small interosseous muscles, and they cause digital hammering or clawing (Fig. 16).
Gray demonstrated that the deep posterior muscle groups, including the flexor hallucis longus, fire earlier and longer in the pes valgus foot (10). However, the action of the flexor digitorum longus muscle was not recorded, and the assumption has been made that this muscle also fires earlier (10,11). With subtalar joint pronation and unlocking of the midtarsal joint, relative forefoot abduction on the rearfoot usually occurs. This usually occurs by medial deviation and collapse of the midfoot because the heel and the ball of the foot remain on the ground. This changes the normal lateral vector of force created by the quadratus plantae. A more medial pull by the flexor digitorum longus results and creates the adductovarus rotation of the fifth toe, possibly the fourth toe, and occasionally the third toe (3).
Weak interosseous muscles can also lead to an increased mechanical advantage for the flexors. Peripheral neuropathy can lead to loss of muscle power of the small intrinsic muscles that allows the normal flexor activity to create stance-phase contraction of the toes. Spasticity of the flexor digitorum longus can also lead to overpowering of the interossei and to flexor stabilization contracture of the toes (4). The subtalar joint usually appears pronated in this situation, but
it may appear normal in the early stages. Flexor stabilization is the most common cause of hammer toes.
it may appear normal in the early stages. Flexor stabilization is the most common cause of hammer toes.
Flexor Substitution
Flexor substitution occurs in a supinated foot in the late-stance phase of gait when the flexors have gained mechanical advantage over the interossei muscles. There is usually a straight contraction of all lesser toes (no adductovarus of the fourth and fifth toes). This situation develops when the triceps surae muscle is weak and the deep posterior and lateral leg muscles try to substitute for the weak triceps (3). A calcaneus gait results. The flexor hallucis longus, the flexor digitorum longus, the tibialis posterior, the peroneus longus, and the peroneus brevis muscles all pass posterior to the ankle joint axis and have a potential for plantarflexion of the ankle. However, the plantarflexion lever arm for these muscles is short, and the plantarflexory force is not extremely effective. In a weight-bearing situation, all these muscles except the peroneus brevis can supinate the subtalar joint.
The tibialis posterior is the primary decelerator of pronation and supinator of the rearfoot (3). The flexor hallucis longus and the flexor digitorum longus also have axes of supination around the subtalar joint. In the presence of a weak triceps surae, these muscles fire earlier and longer than usual and cause severe contraction of the digits and some subtalar joint supination. The pull of the peroneus longus muscle leads to plantarflexion of the first ray, which creates subtalar joint supination in a weight-bearing state. The pronatory force of the peroneus brevis is not adequate to resist these other strong supinatory forces. Thus, a high-arched, late-stance supinated foot occurs with contraction of all the toes (Fig. 17). The early and sustained firing of the flexor group easily gains mechanical advantage over the interossei. The attempt to substitute for the weak triceps surae is usually inadequate to create heel lift. However, this action does lead to hammer digit syndrome. Flexor substitution is the least common of the three major categories that create the pathologic hammer digit syndrome of the lesser digits.
Extensor Substitution
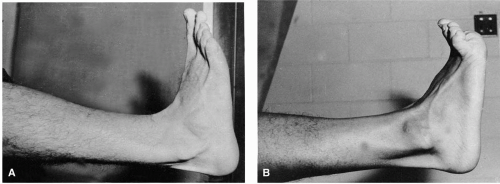
Extensor substitution is seen with a swing-phase excessive digital contraction in which the extensor digitorum longus has gained mechanical advantage over the lumbricales. The severe dorsal hyperextension at the lesser metatarsophalangeal joints is usually a straight dorsal contraction greater than the normal 20 to 40 degrees (12,13). An adductovarus type of contracted toe is usually not seen with extensor substitution. This severe dorsal contraction occurs during propulsion, swing phase, and heel contact when the extensor digitorum longus and brevis muscles are normally active (2,3). Occasionally, the first metatarsophalangeal joint may also be excessively contracted. Bowstringing of the extensor digitorum longus tendons and plantar prominence of the metatarsal heads usually accompany this excessive dorsiflexion contracture of the metatarsophalangeal joints (Fig. 18).
This deformity often begins as a flexible deformity that may reduce completely during weight bearing. The structural changes become more rigid as accommodative contractures develop. The hammered digits can be demonstrated in a non-weight-bearing situation by having the patient dorsiflex the ankles (Fig. 19). Excessive dorsiflexion of the metatarsophalangeal joints can reach as much as 90 to 130 degrees.
The extensor digitorum longus is an extrinsic muscle and also functions to dorsiflex the foot at the ankle. The extensor digitorum longus must move the joints of least resistance (the metatarsophalangeal joints) to their end range of motion before functioning significantly on the ankle. Without the stabilizing effect of the lumbricales, the metatarsophalangeal joints are excessively dorsiflexed as the extensors fire. The extensors can gain this mechanical advantage in many different circumstances. A pes cavus (especially a flexible type),
an ankle equinus, weakness of the lumbricales, spasticity of the extensor digitorum longus muscle, and reaction to metatarsalgia can all lead to this mechanical advantage.
an ankle equinus, weakness of the lumbricales, spasticity of the extensor digitorum longus muscle, and reaction to metatarsalgia can all lead to this mechanical advantage.
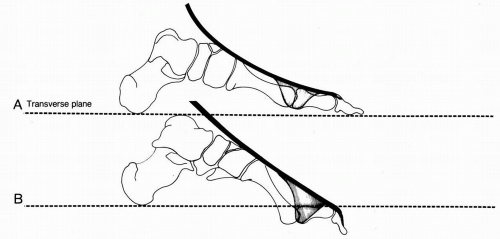
Patients with the pes cavus foot type have an increased declination of the forefoot. With the increased declination, the extensor digitorum longus tendons have a longer distance to course. The tendons do not lengthen; rather, a passive pull is created as the forefoot drops into excessive plantarflexion. This is especially true in the flexible pes cavus (Fig. 20). This leads to dorsiflexion at the metatarsophalangeal joints. Consequently, in a non-weight-bearing situation, the extensor digitorum longus muscle is already on stretch and begins with a mechanical advantage. An additional passive pull of the flexors occurs at the interphalangeal joints. In a weight-bearing position, the flexible component to the anterior pes cavus may be eliminated, and the toes may straighten (Fig. 21).
When the toes become excessively dorsiflexed, the increased retrograde force on the metatarsal heads tends to increase the cavus deformity, thus leading to more dorsiflexion at the metatarsophalangeal joint and creating a further vicious cycle (Fig. 22). The more rigid the hammer digit syndrome becomes, the greater the amount of toe deformity will remain during weight-bearing (14).
When the toes become excessively dorsiflexed, the increased retrograde force on the metatarsal heads tends to increase the cavus deformity, thus leading to more dorsiflexion at the metatarsophalangeal joint and creating a further vicious cycle (Fig. 22). The more rigid the hammer digit syndrome becomes, the greater the amount of toe deformity will remain during weight-bearing (14).
The extensor substitution phenomenon may also result from significant limited ankle joint dorsiflexion. The anterior muscle group (tibialis anterior, extensor hallucis longus, and extensor digitorum longus) fires earlier and longer in an attempt to increase ankle joint dorsiflexion to gain ground clearance during the swing phase of gait. This ineffective attempt to increase ankle dorsiflexion leads to recruitment of the extensor digitorum longus, which then gains mechanical advantage over the lumbricales.
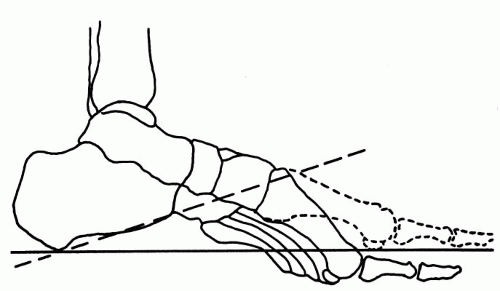 FIG. 21. In a flexible pes cavus, the cavus component is reduced by the reactive force of gravity in a weight-bearing situation. Contracted toes usually also reduce if they are flexible. |
Weakness of the lumbricales or spasticity of the extensor digitorum longus can also create the extensor substitution phenomenon. In patients with neuromuscular disease with peripheral neuropathies, the intrinsic muscles are often affected first. With loss of function of the lumbricales, the extensor digitorum longus gains the mechanical advantage and leads to the extensor substitution phenomenon. Spasticity of the extensor digitorum longus can also lead to overpowering of the small intrinsic lumbricales.
Anything that causes the extensor digitorum longus to gain mechanical advantage over the lumbricales creates extensor substitution. The patient may voluntarily lift the feet off the ground, rather than having a normal propulsive gait pattern, or may resist putting the forefoot on the ground during normal forefoot loading. This action can be caused by pain in the foot, instability in gait pattern, or an active attempt to walk differently. The anterior muscle group must actively function earlier than normal to accomplish this movement. Such action results in its gaining a mechanical advantage over the lumbricales muscles. If the cause of this voluntary foot lift is eliminated by reducing pain or increasing stability, the extensor substitution will often be eliminated.
Transverse plane deformities of the lesser digits also occur. An adducted or abducted digit is usually a result of a loss of balance of power between the set of interosseous muscles to a given digit. It may also result from mechanical pressure on the toes by an adjacent toe. Tumor or joint effusion or joint inflammation may also lead to the transverse plane instability. Structural transverse plane foot deformities such as metatarsus adductus can lead to abnormal transverse positioning of the toes (Fig. 23).
DIGITAL DEFORMITIES
Digital deformities can occur in the sagittal, transverse, or frontal planes.
Mallet Toe
Mallet toe is a sagittal plane deformity in which the distal phalanx is flexed on the middle. It does not normally involve the proximal interphalangeal or the metatarsophalangeal joint. Mallet toe is often associated with a long digit and presents clinically as a flexion contracture of the distal interphalangeal joint.
Clinical evaluation may reveal hyperkeratosis on the distal aspect of the digit in addition to a dorsal heloma, with limited extension of that joint. Early in its development, mallet toe is easily reduced, but later, as adaptation occurs, manual reduction becomes difficult. The condition may be associated with hammer toe and claw toe deformities. Other possible causes of mallet toe are poor visual acuity, in which the patient may need to use the end of the digit for tactile sensation as an aid to balance with decreasing reliance on sight, and a long toe accommodating to short shoes. This may also occur after arthrodesing procedures of the proximal interphalangeal joints and on occasion after a cerebrovascular accident, as a result of residual spasticity of the long flexors.
Radiographic findings include obvious contracture of the distal interphalangeal joint, superimposition of the middle phalanx on the distal phalanx, and an evident gun barrel sign of the distal phalanx.
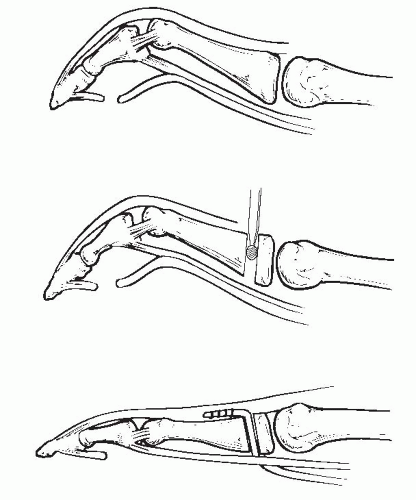
Goals of surgical treatment usually include releasing the long flexor tendon or shortening the toe to relieve the painful hyperkeratosis at the dorsal aspect of the distal interphalangeal joint as well as distally at the end of the toe. Surgical treatment is usually directed at the distal interphalangeal joint. The most common procedure is resection of the head of the middle phalanx through two transverse semielliptic skin incisions. Occasionally, flexion contracture is so severe that skin tension inferiorly at the distal interphalangeal joint or contracture of the flexor digitorum longus hinders correction. Simple transverse flexor tenotomy and capsulotomy can be performed through a plantar stab incision in the flexion crease. The tendon can also be released through the dorsal incision when arthroplasty is performed. Skin tension can be relieved by resection of appropriate amounts of bone. Occasionally, arthrodesis of the distal interphalangeal joint is required. This is usually accomplished by articular resection of both sides of the joint. Kirschner wire (K-wire) fixation generally does not need to cross the metatarsophalangeal joint. Postoperatively, the toe is bandaged and splinted in corrected alignment for 4 weeks. Appropriate supportive bandaging assists in reduction of edema while maintaining alignment as fibrosis of healing sets the joint in a rectus position.
