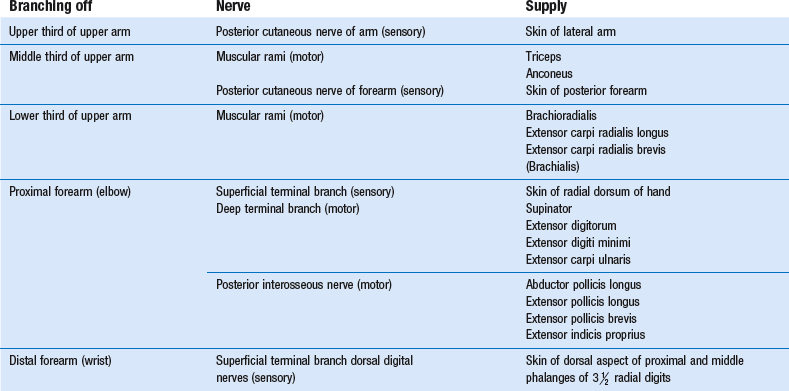
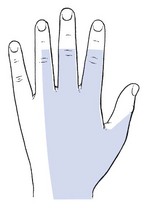
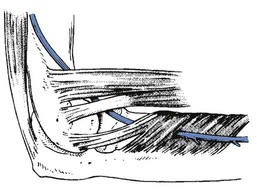
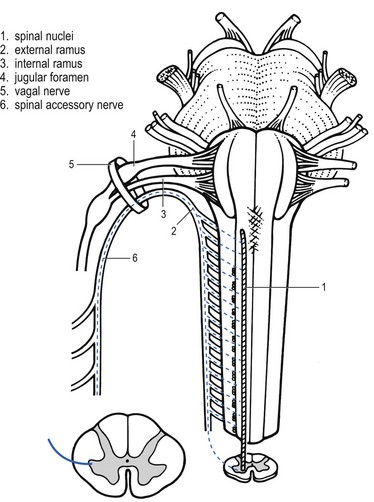
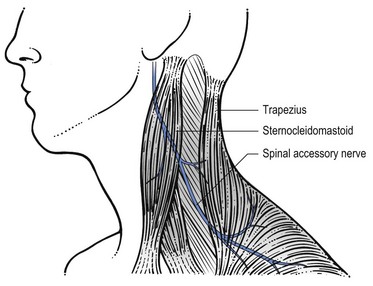
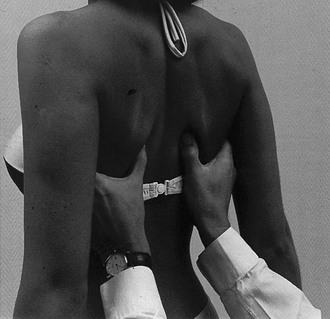
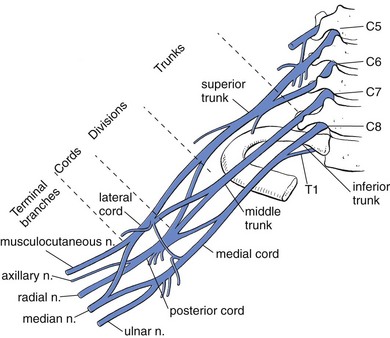
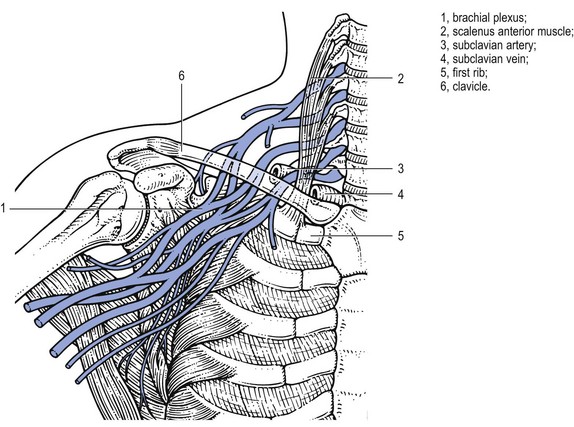
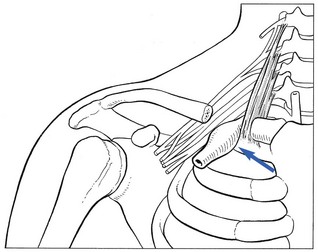
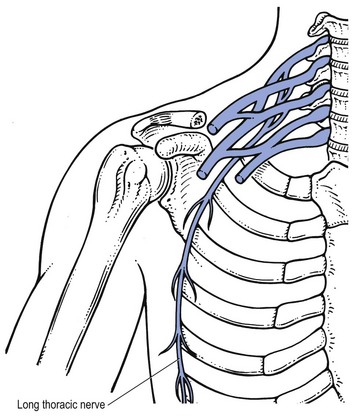
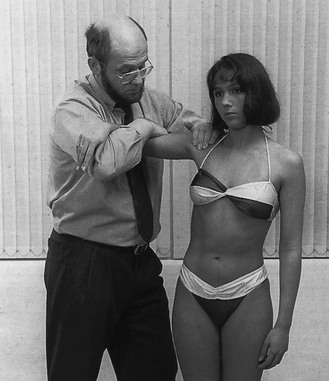
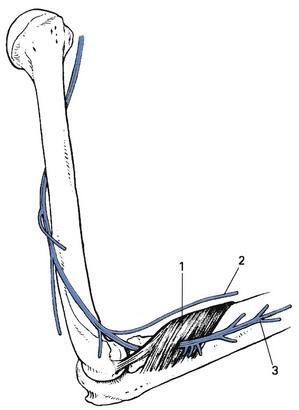
Disorders of the spinal accessory nerve Disorders of the brachial plexus Disorders of the long thoracic nerve Disorders of the suprascapular nerve Disorders of the axillary nerve Lesions at the proximal and middle part of the upper arm Lesions at the distal part of the upper arm Lesions at the upper part of the forearm Lesions at the lower part of the arm and around the elbow Lesions at the forearm: anterior interosseus nerve Entrapment phenomena occur typically at four different sites giving rise to four different mechanisms (see Chapter 2): • Pressure on a distal nerve causes mainly analgesia as well as some paraesthesia in the territory of the nerve. • When a nerve trunk or plexus becomes compressed, the release phenomenon – paraesthesia when the pressure ceases – is found. • Nerve root compression is characterized by pain and paraesthesia, felt in the corresponding dermatome, and often followed by sensory and motor deficit in the same segment. • Pressure on the cervical spinal cord is painless. An early symptom is paraesthesia with multisegmental distribution. When the compression becomes more severe, numbness, incoordination, spasticity and hyperreflexia may occur. Disorders of the spinal cord and nerve roots are discussed in Chapters 2 and 8. Both parts accompany the glossopharyngeal (IX) and vagus (X) nerves in their exit through the jugular foramen. The fibres originating from the nucleus ambiguus then join the vagus nerve and the other fibres – the real spinal accessory nerve – descend towards the muscles they innervate (Fig. 1). The spinal accessory nerve is a pure motor nerve and innervates the sternocleidomastoid and the trapezius muscles (Fig. 2). A lesion of the spinal accessory nerve may be either idiopathic or result from a compression along its course. Idiopathic spinal accessory neuropathy may occur in isolation or in combination with a disorder of other nerves (glossopharyngeal, vagus, long thoracic or dorsal scapular).1 Mechanical lesions of the spinal accessory nerve can occur at different levels: • Within the skull where the cause is usually tumourous.2,3 This is uncommon. • At the level of the exit through the jugular foramen where again, rarely, metastases or schwannomas may affect the nerve.4,5 • At the level of the neck where iatrogenic trauma, for example biopsy of lymph nodes in the posterior triangle, forms the commonest cause of isolated paralysis.6–12 Injury rates from these procedures are reportedly 3–8%.13,14 External traumas may also damage the nerve. The patient initially complains of intermittent pain in the shoulder girdle area, which soon may become permanent.15,16 At the same time, the arm starts to feel weak and heavy, which leads to some functional loss.17 Exceptionally, pain is absent. Pain normally lasts for about 3 weeks, after which it disappears spontaneously. Inspection elicits an asymmetrical neckline with drooping of the effected shoulder. This may be accompanied with lateral displacement and winging of the scapula.18 Typically, winging is minimal and is accentuated during arm elevation, with the scapula moving upwards with the superior angle more lateral to the midline than the inferior angle. Limitation of active elevation of the arm is a consistent finding, and in one series of patients, the majority could only elevate to 80–90°.19 Passive neck, scapular and arm movements do not influence the pain. Resisted elevation of the shoulder girdle is weak. Resisted external rotation of the arm makes the scapula more prominent medially.20 In severe cases the trapezius muscle may be wasted. The diagnosis is confirmed by asking the patient to adduct both scapulae while the therapist applies counterpressure at the medial border of the inferior scapular angle (Fig. 3). In neuritis of the accessory nerve, the scapula on the affected side can easily be pushed away at the side. Spontaneous cure of motor function of the trapezius is the rule and usually takes about 4–8 months.21,22 If inadequate functional recovery is seen after a year, additional conservative treatment is unlikely to be beneficial and surgery is indicated. In a recent review of the literature, authors have reported good or excellent results in approximately two-thirds of patients treated with nerve surgery.23 From the infraclavicular part of the plexus the following nerves originate: the medial cutaneous nerve of the arm (supplying the anteromedial and posteromedial part of the arm); and the medial cutaneous nerve of the forearm (its anterior ramus supplying the anteromedial aspect of the forearm, and its cubital ramus supplying the posteromedial aspect of the forearm) branches of the medial cord of the brachial plexus (Fig. 4). The brachial plexus lies quite superficially within a very mobile shoulder girdle and is closely related to the different bony structures of neck, shoulder girdle, shoulder and thorax. This situation makes it very vulnerable. Traumatic disorders are therefore one of the commonest causes of brachial plexus dysfunction. As the result of traction injuries (e.g. motorcycle accidents), compression by dislocated (e.g. shoulder luxation24,25) or fractured bones (e.g. fracture of the clavicle26) or by haematomas, and intraoperative or birth injuries, larger or smaller parts of the plexus may become damaged, leading to total or partial syndromes.27 This is called Erb–Duchenne’s paralysis and is defined as a palsy of C5 and C6 and sometimes of C7. There is a motor deficit of the muscles innervated by the nerves originating from these fibres and possibly a sensory deficit in the C5 and C6 dermatomes (lateral and anterior aspects of arm and forearm and radial aspect of hand and fingers) (Table 1). Table 1 Affected nerves and muscles in a palsy of the upper part of the brachial plexus The superior pulmonary sulcus tumour (Pancoast) typically invades the lower trunk of the plexus as well as the sympathetic ganglia at the base of the neck.28 A lower brachial plexus dysfunction is then accompanied by Horner’s syndrome (see p. 3 of online chapter Disorders of the thoracic cage and abdomen). Thoracic outlet syndrome (TOS) is a vague term, only suggesting the presence of a disorder within the area of the thoracic outlet. Although it is generally accepted that the aetiology is compression of the plexus and vascular bundle in the thoracic outlet, different opinions exist about the pathogenesis. This is expressed in the various names that have been given to the syndrome (see Box 1).29 The consequence of disagreement on the aetiology is that numerous methods of treatment are advocated. The thoracic outlet is the space bounded by the upper part of the sternum, clavicle, first rib and the first thoracic vertebra.30 Towards the centre, it is limited by the trachea and oesophagus. It forms the communicating area at the base of the neck for the passage of blood vessels and nerves from mediastinum and neck to the axilla and into which the dome of the pleura rises upward.31 The vagus, phrenic nerves, sympathetic trunk and thoracic duct also pass through the same openings. The first rib has a flat upper surface. In its anterior portion there are two grooves, which are separated by the tubercle at which the anterior scalene muscle inserts. The more medial groove accommodates the subclavian vein. Behind the muscle, in the posterior groove, both subclavian artery and brachial plexus are found (Fig. 5). According to Cyriax, the syndrome is the outcome of a compression of the most medial branches of the brachial plexus, usually occurring between the clavicle and first rib, seldom as the result of a cervical rib. The compression is usually bilateral, intermittent or continuous and may or may not involve the subclavian artery and vein.32 It gives rise to a set of neurovascular symptoms, which are rarely present all together. Symptoms of neurological disturbances are usually found but sometimes only features of vascular compression.33 The brachial plexus is involved in 98% of cases, the subclavian vein in 1.5%, and the artery in 0.5%.34,35 Cyriax recognized two main groups of thoracic outlet syndromes based on anatomical and clinical grounds: the cervical rib syndrome and the first rib syndrome. We prefer to substitute for these terms. We make a distinction between the thoracic outlet syndrome caused by anatomical changes and that from postural factors. This approaches the growing agreement about the use of four terms to indicate the presence of the thoracic outlet syndrome;36,37 true neurologic, arterial and venous TOS – those syndromes that result from compression by a cervical rib (anatomical variety); and non-specific neurologic TOS38,39 – the postural variety. This is caused by structural changes – the presence of a bony cervical rib or a band of fibrous tissue which is found in 0.5% of a normal population. Only 5% of them will ever suffer from a thoracic outlet syndrome.40 In a fibrous band, the corresponding transverse process of C7 