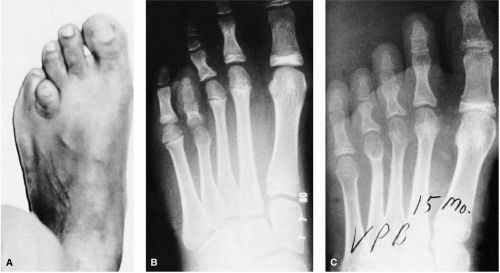
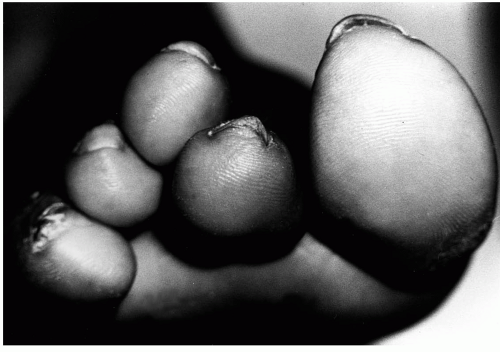
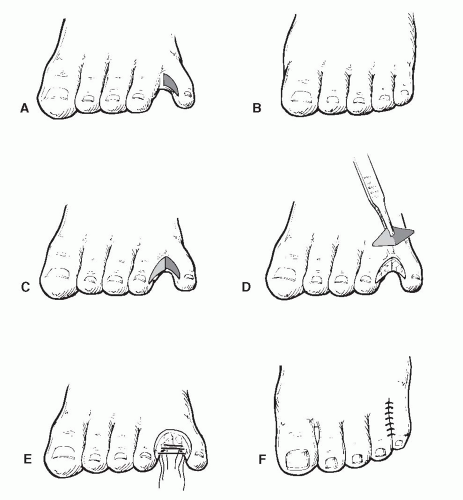
Curly Toes (Varus Toes)
Curly toes, or underlapping toes, are most often congenital. They often involve the third, fourth, and fifth toes, although sometimes all lesser toes may be affected. The deformity represents flexion and varus rotation of the distal phalanx at the interphalangeal joint. Some adduction is likewise present, and in more severe cases the proximal interphalangeal joint is also involved. Curly toes are often evident long before a child wears shoes or socks. They are seen with flexion, varus, and adduction of the distal aspect of the toe. They are usually bilateral.
Symptoms are usually related to hyperkeratoses that develop on the lateral side of the distal or proximal interphalangeal joints. Painful callus nail groove or Lister’s corn in the lateral nail groove (usually of the fifth toe) may develop as a result of transferring weight off the side of the underlapping toe. Radiographs show actual varus rotation of the phalanges, with medial deviation of the middle phalanx on the proximal phalanx or medial deviation of the distal phalanx on the middle phalanx.
Goals of treatment are to achieve a rectus digit, free of painful clavi, flexible enough to absorb shock and to allow
transference of weight during toe off. Surgical therapy is determined by the age of the patient, flexibility, and the degree of the deformity. When curly toes occur in infants, tape splinting of the toes may be adequate to effect correction. In flexible deformities in a child, tenotomy or derotational skin ellipses may be required (15). In the older child and adult with less flexibility in the deformity, varus rotation at the distal or proximal interphalangeal joint may require simple arthroplasty with a teardrop skin incision to assist in digital derotation. Flexor digitorum longus tenotomy may be necessary in some deformities. K-wires may be used for several weeks to encourage the digit to heal in a more rectus alignment. Postoperative toe bandaging and splinting are recommended for a minimum of 4 weeks.
transference of weight during toe off. Surgical therapy is determined by the age of the patient, flexibility, and the degree of the deformity. When curly toes occur in infants, tape splinting of the toes may be adequate to effect correction. In flexible deformities in a child, tenotomy or derotational skin ellipses may be required (15). In the older child and adult with less flexibility in the deformity, varus rotation at the distal or proximal interphalangeal joint may require simple arthroplasty with a teardrop skin incision to assist in digital derotation. Flexor digitorum longus tenotomy may be necessary in some deformities. K-wires may be used for several weeks to encourage the digit to heal in a more rectus alignment. Postoperative toe bandaging and splinting are recommended for a minimum of 4 weeks.
Hammer Toe
Hammer toe is probably the most common digital deformity and is principally a deformity occurring on the sagittal plane. The proximal phalanx is dorsiflexed, and the middle phalanx is plantarflexed. The distal phalanx is classically plantarflexed, but it may be extended at the distal interphalangeal joint. The metatarsophalangeal joint can be buckled plantarly, to create plantar protrusion of the metatarsal head (1). Hammer toe deformity is more frequently thought of as involving isolated toes.
Hammer toes have been widely attributed to wearing improper shoes and stockings. Whereas no doubt exists that foot gear does play a role, the biomechanical function of the foot is probably infinitely more important as a cause of disorders of the lesser toes and the lesser rays. One concrete but persuasive example of biomechanical influence is seen in the pronated foot with a hypermobile first ray. The hypermobility of the first ray results in loading of the second metatarsophalangeal joint. Chronic metatarsalgia commonly develops and results in chronic synovitis of the second metatarsophalangeal joint. Such synovitis maintains a chronic low-grade temperature increase within the joint that contributes to the weakening and eventual herniation of the retinacula that maintain the ordered relationship of the flexor plate to the metatarsophalangeal joint. The flexor plate along with the flexor tendons may slip medially, thus drawing the second toe into digital adduction and varus and resulting in an overlapping second toe. This condition and many others have all too frequently been attributed to wearing narrow or short shoes. No evidence supports foot gear as a cause. To the contrary, overwhelming evidence suggests biomechanical dysfunction as the genesis.
The unusually long second toe shows a significant tendency to develop hammer toe deformity. Investigators have postulated that deformity of the long toe is related to its subjection to greater shoe pressures. Whitney (unpublished data) has observed that whenever a toe is excessively long, it tends to contract until it functions in line with the adjacent toes. This result may indeed be influenced by the break line of the shoe and by the toe-off pressures. However, the condition has been perpetuated through numerous generations, as reported by Schuster in 1927 (1). It appears more probable that the inherited structure and resultant biomechanical dysfunction of the foot have far more to do with the deformity.
The long second toe perhaps best exemplifies the typical hammer toe, although any toe may be involved. The deformity may be present with a heloma on the end of the toe and a dorsal heloma over the proximal or distal interphalangeal joint or both. The deformity is frequently associated with long second or with long second and third metatarsals. A plantar lesion may be pressure beneath the second metatarsophalangeal joint associated with plantar protrusion of the metatarsal head.
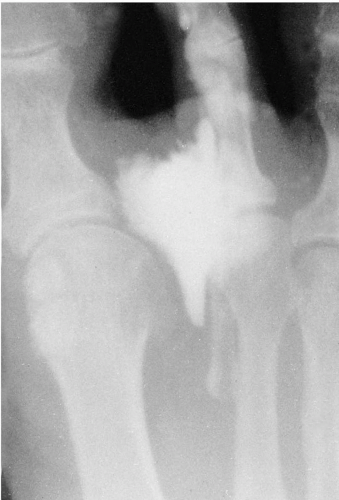
Radiographic findings confirm a dorsiflexed proximal phalanx with flexion of the middle and dorsiflexion of the distal phalanx. With long-term adaptation of the joints, degenerative changes can occur in the interphalangeal and metatarsophalangeal joints. In more severe deformities, dislocation of the metatarsophalangeal joint may be evident.
Surgical treatment for an isolated hammer toe is directed at reestablishing a rectus alignment to the toe, shortening the toe if necessary to place it in appropriate length relative to its two adjacent toes, and providing sufficient stability to resist recurrence if the deforming forces persist. When deforming forces on the toe have been removed or neutralized, resection arthroplasty with appropriate shortening may be an ideal solution. However, when deforming influences are expected to continue, arthrodesis of the proximal interphalangeal joint provides much greater stability and improved leverage for the long and short flexor tendons to assist metatarsophalangeal joint stability. Occasionally, a combined hammer toe-mallet toe (double corn) deformity occurs that requires a double resection arthroplasty (16) or a proximal interphalangeal arthrodesis with a distal interphalangeal arthroplasty. This usually occurs in a patient with a pronated foot type undergoing flexor stabilization contracture. In patients with lesser forms of distal contracture with proximal lesions, the shortening that accompanies the hammer toe repair may relax the long flexor tendon so the contractile force is reduced at the distal interphalangeal level.
Claw Toe
Claw toe is a deformity in which the middle and distal phalanges are flexed on a markedly dorsiflexed proximal phalanx. The metatarsophalangeal joint is buckled plantarly. The deformity usually is more severe than hammer toe. True claw toe deformity is often associated with cavus foot deformity or neuromuscular conditions.
Claw toe deformity most often involves all the lesser toes, with the hallux included in a substantial percentage of patients. It is always associated with dorsal contracture of the metatarsophalangeal joints and plantar contracture of the interphalangeal joints.
Plantar protrusion of the metatarsophalangeal joints is evident, and with adaptive changes in the joints and soft tissue contractures, the metatarsals function in their position of maximum plantarflexion. This situation exaggerates any
cavus deformity that may be present. Hyperkeratosis and painful metatarsalgia beneath the metatarsal heads are the rule. Late changes in the metatarsophalangeal joints frequently include subluxation or dislocation.
cavus deformity that may be present. Hyperkeratosis and painful metatarsalgia beneath the metatarsal heads are the rule. Late changes in the metatarsophalangeal joints frequently include subluxation or dislocation.
In the early and more flexible stages of the deformity, the toes straighten on weight bearing or with the push-up test loading of the metatarsals. In later stages of contracture, the interphalangeal joints flex when the metatarsals are loaded, but the metatarsophalangeal joints fail to straighten.
Radiographic changes vary with the degree of rigidity of the deformity. In earlier stages, the deformities appear most severe on non-weight-bearing films. In later stages, the deformities are exaggerated with weight bearing. Findings generally demonstrate dorsiflexed positions of the proximal phalanges and plantarflexed positions of the middle and distal phalanges. Often, a positive gun barrel sign is displayed with the x-ray projection of the dorsoplantar view looking directly down the shafts of the proximal phalanges. Treatment objectives include not only restoration of rectus alignment of the toes but also establishment of stability of the digit to resist redeformity.
Digitus Adductus
Digitus adductus occurs principally on the transverse plane and represents adduction of the toe at either the interphalangeal or metatarsophalangeal joint. With the passage of time, sagittal plane deformity may also develop. Congenital digitus adductus more often involves an adduction deformity of the distal phalanx with the middle phalanx less frequently affected. Acquired digitus adductus is usually related to metatarsophalangeal joint derangement or to iatrogenic or traumatic causes. Metatarsophalangeal joint derangement usually involves deformity in three planes and is a complex condition.
Digitus Abductus
Digitus abductus is the opposite of digitus adductus, with the deformity representing abduction of the digit at either the interphalangeal or the metatarsophalangeal joint. These transverse plane deformities usually represent congenital deformities when the deformity occurs at the interphalangeal joints, or they may result from derangement of the tendons and flexor plate when the deformity occurs at the metatarsophalangeal joint. The latter circumstance commonly occurs with rheumatoid arthritis.
Heloma Molle
Heloma molle (soft corn) is commonly associated with the underlapping fifth toe or with adductus deformity of the fifth metatarsophalangeal joint. Typically, the head of the proximal phalanx of the fifth toe is displaced against the lateral condyle of the base of the fourth proximal phalanx. Radiographic changes frequently show bone adaptation of both the base of the fourth proximal and the head of the fifth proximal phalanges. The heloma may also occur at the distal interphalangeal joint of the fifth opposed by the proximal interphalangeal joint of the fourth. Less frequently, it occurs between the third and fourth toes or the second and third. It can even occur between the first and second toes.
Clinical presentation is a painful lesion on one or both sides of the proximal or distal interphalangeal joints or an interdigital clavus at the web space. Toes may not necessarily be hammered or clawed. The fourth toe may be longer or shorter than usual, thus altering the normal convex-to-concave relationship between the toes. When the fourth or fifth digit is long, lesions are prevalent on the dorsum of the toes as well. With chronicity, large hyperkeratoses can develop and may become infected. Intertrigo and sinus tracts leading from the hyperkeratosis to bone are common.