is larger than usual – a rudimentary cervical rib. A cervical rib sometimes gives rise to a palpable mass at the base of the neck. Interference with the neurovascular structures usually begins at between 20 and 30 years of age and is thereafter continuous. Structural change and clinical features are frequently bilateral, although often more pronounced at one side.41 The symptoms are the result of compression of both neurological and vascular structures. The compression can be venous and/or arterial. Compression of the subclavian artery (Fig. 6) results in coldness, pallor and easy tiredness of the hand.42 Especially after the arm has been hanging down for a while, the hand may turn white and cold over a period of hours. A diminished pulse may be found. In more severe cases, chronic compressive stenosis of the artery may give rise to claudication of the upper extremity. It may further lead to a poststenotic dilation, sometimes to the formation of an aneurysm. Atheromata arising from these aneurysms or from chronic compression injury of the artery can result in peripheral embolization, which may lead to irreversible damage to the hand and even to the entire arm.34,43–45 There are two types, depending on the clinical features. This is unusual, but the diagnosis is important although difficult to make. Frequently the patient is admitted to the hospital suspected of having had a heart attack.49 It affects the middle aged or elderly, more frequently females. It sometimes occurs in pregnancy. The onset is with pins and needles in the hand and fingers, mainly at night and usually after 2–3 hours of sleep. The process is often bilateral, although worse on one side. Paraesthesia may be felt in all digits but may predominate in the median or ulnar distribution. It wakes the patient, who finds that she has to sit up or walk around for a short period of time, rubbing and moving the hands and fingers, to make the symptoms go. The symptoms disappear after a few minutes, allowing sleep to be continued, although recurrence may take place in the early morning hours. The more physical activity during the preceding day, the worse the symptoms at night.50 In periods of rest or sickness, when the patient lies down for the whole day, no pins and needles are felt. Some patients also experience symptoms during the day, on activities such as knitting, holding a newspaper in front of the eyes or bicycling, all of which require some degree of shoulder elevation. Augmenting the pressure by carrying a heavy object may exceptionally provoke the symptoms as well, but normally only to a mild degree. Cyriax explained this pattern as being the consequence of a diminishing tone in the shoulder muscles, starting in middle age. As a result, the shoulder girdle droops down during the day, resulting in compression of the most medial trunks of the brachial plexus, between the first rib and clavicle. Compression occurs during the day but the symptoms come on mainly at night after the pressure on the nerve has disappeared. He called this the ‘release phenomenon’ (see p. 26). The process seldom leads to damage of the nerve parenchyma with subsequent muscular atrophy because the brachial plexus can recover every night when the pressure is released. The diagnosis is based mainly on the typical history, all passive movements of neck, shoulder and shoulder girdle being normal.51 The resisted movements are of normal strength and painless, except for C8 or T1 structures in the hand, which may be weakened when the compression is the outcome of a cervical rib. This type of characteristic history should always be followed up with the following additional tests. The patient sits in a comfortable position and is asked to shrug the shoulders for about 3 minutes (Fig. 7). This causes maximum release of pressure and therefore may bring on the pins and needles and abolish vascular symptoms if present. However, this test is not always positive when thoracic outlet syndrome is present; in this case, release of pressure must be tried in different positions, either fully raising the arms above the head and maintaining this position for 3 minutes (Fig. 8) or lying supine with both hands on the head for the same length of time (Fig. 9). Other tests for thoracic outlet syndrome have been advocated classically. Although we regard them as less specific and reliable, they are mentioned here for completeness. Adson’s test,52 the modified Adson’s test and Roos’ test (elevated arm stress test)53 are regarded by some as totally unreliable, because about 50–60% of the normal population have positive findings.54,55 The patient abducts the arms to 90°, then opens and closes the hands slowly for 3 minutes. Those who are unable to keep