Often the fourth and fifth toes are long and in varus. Exostoses, or bony prominences, may be evident beneath corresponding pressure areas. The fifth metatarsal may be short, thereby causing the phalanges of the fifth digit to rest further proximal and resulting in the pathologic features previously described. The latter is most commonly the condition that causes the deep interdigital web-space heloma molle. In other patients, one may note a synostosis between the middle and distal phalanges of the fifth, and occasionally, the fourth toe. This condition reduces flexibility of the digit and renders the area more susceptible to irritation and subsequent lesion formation.
Surgical treatment is directed at remodeling of the head of the proximal phalanx of the fifth toe and resection of any bony prominence from the lateral condylar base of the fourth proximal phalanx. In patients with interdigital lesions located distally, condylectomies on the adjacent digits, or a combination of an arthroplasty of the fourth toe with an condylectomy of the fifth toe, may prove successful. In recalcitrant cases, total phalangectomy or syndactyly is sometimes used.
METATARSAL DISORDERS
Disorders of purely metatarsal origin occur, but they are much less common than generally believed. Some of these conditions, such as osteochondrosis and brachymetatarsia, are described in other segments of the text.
Metatarsal Cavus (Equinus)
Metatarsal cavus, or the so-called plantar declinated lesser metatarsal, does occur on rare occasion as a purely developmental condition. More often, the condition termed metatarsal cavus (equinus) is merely a metatarsal that is plantar declinated as a result of plantar buckling of the metatarsophalangeal joint caused by retrograde force from a contracted and deformed toe. A metatarsal cavus is an excess plantar declination of the metatarsals with the apex of the deformity seen at Lisfranc’s joint. If the apex of the deformity is at Chopart’s joint, the deformity is called a forefoot cavus (equinus).
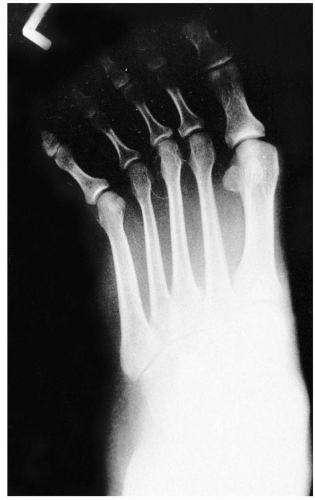
Long Metatarsals
Long metatarsals occur rarely, and unless they are extremely long, they produce minimum difficulty except when associated with plantar declination. When substantially longer than the adjacent metatarsals, they may become symptomatic. A long metatarsal may be associated with an abnormally long toe. The tendency is for the long toe to contract gradually until its tip functions in line with the ends of the adjacent toes. Such a tendency may be associated with the break point of the toe of the shoe or with biomechanical accommodation. With the long toe functioning in a contracted position, retrograde force is placed against the metatarsal head, and the long metatarsal protrudes plantarly, thus receiving increased trauma.
Long metatarsals are hereditary, seen in one generation after another, but they may be unrecognized as a problem until after maturity, when the added weight bearing on the particular metatarsals begins to result in secondary digital deformities and metatarsalgia.
The most common long metatarsal bones are the second or the second and the third. In patients with long second and third metatarsal bones, long second and third toes are likewise noted. Symptomatic callus and metatarsalgia beneath the second and third metatarsal heads may be evident. These lesions are usually slightly more distal under the metatarsal heads as propulsive lesions. If the toe is contracted, the resulting force may be located more directly plantar to the metatarsal head. The second and third toes may show contracture, and fixed contractures may develop in time. As the toes contract into hammer toe deformity, retrograde force against the metatarsals forces them plantarly and exaggerates their already excessive length. When the deformity has been present for a prolonged period without adequate accommodation, dislocation of the metatarsophalangeal joints and contracture of all the lesser toes may be found.
Radiographic findings confirm the digital deformity and the long second and third metatarsal bones. Treatment is directed at reestablishing a rectus alignment of the toes and providing sufficient stability of the digit to allow the long and short flexor function to maintain metatarsophalangeal joint alignment. Metatarsal shortening or osteotomy may be necessary.
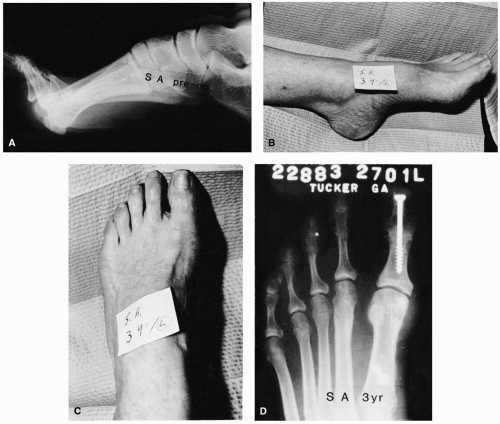
Brachymetatarsia
Brachymetatarsia (short metatarsal) or brachymetapody (multiple short metatarsals) occurs infrequently as a result of premature closure of the growth center of a metatarsal or metatarsals (17,18). As the other metatarsals continue to grow, the difference in length becomes exaggerated, and the condition becomes clinically manifest (Fig. 24). Brachymetatarsia
can also result from trauma to a metatarsal that then results in premature closure of the growth center.
can also result from trauma to a metatarsal that then results in premature closure of the growth center.
The condition apparently is largely hereditary and does result in substantial overloading of adjacent metatarsals. The short metatarsal bears no weight. Consequently, its flexor plate fails to load on weight bearing, and the result is an unstable and floating digit. The adjacent metatarsals may present with metatarsalgia and plantar keratosis, especially in the adult patient. A deep sulcus is usually found beneath the involved short metatarsal. Adjacent toes tend to migrate into the space vacated by the floating toe. Failure of the extrinsic tendons to load on the short ray results in an increased loading on the other toes, and some degree of digital deformity of the adjacent toes usually results. Although most often genetic in origin, the condition often goes unrecognized until premature closure of the involved growth center.
Radiographic findings include a short, underdeveloped metatarsal, at times with deficient bone content in general and with osteoporosis of the metatarsal head in particular. The toe is usually straight but in an extended position, and it floats above the weight-bearing plane.
Historically, surgical treatment has consisted of the insertion of bone grafts in an attempt to lengthen the metatarsal (17). However, in most instances today the lengthening is performed by callus distraction (19, 20, 21, 22, 23, 24, 25, 26, 27). Surgical treatment of the condition is discussed in Chapter 67.
LESSER METATARSOPHALANGEAL JOINT DERANGEMENT
Lesser metatarsophalangeal joint derangement occurs in various different forms, many of which are directly related to simultaneously occurring digital deformities.
Flexor Dislocation
Flexor dislocation is a condition in which the flexor tendons dislocate distally or to the medial or lateral side of the metatarsal head. The derangement can be caused by chronic inflammation of a lesser metatarsophalangeal joint that results in weakening or herniation of the retinacula that maintain the stability of the flexor plate to the metatarsal head. The flexor tendons may dislocate medially or, less frequently, laterally and may result in drawing the toe into varus or valgus rotation and often overlapping the adjacent toe. The tendons may also become attenuated or ruptured in the sagittal plane, and this condition may lead to instability of the metatarsophalangeal joint.
Once the flexor tendons have dislocated to the medial or lateral side of the joint, they exert their influence to draw the toe and the joint in that direction. The extensor tendons are left unopposed, and they begin to create dorsal contractures. A dorsoplantar radiograph usually demonstrates rotation of the proximal phalanx, so the plantar aspect of the phalangeal base is profiled medially or laterally. The articular base of the proximal phalanx is displaced medially or laterally, and the metatarsal head is displaced in the opposite direction.
Metatarsophalangeal Joint Adductus or Abductus
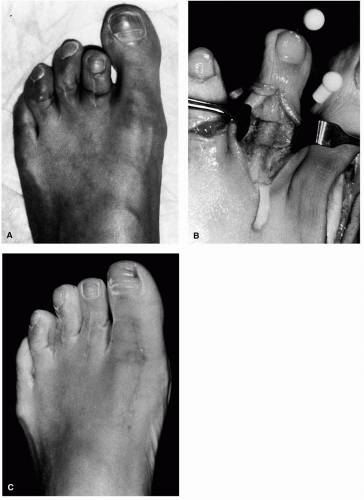
When deranged metatarsophalangeal joints are present, the patient may present with overlapping second or second and third toes (Fig. 25). This condition frequently indicates a medially displaced flexor tendon (Fig. 26). The clinical examination shows obvious medial displacement and usually some torsion or varus rotation of the toe.
In medially displaced or adductus deformities, the cause is usually mechanically induced synovitis that results in
weakening of the supportive structures of the joint. The opposite deformity is seen in patients with rheumatoid arthritis in whom lateral dislocation or deviation is the rule. Regardless of the direction of the metatarsophalangeal joint derangement, digital deformities may be present as claw toes or hammer toes.
weakening of the supportive structures of the joint. The opposite deformity is seen in patients with rheumatoid arthritis in whom lateral dislocation or deviation is the rule. Regardless of the direction of the metatarsophalangeal joint derangement, digital deformities may be present as claw toes or hammer toes.
The push-up test shows adduction or abduction of the toes at the metatarsophalangeal joint (rather than the usual flexion) (28). Moreover, stimulation of the plantar reflex results in digital adduction or abduction, rather than flexion.
The longer the condition is present, the more severe and fixed the contractures tend to become. The more severe the deformity, the more difficult is the correction. A strong argument can therefore be made for early surgical correction. As with all digital deformities, the tendency is toward a corresponding increase in plantar metatarsal protrusion. This increased protrusion is largely responsible for the development of metatarsalgia and intractable plantar keratosis in such patients.
Treatment is directed at restoration of metatarsophalangeal joint alignment and replacement of the flexor structures beneath the metatarsal head. In some instances, this may be accomplished with a variety of capsular release and plication techniques. The digit may be stabilized by arthrodesis of the proximal interphalangeal joint. Such arthrodesis allows the long and short flexors to contribute to maintaining metatarsophalangeal joint reduction. Flexor tendon transfers may be employed, particularly if the patient has dorsal metatarsophalangeal joint instability. In more difficult or recurrent cases, resection of the base of the proximal phalanx and syndactylization may prove more effective.
When metatarsophalangeal joint arthrosis is present, treatment may include implant arthroplasty, appropriate resection arthroplasty, and possible stabilization arthrodesis of the digits. An important consideration is to maintain alignment until healing is complete.
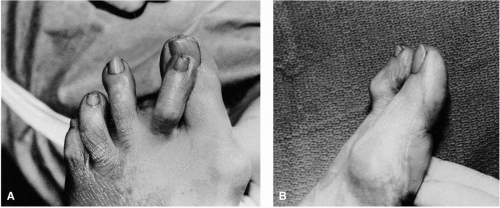
Metatarsophalangeal Joint Limitation
Limitation of motion of the lesser metatarsophalangeal joints occurs as a result of degenerative change in and around the joint. Limitation can occur after relocation of a dislocated joint if sufficient degeneration of the articular cartilage has occurred. Such degeneration can provide an anchor for capsular tissues that, once attached, prevents smooth motion and effectively limits active or passive dorsiflexion of the metatarsophalangeal joint. More often, lesser metatarsophalangeal joint limitation results from chronic synovitis of the joint related to multiple continuing traumas and to biomechanical dysfunction, a localized form of overuse syndrome. With time, the chronic inflammation is able to cause the plexor plate to adhere to the margin of the metatarsal neck, and thus dorsiflexion is limited.
Plantarflexion can likewise be limited by dorsal capsular scarring or contracture (Fig. 27). Limitation of plantarflexion of the joint produces plantar protrusion of the metatarsal head and a floating toe. In addition, the digit becomes unstable because of the absence of loading of the flexor plate to the base of the proximal phalanx. Instead, the loading is shifted to the metatarsal neck, and it fails to render stability to the toe.
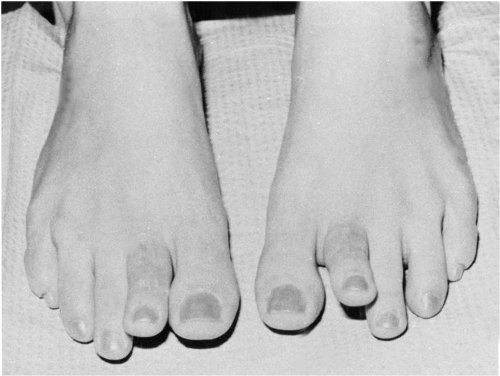 FIG. 27. Two months after routine proximal interphalangeal joint arthroplasty, severe dorsal contracture of the extensor structures has created this floating toe. |
Radiographic findings include narrowing of the metatarsophalangeal joint space and often flattening of the metatarsal head. Commonly, the condition is associated with a dislocated or subluxed metatarsophalangeal joint. Surgical objectives are reduction of the joint if it is dislocated, release of the flexor plate if it is attached, resection or implant arthroplasty if substantial arthrosis is present, and possible stabilization arthrodesis of the digit to encourage more stable metatarsophalangeal joint function. Tendon balancing techniques may be required. These range from simple lengthening of the extensor digitorum longus to transposition of the extensor digitorum longus into the corresponding metatarsal neck area or flexor digitorum transfer to the proximal phalanx. If the flexor plate has been destroyed, either arthroplasty or implant arthroplasty may be necessary along with tendon balancing techniques. Aftercare must include early range-of-motion exercises of the metatarsophalangeal joints. If K-wires are used, they either should not cross the metatarsophalangeal joints or should be retracted from across the joints by 21 days postoperatively. In either event, range-of-motion exercise should be actively pursued at 3 weeks after surgery. Failure to institute exercise often results in recurrent fibrosis of the flexor plate and joint limitation.
Predislocation Syndrome of the Lesser Metatarsophalangeal Joint
Predislocation syndrome of the lesser metatarsophalangeal joint presents as an acute or subacute inflammatory condition localized to the plantar aspect of the joint. Yu and Judge indicated that the tenderness is localized to the periarticular structures plantar and distal to the metatarsophalangeal joint (29). This finding is in contrast to the intraarticular disease and painful motion usually associated with degenerative joint disease or with digital contractures. The pain associated with the plantar capsulitis is generally out of proportion to the clinical presentation, which may show minimal digital contracture or instability. Mild edematous changes may be obvious only after close comparison with the opposite foot. A benign history is commonplace, without any indication of acute trauma. Often, a recent increase in activity or a routine of a high level of activity such as aerobics or running is noted.
Many patients describe the feeling of walking on a pebble or lump on the bottom of their foot. The associated pain can be sharp to throbbing or bruiselike soreness. Severe pain may be reproduced by vertical displacement of the proximal phalanx on the metatarsal. Coughlin indicated that a vertical shift of more than 50% of the proximal phalanx on the metatarsal head is considered a positive test (30). Because the pain may be intense, the patient may contract the muscles so the phalanx may not be shifted. If the test is positive, the patient may not allow the test to be performed more than once.
Standard radiographs, bone scans, magnetic resonance imaging, and arthrography are usually of little assistance in making the diagnosis, but these methods may be helpful in ruling out other causes of pain. Radiographs may be normal. Bone scans may be most pronounced in the initial flow phase or inflammatory phase and may have some increased uptake in the third phase. Magnetic resonance imaging studies may show edematous changes around the joint structures, especially noted on T2-weighted images. Careful clinical history and physical examination with a high index of suspicion are usually adequate to make the diagnosis.
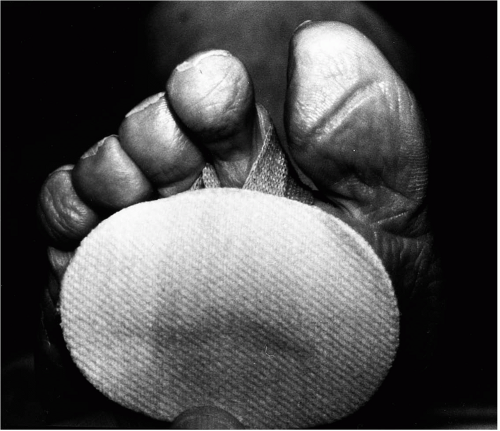
The goals of therapy are to reduce pain and to interrupt the progression of deformity. Pads and splints may be employed from simple dorsiflexion-limiting strapping or padding or buttress padding to shift weight-bearing stress to the adjacent metatarsals. Antiinflammatory medications or a short course of oral prednisone can be initiated. An oral dose of 80 mg of prednisone that is decreased by 10 mg per day may be adequate as a short course of antiinflammatory treatment to arrest the acute symptoms. A limited number of local cortisone injections may be used. Crossover taping can significantly limit the dorsiflexion of the metatarsal phalangeal joint. However, dorsiflexion limitation may be required for months, a finding suggesting that a removable splint is more practical after the initial treatment phase. A simple tubegauze moleskin sling pad (Fig. 28), a Budin splint, or a Darco Velcro digital pad can be used to limit dorsiflexion of the metatarsophalangeal joint. Orthotic devices may also be helpful in redirecting forces across the forefoot and in limiting stress to the affected joint. When subluxation or dislocation has already occurred at the metatarsophalangeal joint, then surgical correction may be the only logical treatment. This may include a flexor tendon transfer with relocation of the metatarsophalangeal joint and temporary K-wire fixation or release of the joint and capsular plication. Proximal phalangeal joint arthrodesis may also be considered (29, 30, 31).
METATARSOPHALANGEAL JOINT DISLOCATION
Metatarsophalangeal joint dislocation may occur as a result of acute or chronic trauma. Acute traumatic dislocation is infrequent. Chronic continuing trauma such as that experienced daily in a biomechanically unsound forefoot is a much more frequent cause. Early in the course of this condition, the clinical presentation may be pain at the joint associated with a mild swelling that can only be noticed by careful comparison with the opposite foot (predislocation syndrome). As the clinical presentation progresses, the metatarsal head becomes more plantarly prominent. A painful plantar keratosis is often present beneath the head. The patient is unable to dorsiflex and plantarflex the metatarsophalangeal joint actively through a normal range of motion. The push-up test shows some flexion of the interphalangeal joints but no realignment of the metatarsophalangeal joint. Passive motion may be possible but is of poor quality. Dorsiflexion of the joint is sharply limited.
Radiographic examination confirms the dislocation. The dorsoplantar radiograph shows superimposition of the base of the phalanx on the metatarsal head. The oblique view accurately assesses the degree of telescoping of the phalanx over the metatarsal and likewise gives an excellent appraisal of the plantar condyles of the metatarsal head.
Treatment objectives are much the same as those described for metatarsophalangeal joint limitation. Relocation of the joint is usually possible if the flexor plate is reasonably intact. When the flexor plate is badly damaged, implant arthroplasty or resection arthroplasty or resection of the base of the proximal phalanx with syndactyly is often necessary. In either instance, arthrodesis of the proximal interphalangeal joint may be required to provide a stable lever on which the long and short flexors can function to help stabilize the metatarsophalangeal joint.
SURGICAL MANAGEMENT OF DIGITAL DEFORMITIES
Various different procedures may be employed for the repair of hammer toe deformities. If the cause of the deformity is understood, then one may be able to determine the stability that may be required to neutralize the deforming forces (32). During normal propulsion, the digit must be stable in a rectus position on the supporting surface. This requires stability of the proximal, middle, and distal phalanges. For the rigid beam effect to occur, the muscles of the foot will need to fire in proper sequence. Whenever this sequence is disrupted, the toes lose their ability to purchase the ground from that point distally (4,6). In flexible deformities, these forces may at times be neutralized biomechanically. Less extensive surgery may be effective if the deforming forces can be neutralized by mechanical means in the postoperative setting. In a patient with a forefoot varus and hammer toes resulting from flexor stabilization, an orthotic support may work well in the postoperative setting to control the deforming forces. However, swing-phase extensor substitution is difficult to control with mechanical measures because functional orthoses primarily exert an influence during the stance phase of gait. Therefore, these orthoses are ineffective in extensor substitution. Definitive surgery, such as the Hibbs suspension or arthrodesis of the proximal interphalangeal joint, may be more practical. In patients with extensor substitution, simple proximal phalangeal head resection or soft tissue release may lead to recurrence of the deformity.
Other considerations are necessary when dealing with digital deformities. Digital length patterns, congenital deformity of the digits, prominent exostoses, shoe gear considerations, and adductovarus deformities all need to be considered. In providing surgical correction for the hammered-digit syndrome, both adequate intraoperative reduction of the deformity and the effectiveness of postoperative neutralization of the deforming forces must be considered.
Soft Tissue Surgery for Deformed Lesser Toes
Tenotomy
Tenotomy of a segment of the extensor or flexor digitorum longus tendons can eliminate the effects of these structures on that toe. Such an effect is generally temporary because the tendon tends to heal by bridging the gap created by the tenotomy. The procedure is occasionally indicated in the pediatric or the elderly patient in whom more definitive surgical correction is contraindicated. An orthodigital retainer is suggested until healing is complete and the toe appears stable in the new position.
Procedure
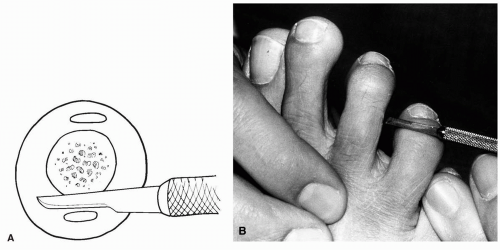
The approach to simple extensor tenotomy is usually proximal to the metatarsophalangeal joint. A No. 15 scalpel blade or a No. 67 Beaver blade is used to make a small stab incision just medial or lateral to the tendon. The knife blade is slipped percutaneously beneath the tendon, and it is rotated 90 degrees to face the underside of the tendon. With the knife held securely in that position, the surgeon firmly plantarflexes the toe at the metatarsophalangeal and interphalangeal joints. The tendon is severed as it is stretched across the knife blade. Flexor tenotomy is usually performed at the head of the proximal phalanx or the head of the middle phalanx. A stab incision is made with a small blade just medial or lateral to the tendon. The blade is slipped deep to the tendon and is rotated 90 degrees. The toe is gently dorsiflexed until the tendon is severed. A simple suture or two closes the skin but is often not necessary.
Aftercare
Discussion
Tenotomy as an isolated procedure has limited usage. First, the tendon tends to regenerate in most instances. Second, unless the toe alignment is effectively controlled while regeneration is occurring, the tendon contractures may result in a worse deformity than was present originally.
Loading phenomenon, or the transfer of tendon load to an adjacent tendon, provides additional loading to an adjacent toe or toes when a tenotomy or tendon lengthening is performed. Because the four long extensors and the four long flexor tendons to the lesser toes originate from a common muscle belly, when one tendon is released by tenotomy, each of the remaining tendons will have one-third more force on it. This loading phenomenon can be observed during surgery and often necessitates performing a tenotomy or tendon lengthening in all the toes to prevent subsequent deformity of the nontreated toes.
Extensor Tenotomy and Capsulotomy
Tenotomy and capsulotomy as isolated procedures are used in those patients in whom the deformity is semi-flexible. The procedures are often used as a part of a more complex surgical correction. The isolated procedures are sometimes indicated in the older patient who cannot undergo reconstructive surgery but who, with appropriate supportive follow-up, may obtain years of help from simple releases.
Procedure
The approach is similar to that used for tenotomy, but a 1- to 2-cm linear skin incision is recommended to permit direct visualization over the metatarsophalangeal joint. If the tendon is severed at the joint level, the extensor hood must usually be released to obtain full benefit of the release. Severing the tendon proximal to the hood fibers accomplishes the same effect. Once the tendon has been severed, the toe is placed under distal traction, to result in a dorsal transverse dimpling of the metatarsophalangeal joint capsule. The surgical blade is introduced into the transverse dimple of capsule while the toe is held distracted. This approach permits sectioning of the capsule medially, laterally, and dorsally without damaging the articular cartilage. Closure is by one or two simple sutures in the skin.
Aftercare
The postoperative bandaging and splinting protocol is similar to that for tenotomy.
Discussion
Extensor tenotomy and metatarsophalangeal joint capsulotomy are simple, relatively atraumatic procedures that are considered palliative rather than corrective surgery. However, they should not be viewed as completely innocuous. As with tenotomy, severing of a single tendon results in increased load (loading phenomenon) to each of the other divisions of that same tendon. The adjacent toe apparently is affected most. When two extensor tendons are severed, the tension to the two remaining ones is doubled, and the possible result is immediate or gradual dynamic deformity. The surgeon should be prepared to perform tenotomy or appropriate lengthening on all divisions of the extensor digitorum longus tendons whenever tenotomy is performed on one division. If there is clinical evidence of loading phenomenon, then the additional tenotomies are suggested.