their arms and hands elevated because of pins and needles are regarded as suffering from thoracic outlet syndrome. However, in carpal tunnel syndrome, active flexion of the fingers can bring on the pins and needles, and therefore this test does not differentiate between these two disorders (Fig. 10). Electromyography (EMG) and conduction studies are of little value, for two reasons.56,57 First, the range is quite variable in normal patients. Second, because the stimulating electrode can not be placed proximal to the level of the compression, the compound action potential which is measured does not cross the site of the nerve compression. But EMG is helpful for differential diagnosis, in excluding nerve compression at other levels, such as ulnar nerve impingement at the elbow or carpal tunnel syndrome. A radiograph of both the cervical spine and thorax can help to detect a cervical rib, a hypertrophic transverse process of C7 (suggesting a fibrous band) or the formation of a clavicular callus.58 It also helps to exclude a Pancoast’s tumour. A CT scan may demonstrate an abnormal fibrous band. A lesion of the ulnar nerve provokes pins and needles felt only in the fifth finger and at the ulnar half of the fourth. In compression at the cubital tunnel, some local pain around the elbow may also occur (see p. e138 of this chapter). Pins and needles may be felt at the dorsal aspect of the lower arm, and of the Compression of the median nerve in the carpal tunnel causes paraesthesia felt on the palmar aspect of the thumb, index and middle finger and the radial half of the ring finger. Carpal tunnel tests may be positive, although in 50% they remain negative (see p. e155 of this chapter). The coexistence of pins and needles and Pancoast’s tumour implies invasion of the brachial plexus, which may give rise to a palsy of the interosseous muscles at the hand. Very often a palsy of the recurrent nerve, causing hoarseness, is also present. Clinical inspection of the face may reveal Horner’s syndrome (ptosis of the upper eyelid, enophthalmia and myosis; see p. 3 of online chapter Disorders of the thoracic cage and abdomen). Because of the lack of consensus about the aetiology of this syndrome, various forms of treatment have been described (see Box 2). In the light of the mechanism that we consider responsible for the symptoms, the following approach is proposed. For some weeks, the following daily exercise must be done in the evening. Seated in an armchair, elbows resting on the arms, both shoulders are kept shrugged passively (Fig. 11). This brings the pins and needles on after a while but the position is maintained, even if symptoms become more severe. Once they diminish and disappear spontaneously, usually in half an hour, the shoulders are let down. An orthosis designed to elevate the shoulder has been described. It has good results in 77% of patients.59 In cases refractory to conservative treatment, resection of the normal first rib can be performed.60–63 However, this is major surgery and not always successful in relieving symptoms. This approach also carries potential dangers, because of the close relationship to the brachial plexus and subclavian/axillary artery.64,65 Table 2 provides a summary and differential diagnosis of the anatomical and postural varieties of thoracic outlet syndrome. Table 2 Differential diagnosis and summary of anatomical and postural varieties of thoracic outlet syndrome This rather uncommon parenchymatous disorder of the peripheral nerves, described by Parsonage and Turner,66,67 has no specific cause.68 However, two biopsy studies, mentioned by Stewart,36 may clarify the pathology and pathogenesis of this syndrome. They suggest that the disorder is the result of immune-mediated nerve damage following a previous viral infection or autoimmune process.69,70 It may develop at any age.71 The onset is with quite sudden central neck pain or pain in one or both scapulae. After some hours to some days the pain radiates to one or both upper limbs, sometimes as far as the hands. Even in bilateral distribution the picture is asymmetrical and paraesthesia is uncommon. The pain is extreme during the first weeks, continues for 2–3 months and then gradually diminishes. Sometimes coughing or taking a deep breath may also be painful. It takes another 2 or 3 months before the patient is comfortable. Once the acute stage of an attack is over and the initial pain has disappeared, a patchy paresis and atrophy will become evident. There is visible atrophy in shoulder and shoulder girdle72 and isometric testing reveals gross weakness in several muscles. All kinds of combinations of weakness may be possible. A typical feature of neuralgic amyotrophy is the patchiness