Flexor Tenotomy and Capsulotomy
Tenotomy of the flexor digitorum longus tendon is rarely performed as an isolated procedure in the adult, but it may be done in isolation in the young child. More often, flexor tenotomy and capsulotomy of the interphalangeal joint are combined with extensor tenotomy and metatarsophalangeal joint capsulotomy. As with other tenotomy procedures, flexor tenotomy and capsulotomy find greatest application in the young child or in the older patient in whom more definitive reconstructive surgery is not possible. Flexor tenotomy does sacrifice some digital purchase. This is rarely a problem in the older patient in whom an apropulsive gait is already present, but it may be a problem in the younger patient.
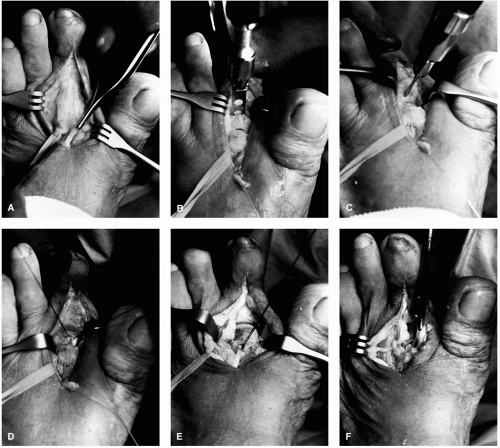
Procedure
The approach is through a medial or lateral percutaneous incision along the side of the toe or through a plantar stab incision directly beneath the interphalangeal joint. The flexor retinaculum that binds the tendons to the underside of the phalanges is incised. The surgical blade is rotated to face against the plantar side of the tendon. The toe is placed on stretch, and the tendon and capsule are severed. The interphalangeal joint is manipulated into hyperextension. The skin incision may be closed with one or two simple sutures, but often these are not necessary (Fig. 29).
Aftercare
The toe is bandaged and is splinted in corrected alignment for a full 3 to 4 weeks. A postoperative retainer can then be worn for an additional period. Range-of-motion exercises of the metatarsophalangeal joint may be instituted to enhance flexibility of the joint.
Discussion
Wherever hammer toe deformity is present, the long flexor tendon is converted to a dorsiflexor of the metatarsophalangeal joint because the phalanges cannot be plantarflexed through the ground. Once the metatarsophalangeal joint is dorsiflexed, the flexors become responsible for the flexion deformity of the interphalangeal joints. Flexor tenotomy and capsulotomy alone or, when appropriate, in conjunction with other procedures can remove the retrograde deforming force. The procedure and orthodigital support can provide years of improved comfort with minimal surgical trauma. In the absence of orthodigital follow-up, the toes may tend to redeform. Digital purchase or toe off is sacrificed, but this is rarely a problem in the older patient. Like the extensor tenotomy and capsulotomy, the flexor tenotomy and capsulotomy are considered palliative rather than corrective surgical procedures.
Extensor Tendon Lengthening
Rarely is an extensor tendon lengthening done as an isolated procedure. The indications and the results are similar to those for the tenotomy procedures. The major difference is that the amount of tendon lengthening can be controlled with a Z-plasty technique. Care must be taken to evaluate the transfer loading that occurs on adjacent tendons.
Procedure
A small incision is made over the extensor tendons proximal to the extensor hood over the third metatarsal shaft area. The peritenon tissue is incised over each extensor digitorum longus tendon in turn. Individual Z-plasty lengthening is performed and is secured with simple suture technique, and the wound is closed.
Aftercare
The patient is treated with bandaging and splinting in the same manner as after tenotomy.
Discussion
Extensor tendon lengthening procedures are simple, relatively atraumatic procedures that are considered palliative rather than corrective surgery. However, they should not be viewed as completely innocuous. As with tenotomy, the lengthening of a single tendon results in increased loading phenomenon to each of the other divisions of that same tendon. The surgeon should be prepared to perform appropriate lengthening on all divisions of the extensor digitorum longus tendons whenever tendon lengthening is performed on one division. If there is clinical evidence of loading phenomenon, then the additional tenoplasties are recommended.
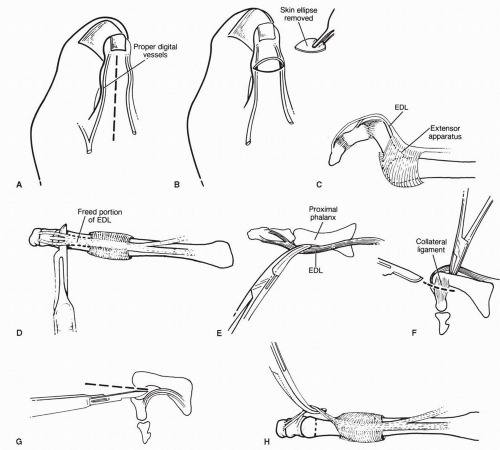
Flexor Tendon Transfer
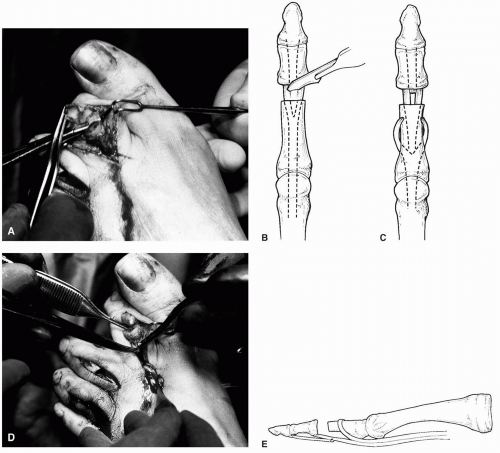
Forrester-Brown, in 1928, used transfer of the long flexor tendon to the extensor tendons to replace lost intrinsic function to the hallux (33). In 1947, Girdlestone transferred flexor digitorum longus and brevis tendons into dorsal expansions of the extensor tendons (34). The theory was that
the flexor muscles would take over the function of the lost intrinsic muscles. Taylor reported performing the same procedure on 112 feet (35). He followed 68 of these surgical cases. Thirty-seven were cavus feet, and 27 were valgus feet; 59 feet had good results.
the flexor muscles would take over the function of the lost intrinsic muscles. Taylor reported performing the same procedure on 112 feet (35). He followed 68 of these surgical cases. Thirty-seven were cavus feet, and 27 were valgus feet; 59 feet had good results.
Pyper reviewed 45 feet in which flexor transfer had been performed and found an almost equal number of good and poor results (36). Best results were obtained in patients with the mildest deformities. He found a straight digit with loss of interphalangeal joint motion resulted. The toe was converted to a rigid lever on which the long extensors and flexors could work at the metatarsophalangeal joint. For this reason, he recommended proximal interphalangeal joint arthrodesis as a better alternative.
Sgarlato reported on 53 cases of flexor transfers. He used 2 different techniques (37). He severed the flexor digitorum longus tendon from its attachment to the distal phalanx, split it longitudinally, and attached it as a sling over the proximal phalanx. It was sutured to itself and to the extensor expansions over the proximal phalanx. Pain associated with dorsal clavi was completely relieved, and impressive results were reported in repositioning the phalanx on the metatarsal head and in repositioning the plantar fat pad. He reported a single “elevated and fat toe.”
Barbari and Brevig reported on 39 operations using the Girdlestone-Taylor-type procedure (38). In 28 operations, these surgeons used Parrish’s modification in which the long flexor tendon was split longitudinally and the ends were sutured to themselves and to the dorsal expansion of the extensor tendon (39). Best cosmetic results were reported in younger patients, although this group complained most of toe stiffness. The elderly patients did not complain of stiffness, even though motion was decreased or absent. Results were considered satisfactory in 28 of 31 patients. However, when metatarsalgia was the dominant preoperative complaint, no improvement was noted, even though the toe was straight and the range of motion was acceptable.
Kuwada and Dockery reported a modification of the flexor transfer in which the flexor tendon was brought through a drill hole in the anatomic neck of the proximal phalanx (40). Kuwada found this transfer effective in cavus foot structures when other procedures failed to reduce the hammer toe deformities (41). Schuberth transferred the flexor digitorum longus tendon through a drill hole at the base of the proximal phalanx (42) (Fig. 30). He believed that attaching the flexor at the base of the proximal phalanx was more anatomic. This approach also allowed for arthrodesis of the proximal interphalangeal joint.
Flexor transfer to the extensor hood has been employed in patients with myelodysplasia with flexible hammer toe deformities. These patients had residual paralysis from myelomeningocele (43). Results of tendon transfer without bone surgery were good to fair in 94% of the cases. Marcinko and associates reported the modification used when flexor tendon transfer is performed as an isolated procedure without an associated arthroplasty or arthrodesis of the proximal interphalangeal joint (44) (Fig. 31).
Procedure
When this operation is performed as an isolated procedure, two skin incisions are employed, one on the side of the digit that provides the most exposure and the other over the dorsum of the base of the proximal phalanx but on the opposite side from the first incision. The incision on the side of the toe is usually medial on the second toe and lateral on the third, fourth, and fifth toes, to provide the greatest exposure.
The medial or lateral incision is carried from the web space to the distal interphalangeal joint. The incision is between the dorsal and plantar neurovascular bundles. Sharp dissection is used to open the retinacula that bind the flexor tendons to the underside of the phalanges. The flexor longus tendon is traced distally and is severed close to its attachment to the distal phalanx.
The long flexor tendon is split longitudinally to the base of the proximal phalanx. One slip is tagged with a straight hemostat and the other with a curved hemostat. A tenotomy is performed on the flexor digitorum brevis tendon in cases of extreme contracture.
The second incision is made dorsomedially or dorsolaterally, but on the side opposite to that on which the first incision is made. The incision is deepened to the periosteal level. A channel is created, with a periosteal elevator passed medially and laterally around the bone but superficial to the periosteum.
A curved pediatric hemostat is introduced first through
one channel and then through the other, and the tendons are drawn dorsally adjacent to the phalanx. The tendons are crossed to create a sling and are tightened appropriately. They are then sutured to themselves with 3-0 nonabsorbable braided suture. They are also sutured to the extensor expansions. Excess tendon is cut away. Skin closure may be accomplished with several interrupted sutures.
one channel and then through the other, and the tendons are drawn dorsally adjacent to the phalanx. The tendons are crossed to create a sling and are tightened appropriately. They are then sutured to themselves with 3-0 nonabsorbable braided suture. They are also sutured to the extensor expansions. Excess tendon is cut away. Skin closure may be accomplished with several interrupted sutures.
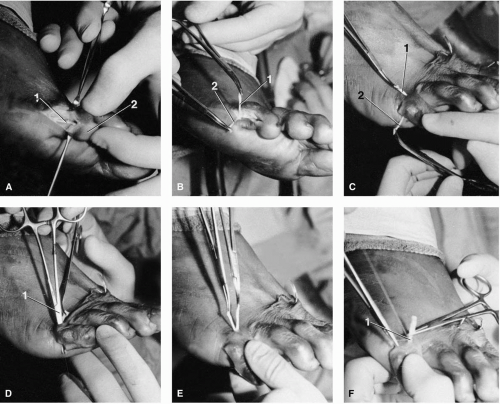 FIG. 31. Flexor digitorum longus (FDL) transfer. A: The FDL tendon (1) is isolated by a lateral approach to the fifth digit (2). B: The FDL has been sacrificed from its insertion into distal phalanx and longitudinally divided into medial (1) and lateral (2) portions. C: A dorsal incision is placed over the proximal phalanx. The medial tendon segment is redirected medial to the proximal phalanx but inferior to the neurovascular structures exiting the dorsal incision. 1, FDL medial portion; 2, FDL lateral portion. D: A curved mosquito hemostat (1) is used to grasp and redirect the lateral portion of the tendon. E: Both tendon portions now exit the wound dorsally. F: With the proximal phalanx in a rectus position, the FDL tendon segments are sutured (1) around the proximal phalanx under physiologic tension. Excess tendon is then excised. |
When the flexor transfer in performed in conjunction with osseous procedures, access to the flexor tendon is much easier. The tendon can be easily located plantarly once the head of the proximal phalanx has been freed. A linear incision is made in the plantar capsule of the proximal interphalangeal joint, and the long flexor tendon is isolated from the brevis (Fig. 32). The tendon is transected and is freed proximally for transfer through a drill hole in the proximal phalanx or is split and delivered dorsally around each side of the shaft of the proximal phalanx. The tendon is secured under appropriate tension. The stump of the long flexor tendon can be sutured to the short flexor tendon at the proximal interphalangeal joint if desired. Typically, the normal skin incision for the osseous procedure is adequate for the tendon transfer as well.