of the motor and sensory symptoms. Histological studies have already shown that the pathologic process can cause very focal damage to one or a few of the fascicles that make up a brachial plexus trunk or cord, while simultaneously affecting several parts of the plexus as a whole.73,74 This is clinically reflected by a wide variety in the possible distribution – and severity – of paresis. Any part of the brachial plexus, and clinically any muscle or skin area can be involved, in all sorts of combinations. It is precisely the recognition of this patchiness that is a very important clue to the diagnosis of neuralgic amyotrophy.75 The muscles most often involved are: serratus anterior, deltoid, supraspinatus and infraspinatus, followed in frequency by biceps and triceps. The infraspinatus muscle seems to be always affected. Sensory abnormalities are much less pronounced than pain and weakness. Analgesics may be necessary during the pain period but the other symptoms and signs recover spontaneously. In the majority of patients, the weakness abates in the next few months after the disappearance of the pain.76 The long thoracic nerve takes origin in the upper trunk of the brachial plexus from the ventral rami C5, C6 and often C7. It courses behind the brachial plexus and follows the lateral wall of the thorax where it divides into several branches (Fig. 12). The long thoracic nerve is a pure motor nerve and innervates the serratus anterior muscle. The serratus anterior is a broad flattened sheet of muscle originating from the first nine ribs and passes posteriorly around the thoracic wall before inserting into the costal surface of the medial border of the scapula (Fig. 13).77 The main function of the serratus anterior is to protract and rotate the scapula, keeping it closely opposed to the thoracic wall and optimizing the position of the glenoid for maximum efficiency for upper extremity motion.78 The nerve can become affected: • As the result of iatrogenic causes, such as axillary or first rib surgery79,80 • As the result of direct compression (‘backpack injuries’) because of its long course along the thorax81 • As the result of excessive shoulder activity.82,83 Although the association is well established, there is no consensus of exactly how trauma injures the long thoracic nerve. Work on cadavers suggests that injury may take place as the nerve exits the fascial sheath that encompasses it, either in the form of a traction injury 84 or in a ‘bow-stringing’ effect85 The patient presents with pain around the affected shoulder, which either arises spontaneously or is linked to some traumatic event.86 This pain may radiate down the arm and to the scapula. In addition, he typically complains of shoulder weakness. The pain usually resolves spontaneously over the next several weeks, but the patient is left with weakness and a winged scapula.87 Upon inspection, medial scapular winging is evident, with the medial and inferior borders closer to the spine and lifted superiorly when compared to the normal side.88 Examination of the shoulder shows a limitation on active elevation of the arm of about 45–90°. Passive movements are of full range; resisted movements are normal. The diagnostic manūuvre is to ask the patient to push against a wall with the arms stretched out horizontally in front of the body (Fig. 14).89 In this position, the vertebral border of the scapula lifts further from the thoracic wall due to the loss of serratus anterior scapular protraction. In most cases spontaneous recovery occurs in 4–8 months.90 However, in approximately 25% of patients the paralysis and scapular winging will persist and such patients are then candidates for surgical reconstruction.91,92 The suprascapular nerve takes origin from the upper trunk of the brachial plexus with fibres from the C4 to C6 ventral rami. It courses through the posterior triangle of the neck, underneath the trapezius muscle. The nerve passes through the suprascapular notch of the scapula, which is bridged by the thick transverse scapular ligament93 (Fig. 15). After entering the supraspinatus fossa the nerve gives off two motor branches to the supraspinatus muscle and then passes laterally within the fossa, providing sensory branches to the posterior capsule of the glenohumeral joint and acromioclavicular joint. It then goes around the lateral border of the base of the spinous process to the infraspinatus fossa, where the nerve terminates by supplying motor branches to the infraspinatus muscle. The suprascapular nerve has a short course and several sites of relative fixation, making it vulnerable to both traction and compression forces. The nerve is fixed at both its origin at the Erb point on the brachial plexus and at its terminal insertion on the infraspinatus. The nerve is relatively fixed at the suprascapular notch, and anatomical studies have shown that motion does not occur at this point.94 Suprascapular nerve dysfunction can be caused by: • Entrapment of the nerve by a ganglion,95,96 or a tight ligament at the level of the suprascapular notch • Entrapment at the spinoglenoid notch97,98,99 • Acute brachial plexitis (the suprascapular nerve is involved in 97% of the cases)100 • Trauma, e.g. shoulder luxation or scapular fracture101 A lesion at the suprascapular notch is either the result of a ganglion cyst or a traction trauma. Downward traction of the scapula can result in opposition of the suprascapular nerve against the sharp inferior border of the transverse scapular ligament. Cross-body abduction or protraction with forward flexion, as seen in fencing, throwing sports,102 racquet sports, and weight lifting, have also been found to maximally stretch the suprascapular nerve. Entrapment can also occur more distally at the spinoglenoid notch, which is more commonly seen in athletes whose sports require rapid forceful external rotation movements, such as volleyball.103,104 The cocking motion for the smash results in rapid external rotation of the shoulder; this rapid motion of the infraspinatus muscle is thought to pull the suprascapular nerve against the base of the scapular spine, resulting in nerve injury at this level. Injury to nerves in the spinoglenoid area has also been noted secondary to ganglion cysts. An EMG shows a denervation of the infra- and supraspinatus which, together with the history of an injury, confirms the diagnosis. Ultrasonography can be used to show a ganglion. Magnetic resonance imaging is appropriate to diagnose entrapment.105 The management for suprascapular nerve entrapment includes a conservative regimen of observation, rest, analgesics, and cortisone injections into the suprascapular notch.106,107 If this treatment is unsuccessful, surgical decompression of the nerve at the suprascapular ligament is necessary. In most patients it leads to full relief.108,109 The patient sits on a chair. The entire spine of the scapula is marked from the medial to the lateral edge. This line is bisected and a second line drawn at a 45° angle in an anterolateral direction. A 2.5 cm mark is made on this second line and a 7 cm needle, fitted to a syringe containing 2 ml of steroid, is inserted vertically downwards at this point until it hits the bone at the base of the scapular spine (Fig. 16). The tip of the needle is then moved further anteriorly until it slips in the suprascapular notch. The steroid is injected here. The axillary nerve takes origin in the posterior cord of the brachial plexus from fibres derived from C5–C6. It curves around the neck of the humerus and passes through the quadrilateral space close to the inferior shoulder joint capsule. This quadrilateral space is bounded by the teres minor superiorly, the long head of the triceps medially, the teres major inferiorly, and the humeral neck laterally and forms a potential site of compression for the axillary nerve as it passes from the anterior to the posterior aspects of the shoulder.110 After passing through the quadrilateral space, the axillary nerve divides into anterior and posterior branches, which supply the anterior and posterior portions of the deltoid muscle. The posterior branch of the axillary nerve also supplies the teres minor and supplies cutaneous sensation overlying the deltoid (the upper lateral cutaneous nerve of the arm). The short length of the axillary nerve renders it vulnerable to stretch injuries, especially during shoulder dislocation 111 (Fig. 17). • Most axillary nerve lesions occur after anterior shoulder dislocation,73 the exact incidence ranging between 9% and 18%.112 Blunt trauma to the anterior aspect of the shoulder without dislocation has also been implicated in axillary nerve trauma in contact sports.113,114 • Acute axillary neuropathy is also associated with backpacking, usually in inexperienced hikers. The cause of axillary nerve injury in ‘rucksack palsy’ is thought to be traction caused by depression of the shoulder from the excessively weighted backpack. • Quadrilateral space syndrome represents a chronic compression syndrome of the axillary nerve in throwing athletes.115 Axillary nerve entrapment then occurs insidiously in the quadrilateral space without history of trauma. Fibrous bands at the inferior edge of the teres minor have been implicated, as have randomly oriented fibrous bands found in the quadrilateral space.116,117 • The axillary nerve sits approximately 2 cm inferior to the usual posterior portal for arthroscopy, putting this