Aftercare
Postoperative bandaging is used to retain the toes and metatarsophalangeal joints in corrected alignment for 3 weeks. After that, digital retainers are used if needed.
Complications
Complications have included an occasional fat toe, with edema sometimes lasting for several months. We have also seen a reverse deformity in which the toe developed a reverse curve or swan’s neck deformity, with painful pressure occurring under the head or stump of the proximal phalanx (Fig. 33). Stiffness may develop at the proximal interphalangeal joint, and it may create the functional effect of an arthrodesis.
Discussion
Flexor tendon transfers may have greatest application in those cases in which flexor stability has been lost, such as in patients with deranged metatarsophalangeal joint function. We believe that arthrodesis of the interphalangeal joints of the three middle toes is a preferred approach to converting the long flexor tension into an effective plantarflexor of the
metatarsophalangeal joint. Because arthrodesis of the fifth toe tends to create problems of shoe irritation, flexor tendon transfer may be well suited for assisting stabilization of that toe. It is sometimes difficult to determine the correct amount of tension under which to suture the flexor tendon. Too little tension can lead to poor toe purchase. Too much tension can lead to stiffness or reverse hammer toe deformity.
metatarsophalangeal joint. Because arthrodesis of the fifth toe tends to create problems of shoe irritation, flexor tendon transfer may be well suited for assisting stabilization of that toe. It is sometimes difficult to determine the correct amount of tension under which to suture the flexor tendon. Too little tension can lead to poor toe purchase. Too much tension can lead to stiffness or reverse hammer toe deformity.
Syndactyly
Syndactyly is the side-to-side anastomosis of two neighboring toes by resection dermoplasty. This is generally performed to help stabilize a flail toe or to eliminate an interdigital soft corn or heloma molle (45, 46, 47). This may be done as an isolated procedure or in combination with osseous procedures. The key conditions for successful correction are that the deforming forces be eliminated from the flail toe and that the adjacent toe be a stable functioning rectus digit. The dermoplasty itself is inadequate to neutralize deforming forces.
Procedure
A triangular or rectangular area of skin is marked on the side of the flail toe to be anastomosed to the adjacent toe. The base of the triangle is at the proximal web space, and the tip is distal. The dorsal arm of the skin resection is located slightly below the dorsal aspect of the web space. This approach allows a short fold between the toes, to enhance the cosmetic appearance. The distal tip of the triangle curls plantarly from the dorsum and dorsally from the plantar to meet, bisecting the toe. The toes are pressed together to form a mirror-image triangle on the adjacent toe. This mirror-image triangle can be marked in blood on the adjacent toe after the initial incision on the flail toe as an alternate marking system. This forms a trapezoid between the two toes. A controlled-depth incision is placed along the marked area to penetrate only the dermis. The dermis is undermined carefully so as not to disturb the underlying vasculature and is excised in toto. The plantar incision is then approximated with simple interrupted sutures that are initially not tied together but held with hemostats. Suturing is begun at the proximal edges of the wound and continues distally. The dorsal skin edges are likewise approximated. These sutures are also placed individually from proximal to distal and are initially not tied to allow for easy access to the skin for subsequent sutures. Once all the sutures are placed, the plantar sutures are tied starting from proximal to distal. Next the dorsal sutures are tied in order from proximal to distal. The suture ends are left slightly longer than normal to facilitate their removal (Fig. 34).
Aftercare
The toes are bandaged and splinted together for 10 to 14 days when the sutures can be removed. Little tension should exist between the toes if the flail toe has no deforming force remaining on it. If the two toes have any deforming forces on them, the toes can be splinted together for an additional 1 to 2 weeks.
Discussion
Whenever a syndactyly procedure is performed for a flail toe, all deforming forces on the adjacent toe should be neutralized before the procedure. The flail anastomosed toe will deform along with the adjacent toe if deforming forces remain present. In the case of a soft corn, syndactyly can readily eliminate the corn between the two toes. The results can be rewarding cosmetically if the deforming forces are neutralized in both toes. Often, additional osseous procedures for the toes are necessary concurrent with surgical syndactyly.
Osseous Procedures to Correct Digital Deformities
Historical Review
Post, in 1882, “excised distal extremities” of the proximal phalanges (48). This procedure is the predecessor of the present-day proximal interphalangeal joint arthroplasty, the most common procedure used for hammer toe surgery. In 1888, Terrier resected the base of the proximal phalanx in addition to performing head resection (49). Soule described the intentional arthrodesis of the proximal interphalangeal joint (50), and Higgs performed a fusion that consisted of using a spike-and-hole method after dovetailing the proximal phalanx after removal of the articular surface (51). Young remodeled the proximal phalanx into a truncated cone, removed the appropriate intramedullary bone from the middle phalanx, and locked them together (52). Taylor is credited with the first use of the K-wire for achieving intramedullary
fixation in hammer toe surgery (53). Selig bent the K-wire to stop proximal migration (54).
fixation in hammer toe surgery (53). Selig bent the K-wire to stop proximal migration (54).
Arthroplasty of Proximal Interphalangeal Joint
Indications
Arthroplasty of a proximal interphalangeal joint is often indicated in those digits with a flexible to semirigid deformity. The procedure shortens the toe and relaxes the soft tissues, and it lessens the tension of deforming extensor and flexor forces on the toe.
Procedure
The digit is approached through a linear or transverse incision at the level of the proximal interphalangeal joint (Fig. 35). Two semielliptic transverse incisions may be employed to remove redundant tissue. The incision is carried through the subcutaneous tissues to the level of the extensor digitorum longus tendon. The extensor tendon is freed from its soft tissue attachments to the dorsal aspect of the proximal phalanx. A curved mosquito hemostat can be used to retract the tendon. The medial and lateral collateral ligaments are then incised, and the head of the proximal phalanx is delivered into the wound. Soft tissue from the distal one-third of the proximal phalanx is removed. The head is resected at its appropriate level. The amount of bone resected depends on the amount required to relieve soft tissue tension while keeping the toe’s length appropriate to that of the adjacent toes. The remaining bone may be rasped smooth.
Occasionally, the extensor digitorum longus tendon is divided for access to the joint. If the tendon has been divided, it is resutured at closure. When a tendon has been retracted, it is repositioned on the dorsal aspect of the proximal phalanx and is sutured either medially or laterally to create stability. The wound is closed in a manner of preference.
Aftercare
Postoperative care includes supportive bandaging until skin and tendon have healed, usually for 3 to 6 weeks. When the procedure is performed on multiple toes, supportive bandaging may be continued for a longer interval and is of assistance in controlling edema.
Discussion
Arthroplasty of the proximal or distal interphalangeal joint is probably the most widely used procedure for correction of digital deformity. It is an excellent procedure to correct an isolated hammer toe, provided the cause of the deformity has been removed. If the deforming influence is still present, arthroplasty will leave a flexible joint that may subsequently redeform. Furthermore, arthroplasty of a toe relaxes both flexor tendons. The extensor tendons to that toe are also relaxed to some extent. However, because of the extensor hood attachments, the hood fibers would need to be released to gain the full benefit of the relaxation. This relaxation of the soft tissues is beneficial to that toe, but the tension is transferred to the other slips of the long extensor and long flexor tendons. In effect, loading of the tendons to the adjacent toes may occur, especially if too much bone is resected for the digital arthroplasty.
Other procedures to consider for neutralizing deforming forces include extensor hood release and proximal interphalangeal joint arthrodesis. If a transverse incision is used, there will be limited access to releasing the extensor hood. Tenotomy or Z-plasty tendon lengthening would best be performed through a separate incision proximal to the hood fibers if extensor contraction is not adequately released by bone resection in such a situation.
Interphalangeal Arthrodesis with Kirschner Wire Fixation
Interphalangeal arthrodesis with K-wire fixation consists of resecting the articular cartilage from both surfaces of the joint and fixing the bones in close apposition with a K-wire. This method converts the toe to a rigid lever on which the extensor and flexor digitorum longus tendons can function effectively. Arthrodesis is indicated in those patients in whom intrinsic muscle function has been compromised and digital and metatarsophalangeal joint stability are lacking. In fact, the principal indication is to provide a stable lever arm on which the long and short flexors can function to assist metatarsophalangeal joint stability. The procedure shortens the toe slightly because only cartilage is resected to expose subchondral cancellous bone. In fact, the straightening process may appear to lengthen the toe. The cartilage and bone that are resected do relax the soft tissues, and this again helps to remove some of the deforming forces. In some cases, an additional degree of shortening may be combined with the arthrodesis to provide better relaxation of soft tissue tension.
Procedure
The area is approached through a linear incision, but a transverse incision, or two transverse converging semielliptic incisions, may be used in special circumstances. The extensor digitorum longus tendon is identified and is generally divided into proximal and distal segments. This is done in a Z fashion if the tendon needs to be lengthened. The extensor tendon is then freed from its attachments to the proximal phalanx dorsally and is elevated from the proximal portion of the middle phalanx dorsally approximately 2 mm from the joint. The collateral ligaments are divided, and the joint is opened. The distal end of the proximal phalanx and the base of the middle phalanx are freed from soft tissue attachments. The cartilage is then resected, leaving exposed cancellous bone. At this point, extra bone can be removed from the proximal phalanx if shortening the digit is desired.
The K-wire is then driven distally through the middle and distal phalanges, and it exits through the distal end of the toe. The distal phalanx must be dorsiflexed so the nail bed and plate are not injured. The middle and proximal phalanges are then aligned. The K-wire tip is visually seated into the intramedullary canal of the proximal phalanx and is directed in retrograde fashion to the base of the bone. Stability is then checked. The wire can be placed in retrograde manner across the metatarsophalangeal joint while the joint is held in corrected or slightly overcorrected alignment.
The extensor digitorum longus tendon is sutured into corrected position, and any redundant tendon may be removed. The K-wire is bent 90 degrees at the distal end, to allow approximately one-fourth inch of space between skin and the distal aspect of the K-wire. This space accommodates occasional edema, which can create tension of pin against the skin. A K-wire cap can be used to protect the K-wire. The toe is then splinted with gauze as the bandage is applied.
Aftercare
The K-wire is usually left in place for 6 to 8 weeks, and ambulation is allowed to tolerance. If the wire crosses the metatarsophalangeal joint, it must be protected against bending force. At heel off, pressure is normally exerted by the ground against the tips of the toes. If wires are limited to the toes, the metatarsophalangeal joint will dorsiflex freely. If the wires cross the metatarsophalangeal joint, the bending force will disturb the pin-soft tissue interface and can contribute to pin tract infections or bending of the wire at the metatarsophalangeal joint. In addition, the repetitive force against the wire may cause metal fatigue that can result in breakage of the wire. The wire is usually protected against bending force for the entire 6 weeks by supportive splinting.
To accomplish this, the insole of the surgical shoe can be built up with felt or cork from heel to the web area. The toes are thus allowed to float over the end, to prevent contact with the shoe (Fig. 36). Supportive splinting is used with the bandaging, even when the shoe insole is built up, and it may prevent flexion stress with metatarsal loading.
To accomplish this, the insole of the surgical shoe can be built up with felt or cork from heel to the web area. The toes are thus allowed to float over the end, to prevent contact with the shoe (Fig. 36). Supportive splinting is used with the bandaging, even when the shoe insole is built up, and it may prevent flexion stress with metatarsal loading.
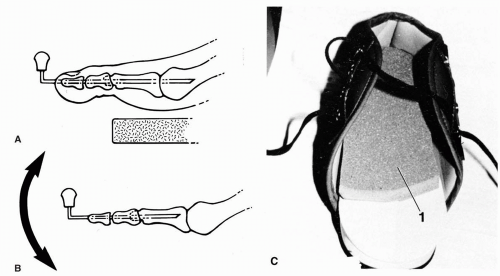 FIG. 36. A: A Kirschner wire (K-wire) maintains the arthrodesis of the proximal interphalangeal joint and is in place across metatarsophalangeal joint for at least the first 3 postoperative weeks. The K-wire is protected from bending forces by cork buildup in surgical shoe from heel to the sulcus beneath the toes. The end of the toe floats freely. A cast is an alternate method to prevent toe contact and to protect the metatarsophalangeal joint from bending forces. The distal end of wire is bent 90 degrees to prevent possible migration into tissues. A plastic cap on the end of the wire protects the wire from catching on clothes or sheets. B: After the first 3 to 3½ weeks, the K-wire can be withdrawn from across the metatarsophalangeal joint; the tip of wire again is bent to a right angle, and the cap is replaced. This permits exercise of metatarsophalangeal joint to minimize the chance of joint limitation. C: Postoperative shoe is illustrated with ¼-inch cork buildup (1) extending from the heel to the sulcus beneath the toes. |
Once the K-wires are removed, edema may be present for several weeks, especially where multiple wires cross metatarsophalangeal joints. This edema is managed with moist heat, compressive bandaging, range-of-motion exercises, and nonsteroidal antiinflammatory agents.