nerve at risk during routine arthroscopic procedures.118 An unintentional local infiltration with steroid into the axillary nerve on infiltrating too far distally for infraspinatus tendinitis may cause the same problem. Symptoms are often vague, consisting of a dull ache and/or pins and needles over the deltoid area. Sometimes extensive visible wasting of the deltoid is present, together with an area of cutaneous analgesia in the mid-deltoid region. According to Cyriax,119 (his p. 153) some patients tend to relax the axillary nerve as much as possible by elevating the scapula at the same side during the first few weeks after the injury. The process is a consequence of spasm of the trapezius and leads to pain on passive side flexion of the neck towards the contralateral side. Deltoid weakness is often masked by the activity of supraspinatus and pectoralis major.120 Because the supraspinatus muscle is not involved, active elevation of the arm remains possible, and weakness is only found on resisted abduction. The diagnostic test is to ask the patient to abduct the arm to 90° and to bring it further backwards into horizontal extension (Fig. 18). This is impossible with an axillary nerve lesion. Spontaneous cure is possible, but takes about 6 months. Care should be taken to mobilize the shoulder during the recovery so as to avoid an immobilizational arthritis. If no improvement has occurred after 6 months, surgical decompression is needed via a release of the teres minor and major tendinous insertions.121 The posterior interosseous nerve winds around the neck of the radius and goes into the dorsal compartment of the forearm. It pierces the supinator muscle through the arcade of Fröhse and runs deeply under the extensors as far as the wrist (Fig. 19). The radial nerve is quite frequently affected by pathological conditions. This happens in more generalized diseases, such as poisoning by heavy metals (e.g. lead), but also in more localized lesions, either traumatic or following entrapment of the nerve tissue. The symptoms and signs depend on where, along the nerve, the lesion lies. The radial nerve may become affected at five different sites: the proximal and middle part of the upper arm, the distal part of the upper arm, the proximal part of the forearm and the distal part of the forearm (Table 3). When the lesion results from an injury – fracture or dislocation of the humerus – it is usually combined with an axillary palsy.101 Space-occupying lesions in the axilla or the use of old-fashioned axillary crutches are other (rare) causes.122,123 Lesions are more common at the distal than the middle and proximal part of the arm. The palsy may be traumatic – fracture of the humerus,124,125 fracture or dislocation of the elbow – or may result from a sustained pressure just proximal to the elbow. This is typically the case in a patient who has fallen asleep with the arm over the edge of a chair or has lain all night with the arm resting against the hard edge of a bunk – ‘Saturday night paralysis’. The full radial syndrome develops, except that the triceps and anconeus muscles are unaffected, as is the brachioradialis muscle. The patient awakes with a painless dropped wrist. Level with the head of the radius, the radial nerve divides in its two terminal branches – the superficial (sensory) and deep (motor) branches (see Fig. 19). The latter then forks off into (1) muscular rami running towards the supinator, extensor digitorum, extensor digiti minimi and extensor carpi ulnaris muscles, and (2) the posterior interrosseous nerve of the forearm, which supplies the long abductor and extensors of the thumb as well as the extensor indicis proprius. When a lesion occurs proximal to this division, symptoms of both are combined. As the branches supplying the brachioradialis, extensor carpi radialis longus and brevis, and brachialis escape the compression, there is only weakness of supination, extension of the fingers, ulnar deviation of the wrist and extension and abduction of the thumb. Just below the point where the deep radial nerve comes to lie at the dorsal aspect of the forearm, the posterior interrosseous nerve of the forearm branches off and passes through the deep and superficial heads of the supinator brevis muscle126 (Fig. 21). When the edge of the upper border of the superficial head has become fibrous, this opening forms the arcade of Fröhse,127 also called the radial tunnel. The nerve then passes further down along the interrosseous membrane and innervates the abductor pollicis longus, extensor pollicis longus and brevis, and extensor indicis proprius muscles. The posterior interosseous nerve can be compressed as the result of: (1) an injury, usually a fracture (or