Elastic tape bandaging is most helpful. The edema and related soreness are usually short lived, lasting from 2 weeks to as long as 2 or 3 months.
Discussion
After arthrodesis, the digit usually can grasp the ground. Flexibility of the toe is reduced because all motion then occurs at the distal interphalangeal or the metatarsophalangeal joints. The decreased motion occasionally presents a problem in extremely active, athletically inclined patients. In this circumstance, delaying arthrodesing procedures or compromising by performing arthroplasty may be considered.
Peg-in-Hole Arthrodesis
Peg-in-hole arthrodesis has been used extensively for more than 50 years. One advantage of the procedure as compared with end-to-end arthrodesis is the snug fit created between the middle and proximal phalanges even without fixation. Generally, fixation is added with a K-wire, although its use is not essential.
Procedure
The approach for peg-in-hole arthrodesis is through a linear, transverse incision, or through two transverse, converging semielliptic incisions, depending on the degree of deformity (Fig. 37A). Generally, a linear incision is used when there is also deformity at the metatarsophalangeal joint. Use of two converging, transverse semielliptic incisions with removal of a wedge of dorsal skin is well suited to digits when the principal deformity is at the interphalangeal joint. If extensive deformity exists at both joints, it is helpful to combine
two converging, controlled-depth semielliptic incisions at the interphalangeal joint with a longitudinal incision that curves as it courses proximally over the metatarsophalangeal joint. The longitudinal incision in this latter instance provides surgical access, whereas the transverse, controlled-depth incisions simply remove redundant skin without penetrating the neurovascular structures.
two converging, controlled-depth semielliptic incisions at the interphalangeal joint with a longitudinal incision that curves as it courses proximally over the metatarsophalangeal joint. The longitudinal incision in this latter instance provides surgical access, whereas the transverse, controlled-depth incisions simply remove redundant skin without penetrating the neurovascular structures.
The longitudinal incision is deepened, and the extensor tendon is exposed. The tendon is severed transversely unless there is considerable dorsal contracture at the metatarsophalangeal joint. In the latter case, the tendon is separated by Z-plasty to accommodate the longer length required when the toe is straightened. The tendon ends are retracted, and the interphalangeal joint is opened. The head of the proximal phalanx and the distal one-third of the shaft are freed. The medial, lateral, and plantar condyles are resected from the phalangeal head (Fig. 37B). The distal cap of cartilage is also resected. The dorsal cortex is carefully protected, as is the cancellous center of the bone.
The intramedullary canal of the phalanx is opened with a hand-held K-wire before remodeling of the peg. Finding the canal after remodeling the peg can otherwise be difficult to impossible. The peg is then shaped to appropriate size and contour with a rotary bur, with care taken to preserve the dorsal cortex for structural stability. The base of the middle phalanx is drilled the length of the canal with a drill bit and is reamed with a ball bur to prepare to receive the peg. A trial seating is done to ensure the fitting (Fig. 37C).
A K-wire is drilled through the middle phalanx and out the end of the toe slightly plantar to the central area of the medullary canal to accommodate the dorsal cortex of the proximal phalanx. The toe is aligned, and the proximal end of the wire is introduced into the previously established intramedullary canal in the proximal phalanx. The wire is moved in retrograde fashion into the proximal phalanx. If required, it is drilled across the metatarsophalangeal joint and into the distal one-third of the metatarsal while the joint is held appropriately reduced.
The peg is seated securely, the wire is bent 90 degrees at the end of the toe, and a wire cap is placed on the tip. If the extensor tendon contracture through the hood fibers remains a deforming force, extensor hood recession may be required. The extensor tendon is repaired, and the subcutaneous tissue and skin are closed in layers.
Aftercare
Postoperative care is much the same as for end-to-end interphalangeal joint arthrodesis, except osseous stability is greater and thus permits earlier removal of the wires. The K-wires must be protected at the tip, and if the wires cross the metatarsophalangeal joint, they must also be protected against bending force. Postoperative supportive bandaging is usually continued for 6 weeks until the K-wires are removed. In actual practice, the wires may be removed by the third postoperative week when the peg is well seated and when the toes can be adequately protected. A digital retainer may be used after removal of multiple wires and helps to control postoperative edema.
Range-of-motion exercises for the metatarsophalangeal joints and moist heat are helpful once bandaging is removed. Passive range-of-motion exercises may also be helpful.
Discussion
An advantage of peg-in-hole arthrodesis is that it shortens the toe, relaxes soft tissues, and allows for ease of correction. When the toe is already short, performing an end-to-end arthrodesis may be preferred. The procedure has the added advantage of providing more bone-to-bone contact and has a higher union rate than does the end-to-end fusion. No fixation is actually required, especially when a cast is used and a snug fit is present between the proximal and middle phalanges. Disadvantages include a general shortening of the toe (if the toe is already short). The possibility of dorsal cortical fracture of the proximal phalanx always looms, and this could create instability between the proximal and middle phalanges. This is the one reason that a K-wire is usually used. Another disadvantage is that the procedure is technically more difficult when compared with the end-to-end arthrodesis.
When performing an arthrodesis of the fourth toe on a young patient who enjoys fashionable or snug shoes, it is wise to shorten the peg just enough so the end of the fourth toe will be sheltered by an imaginary line drawn between the ends of the third and fifth toes. The toe is thus protected from pressure against the curve of the shoe. Rigid toes do not tolerate shoe pressures well, and this is the principal reason that arthrodesis is rarely, if ever, performed on the fifth toe. This excellent procedure provides a stable toe and usually results in greatly improved metatarsophalangeal joint function, provided adequate soft tissue releases have been performed in conjunction with the procedure.
Digital Arthrodesis Using Internal Pins
Fixing a digital arthrodesis site by means of a K-wire protruding out the end of the toe poses certain problems. Exiting the skin for a protracted period exposes the site to potential infection, pin trauma, pin bending, and accidental removal, although the actual incidence of such occurrences is low. In addition, the patient must keep the wound dry for up to 6 weeks. Finally, the anticipation of pin removal can generate considerable anxiety, and the extraction itself may be painful. All these factors can be frustrating to the patient and challenging to the surgeon. In response to these considerations, internally placed pins have been used to provide digital fixation.
Two types of pins have been implanted across digital arthrodesis sites for internal fixation. Patton used a 1.3-mm para-dioxanone absorbable pin that dissolved by hydrolysis approximately 6 months after insertion (55). Miller implanted a 2.4-mm diameter pin fashioned out of cortical allograft bone (56). This bone pin, placed in the intramedullary canals across the arthrodesis site, is actually incorporated into the local bone to form a framework for bone fusion. Small screws have also been placed internally for proximal interphalangeal joint fusion; the main disadvantage is that, for insertion, they must pass through or across the distal interphalangeal joint.
Procedure
Once the proximal interphalangeal joint is exposed, the opposing articular surfaces are resected, and both intramedullary canals are drilled with a 2.4-mm smooth K-wire. The two channels are measured, and the results are totaled to determine the appropriate length for the allograft bone pin. The pin is first placed into the proximal phalanx using a plunger, and then the middle phalanx and distal end of the toe are manipulated onto the protruding end of the pin to complete the fixation. One main advantage of the bone allograft pin over the absorbable pin is that the former pin is visible on radiographs, a feature allowing a periodic assessment of the incorporation arthrodesis (Fig. 38).
Discussion
Internal fixation pins function as rigid intramedullary rods. Although both types of pins provide rigidity and resist shearing forces, the absorbable pins lack strength related to bending and compressive forces, whereas the processes for preparing the bone allograft pins tend to reduce their torsional and bending strength. These modest limitations have not affected the success of digital corrections with either device.
In contrast to the polymeric pins that are hydrolysed for linear resorption and bone replacement without incorporation, the bone pins act as a lattice on which new bone can form by osteoconduction. Some bone morphogenic protein
is preserved in the bone allograft pins so they possess osteoinduction capabilities as well. The result is total incorporation and the ability to bridge gaps. Besides their low antigenicity, these processed bone bins are associated with a negligible risk of infection calculated at 1:1.6 × 106. There have been no reported diseases to date as a result of the implantation of bone allograft pins.
is preserved in the bone allograft pins so they possess osteoinduction capabilities as well. The result is total incorporation and the ability to bridge gaps. Besides their low antigenicity, these processed bone bins are associated with a negligible risk of infection calculated at 1:1.6 × 106. There have been no reported diseases to date as a result of the implantation of bone allograft pins.
One disadvantage of internal pins for toe surgery is the lack of compression for the acceleration of bone healing. As rigid devices, they can fracture, but this has not proven to be a problem. Another disadvantage is that the pins cannot cross the metatarsophalangeal joint when it is necessary to maintain the reduction of a subluxed or dislocated articulation. This problem can usually be overcome with the addition of a flexor digitorum longus tendon transfer.
Resection of the Base of the Proximal Phalanx
Resection of the base of the proximal phalanx was first described by Kreuz in 1923 for correcting dislocation of the
metatarsophalangeal joint (57). However, the procedure has been used for the correction of hammer toe deformities. The operation is intended to increase motion at the metatarsophalangeal joint.
metatarsophalangeal joint (57). However, the procedure has been used for the correction of hammer toe deformities. The operation is intended to increase motion at the metatarsophalangeal joint.
Performing resection of the proximal phalangeal base by itself is contrary to all logic in trying to maintain digital stability. Loss of the digits’ intrinsic muscle function is obvious because their attachments to the proximal phalanx are sacrificed. Instability is created, and this allows the digit to retract dorsally, often creating plantar protrusion of the metatarsal head and causing a plantar keratosis. The toe floats or dangles and cannot act as a lever for weight transfer. The procedure is justified in patients with bone tumors and in those with osteomyelitis involving the base of the proximal phalanx. It is commonly used as an adjunct procedure in severe rheumatoid foot surgery and in patients with derangement of the metatarsophalangeal joint.
When proximal phalangeal base resection is performed, Kelikian recommends constructing a web between the involved digit and the adjacent toe to enhance the grasping effects of the combined toes and thus to decrease instability and the tendency to shorten (28). The combined action of the long flexors is at least partially transferred to the metatarsophalangeal joint where flexion is indispensable. However, this is an ineffective way to stabilize the toe. Conklin and Smith found that when they included an extensor tenotomy, the satisfaction with the procedure increased (58). They also found that those cases in patients with transverse plane deviation, metatarsalgia, and metatarsophalangeal subluxation or dislocation had lower rates of success. In 1979, Jim Ganley indicated that resection of the base of the proximal phalanx worked well for him in digital surgery (59). He showed some excellent cases in which malalignment and poor toe purchase did not occur. The reason for the good results achieved were believed to be derived from the transfer of the extensor digitorum longus tendon into the corresponding metatarsal. The extensor digitorum brevis tendon was preserved to allow some continued dorsiflexion force.
Ganley seemed to be using the principle of tendon balancing similar to that seen in the Keller arthroplasty for the first metatarsophalangeal joint. In the Keller bunionectomy, Ganley had advocated lengthening the extensor hallucis longus tendon (60). McGlamry recommended attaching the flexor hallucis longus or brevis to the stump of the proximal phalanx (61). These tendon balancing procedures have allowed better digital function for the hallux along with the good pain relief of the traditional joint-destructive procedure.
Although we do not recommend the base resection of the proximal phalanx as a first-line procedure for correcting hammer toes, it can be used effectively when the patient has arthrosis or degeneration at the lesser metatarsal joints or if there is difficulty in relocating severe dorsal or transverse plane contracture at the metatarsophalangeal joint. We recommend Ganley’s extensor digitorum longus transfer to the metatarsal and McGlamry’s flexor digitorum longus transfer to the stump of the proximal phalanx along with the traditional base resection and capsulorrhaphy.
Procedure
A curvilinear skin incision is placed over the base of the involved digit and metatarsophalangeal joint. The extensor digitorum longus and brevis tendons are identified. The extensor hood is incised, and the extensor apparatus is reflected. The extensor digitorum longus tendon is divided transversely at the metatarsal neck and is retracted. The extensor digitorum brevis is preserved. The periosteum and capsule are reflected in a linear fashion, to expose the proximal one-third of the proximal phalanx. The proximal phalangeal base is resected, and the remaining bone may be rasped smoothed. A drill hole is placed centrally through the plantar cortex of the stump of the proximal phalanx. The metatarsal head may be freed of any restrictive soft tissue attachments with the aid of a McGlamry elevator. A linear incision is made through the plantar capsule, and the flexor digitorum longus and brevis tendons are identified. The flexor digitorum longus is isolated and is attached by the drill hole to the plantar stump of the proximal phalanx. The tendon is secured under tension with the toe held in a slightly overcorrected position. The extensor digitorum longus is secured to the metatarsal neck with the foot held at right angles to the leg. The periosteum is closed over the tendon and is further secured to the tendon. If desired, one may “pursestring” the capsule into the void from side to side. A K-wire may be driven out through the tip of the toe from the stump of the proximal phalanx and may be moved in retrograde fashion back across the metatarsophalangeal joint. The wire should hold the toe in a mildly plantarflexed attitude. The extensor hood apparatus is relocated with the extensor digitorum brevis, and the wound is closed in layers. The range of motion is evaluated intraoperatively to ensure adequate motion if no K-wire is used (Fig. 39).
Aftercare
A K-wire may be used for a sufficient period of time to allow fibrous tissue organization to help stabilize the digit. The wire may also be used to anchor the pursestring capsule in the joint space during healing.
Discussion
When conservative therapy and joint preservation techniques are inadequate, the tendon balancing technique described in conjunction with base resection has proven successful in the surgical treatment of painful arthrosis of the lesser metatarsophalangeal joints. The advantages to this procedure are that it preserves the weight-bearing metatarsal head, it neutralizes the dynamic forces across the metatarsophalangeal joint, it helps to replace the intrinsic forces at least in the sagittal plane, and it stabilizes the digit. Like most other joint-destructive procedures of the lesser metatarsophalangeal joints, the procedure also eliminates painful motion. It can be combined with arthrodesis or arthroplasty of the proximal interphalangeal joint or with implant arthroplasty of the metatarsophalangeal joint. Neutralization of transverse plane deformities is often not necessary because the interossei on both sides of the metatarsophalangeal joint have been released with the resection of the base of the proximal phalanx. However, this procedure does not stabilize the metatarsophalangeal joint in the transverse plane. Additional techniques may be necessary to maintain stability in the transverse plane. The key to the successful positioning of the toe is the tendon balancing.
Bone Grafting in Digital Repair
In most cases of digital surgery, bone shortening techniques are beneficial to help release soft tissue contractures. However, some patients may have a flail toe as a result of overaggressive bone resection with previous surgery. In this circumstance, lengthening the toe may be desirable to reestablish function (62). Bone graft arthrodesis and implant
arthroplasty are options to achieve this result. Syndactyly is an alternate procedure, but this does not have the benefit of restoring length and function to the toe.
arthroplasty are options to achieve this result. Syndactyly is an alternate procedure, but this does not have the benefit of restoring length and function to the toe.
A flail toe can be defined as one that lacks stability and structural integrity. Often, the patient complains of catching the toe on stockings or shoes. The flail toe presents a functional, cosmetic, and sometimes symptomatic problem (Fig. 40A). Mahan described a bone graft stabilization technique for a flail toe using cortical cancellous calcaneal graft that has proven successful (63).
Procedure
A linear incision is made over the digit (usually encompassing a previous scar if present). The extensor tendon is lengthened in a Z-plasty technique. The distal portion of the proximal phalanx and the base of the intermediate phalanx are resected to raw bleeding bone, with removal of any sclerotic tissue. Any plantar scarring that would restrict lengthening of the digit is released.
A corticocancellous autograft is procured from the dorsolateral aspect of the calcaneus or other suitable area. The graft is trimmed to the necessary length and width and is predrilled with a 0.035-inch K-wire. A 0.045-inch K-wire is inserted in retrograde fashion through the intermediate and distal phalanges out the end of the toe. The graft is placed between the proximal and intermediate phalanges so the cortical surface is on the dorsal side of the toe for stability. The K-wire is then driven from distal to proximal through the bone graft, the proximal phalanx, and into the corresponding metatarsal (Fig. 40B). The wound is closed in layers. The vascular status to the digit is checked to ensure that lengthening has not compromised the circulation to the toe.
Aftercare
A below-knee non-weight-bearing cast is used. When consolidation of the graft is noted (usually around 8 weeks postoperatively), the K-wire is removed. The cast is continued for an additional 2 weeks, but partial weight bearing may be allowed. A surgical shoe is used for an additional 3 weeks. If good consolidation and stability are noted along the graft at 3 months, then the patient is allowed into a flexible shoe.
Discussion
Bone grafting in digital surgery is not a common procedure. Fortunately, the flail toe is becoming less common. Postoperative disability, the small graft-host interface, the additional surgical procedure required to obtain the donor graft, and the potential risks including failure of the graft and vascular compromise must all be weighed in the preoperative decision. Implant arthroplasty, syndactyly, and amputation can be considered as alternative techniques. However, the bone grafting technique can be successful in restoring structural and functional stability to the flail toe (Fig. 40C).
Intraoperative Stepwise Approach to Digital Surgery
Hammer toe surgery is best approached in a stepwise manner. The degree of fixed deformity is determined by the push-up test and by range-of-motion examination of the involved joints. A flexible deformity allows the digit to assume a rectus position when the foot is loaded. Semirigid or rigid deformities are evidenced by continued flexion of the interphalangeal joint and extended metatarsophalangeal joints when the forefoot is loaded. The surgeon should have a good understanding of digital pathomechanics. Clinical judgment should allow for presurgical planning regarding whether an arthroplasty procedure will be adequate or whether soft tissue releases combined with digital stabilization arthrodesis will be necessary. However, adequate anatomic relocation of the digit and release of deforming soft tissue structures should be performed intraoperatively.
Resecting the Head of the Proximal Phalanx (Post Procedure)
Resecting the head of the proximal phalanx is most commonly performed to reduce the bony prominence under painful corns on the digit (48) (Fig. 41). This procedure also releases some of the deforming force of the flexor digitorum longus and brevis by shortening the origin to insertion of these tendons. However, the extensor sling, which provides the primary pull of the extensor tendons, is proximal to the resected bone. Therefore, simple head resection of the proximal phalanx may be inadequate to release the contracture of the extensors. When the toe returns to anatomic alignment after loading of the metatarsal (push-up test), the extensor contraction is not a significant deterrent to correction. In the event the joint does not realign and the proximal phalangeal stump remains extended, an additional surgical step is necessary.
Extensor Hood Recession
Distal relaxation is created in the extensor tendons by relatively lengthening the origin to the insertion with the resection of the head of the proximal phalanx. This slack can be transmitted proximally by releasing the extensor hood fibers on either side of the extensor digitorum longus and brevis tendons and at the metatarsophalangeal joint. Extensor hood recession is performed by placing the tendon on stretch distally and severing the hood fibers medially and laterally at their attachments to the joint capsule and the proximal phalangeal sling. The metatarsal ray is then loaded by the push-up test. If the metatarsophalangeal joint completely realigns, adequate correction has been obtained. If the proximal phalangeal stump stays in an extended position, an additional surgical step will be needed. An alternative procedure to the hood recession is lengthening or tenotomy of the extensor digitorum longus tendon. However, this must be accomplished proximal to the hood fibers to be effective.
Extensor Tenotomy or Lengthening
Lengthening of the extensor digitorum longus tendon can be achieved by tenotomy or a Z-plasty lengthening. Caution should be used if all the extensors are not lengthened. All four of the tendons originate from the same muscle. Releasing the tension on any one tendon segment will apply additional load on the others. This may result in significant loading force on these adjacent toes and may cause pathologic contracture. The tendons can be lengthened in a Z-plasty technique through a single longitudinal incision over the metatarsal shafts proximal to the extensor hoods. However, in the stepwise approach when the hood recession has been done, the Z-plasty lengthening can be accomplished at the digital or metatarsophalangeal joint area. The long extensor tendon is split by open Z-plasty, and the ends are retracted from the wound. The foot is again loaded, and the proximal phalangeal alignment is evaluated. If the proximal phalanx stays in an extended position when the ray is loaded, additional surgical treatment will be needed.
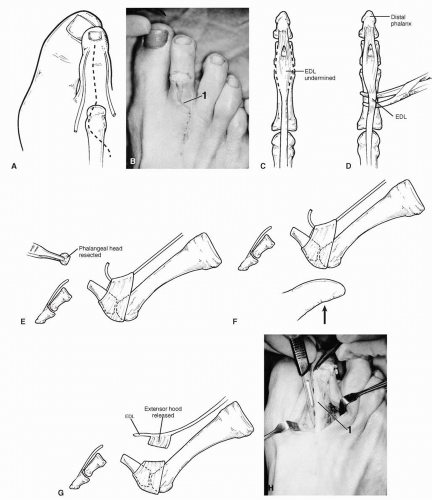 FIG. 41. Stepwise approach to hammer toe repair. A: A curvilinear incision is placed over the metatarsophalangeal joint to minimize the effects of contracture during healing. B: Transverse converging semielliptic controlled-depth incisions may be combined with a curvilinear incision (1). Removal of the transverse ellipse helps to eliminate redundant tissue and assists in holding the digit in rectus position (if necessary). C: Broken lines indicate the section of the extensor digitorum longus (EDL) tendon to undermine from the proximal and middle phalanges. D: A curved hemostat is used to retract the extensor tendon. E: The proximal phalangeal head is resected. F: The push-up test loads the metatarsal ray. If the metatarsophalangeal joint does not realign and the proximal phalanx remains extended, an extensor hood recession will be required. G: An extensor hood recession is performed. H: The extensor tendon is distracted distally, and the hood fibers are released medially and laterally at their attachment to the proximal phalanx and joint capsule. 1, EDL. I: A repeat push-up test revealed that the proximal phalanx remained extended, and the extensor digitorum longus tendon is divided in an open Z-plasty technique. This can be done at this level because the extensor hood has already been released. J,K: If the proximal phalanx remains extended with a repeat push-up test, this indicates dorsal capsular contracture. As the proximal phalanx is distally distracted, a dorsal, medial, and lateral capsulotomy is performed. L: A repeat push-up test may reveal that the digit and the metatarsophalangeal joint are in rectus alignment. M: Arrow shows the fibrosis of capsule to the inferoproximal aspect of the metatarsal head. This capsulodesis prevents realignment of toe and metatarsophalangeal joint in response to the push-up test. N: With the metatarsophalangeal joint flexed 90 degrees, an 11- or 13-mm metatarsal elevator is used to release the flexor capsulodesis from the proximal plantar aspect of the metatarsal head and neck. O: The head of the proximal phalanx is shaped to form a peg (2), and the middle phalanx has been reamed to accept a peg (1). P: The arthrodesis site is reduced. Extreme care must be taken to preserve the dorsal cortex of the proximal phalanx. 1, Arthrodesis of the proximal interphalangeal joint. Q: The arthrodesis and metatarsophalangeal joint alignment are maintained with a Kirschner wire (1). Note the slight overcorrection of the metatarsophalangeal joint, with the proximal phalanx resting abducted and plantarflexed on the second metatarsal head (2). |
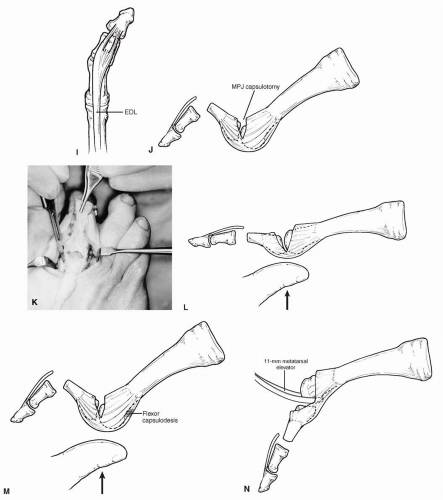 FIG. 41. Continued.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|