the hardware used to fix fractures),128,129 or elbow joint dislocation;130 (2) space-occupying lesions, such as synovial proliferations from the elbow joint in rheumatoid arthritis131,132 or soft tissue tumours,133,134 for example lipomas;135 or (3) fibrous bands, which can be traumatic in origin (e.g. Volkmann’s contracture) or developmental (arcade of Fröhse).136–140 Many authors believe that compression of the posterior interosseous nerve at the point where it passes through the arcade of Fröhse is a cause of lateral elbow pain and they therefore consider it as a type of tennis elbow. We do not agree that this condition should be considered to be a (resistant) type of tennis elbow, because the lesion does not lie in the extensors of the wrist. Hagert et al141 also regarded epicondylitis and posterior interosseous nerve entrapment as ‘two different disorders, which have nothing to do with each other, and which should therefore not be mixed up’. In 1883, Winckworth stated that the posterior interosseous nerve could become compressed where it passes through the supinator muscle.142 Since Roles and Maudsley described the radial tunnel syndrome in 1972,143 this pathology has become recognized as a cause of resistant tennis elbow.133,136,144–146 This idea is based on the reports of good results after surgical decompression of the posterior interosseous nerve at the radial tunnel.147,148 In compression of a predominantly motor nerve, such as the posterior interosseous nerve, the main symptom would be paralysis. Kopell and Thompson, however, state that entrapment of a motor nerve may cause diffusely localized dull aching pain.149 The pain would originate from the nociceptive thin or non-myelinated afferent nerve fibres of muscular and extramuscular origin.150 However, the symptoms described by different authors are very similar to those found in tennis elbow: pain at the lateral side of the elbow, radiating distally along the posterior aspect of the forearm. The pain may be constant and can be brought on or aggravated by exertion, especially rotation movements, and the symptoms continue for some time after the causative strain has ceased. There is also diffusely localized pain on resisted supination and/or pronation as well as on resisted extension of the middle finger. Local tenderness is present over the proximal and posterior aspect of the forearm, at the suspected entrapment site. These symptoms and signs correspond with the clinical picture of what we have described as type IV (muscular) tennis elbow (see p. 313). Werner analysed the hypothesis that posterior interosseous nerve entrapment can be a cause of lateral elbow pain.151
Nerve lesions and entrapment neuropathies of the upper limb
Disorders of the spinal accessory nerve
Anatomy
Innervation
Disorders
Mononeuropathy of the spinal accessory nerve
Disorders of the brachial plexus
Anatomy
Peripheral nerve
Traumatic disorders
Upper brachial plexus palsy
Nerve
Muscle
Long thoracic
Serratus anterior
Dorsal scapular
Rhomboids
Suprascapular
Supraspinatus
Infraspinatus
Axillary
Deltoid
Teres minor
Musculocutaneous
Coracobrachialis
Biceps
Radial
Brachioradialis
Supinator
Space-occupying lesions
Thoracic outlet syndrome
Anatomy
Types
Anatomical variety
Vascular compression
Postural variety
Acute onset
Slow onset
Functional examination
Sustained elevation of the shoulders
Other tests
Roos’ test
Technical investigations
Differential diagnosis
Compression of the ulnar nerve
Compression of the radial nerve
 radial digits. Resisted extension of the hand is weak but painless. Sometimes a drop hand is found (see p. e132 of this chapter).
radial digits. Resisted extension of the hand is weak but painless. Sometimes a drop hand is found (see p. e132 of this chapter).
Carpal tunnel syndrome
Carcinoma of the superior sulcus of the lung (Pancoast’s tumour)
Treatment
Postural variety
Posture and exercise
Surgery
Anatomical
Postural
Age
20–30 years
Middle-aged and elderly
Release phenomenon?
At first
All the time
Pins and needles?
All day
At night
Atrophy and weakness?
Thenar/hypothenar/interossei
None
Cold hands?
Possible
None
Cynosis and swelling?
Possible
No
Treatment
Surgery
Keeping shoulders slightly shrugged at all times; daily exercises in the evening
Plexitis
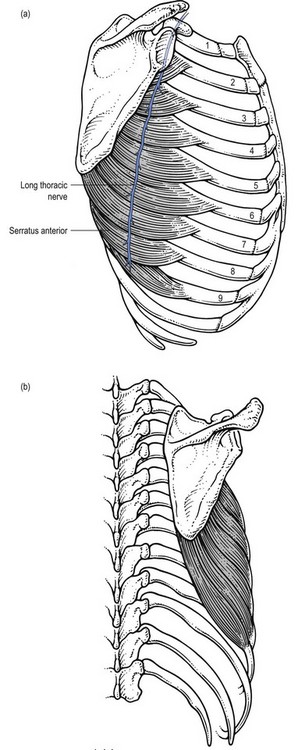
Disorders of the long thoracic nerve
Anatomy
Innervation
Disorders
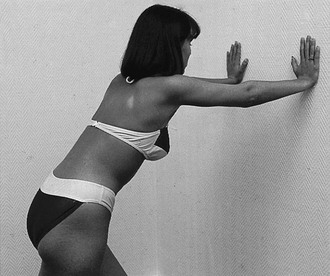
Mononeuropathy of the long thoracic nerve
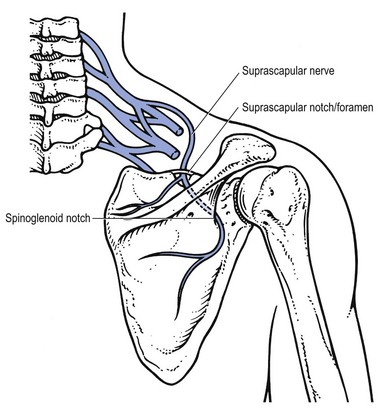
Disorders of the suprascapular nerve
Anatomy
Disorders
Technique: injection
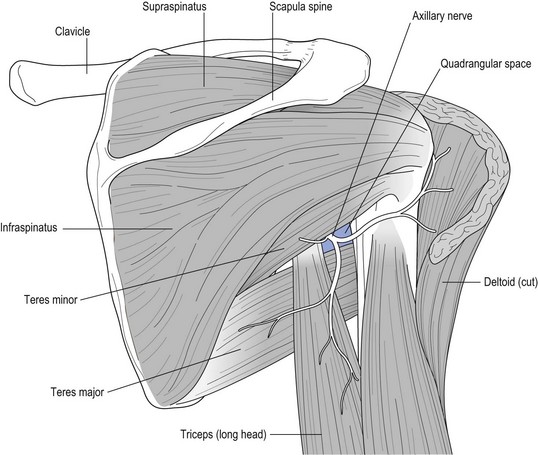
Disorders of the axillary nerve
Anatomy
Disorders
Disorders of the radial nerve
Anatomy
Disorders
Lesions at the proximal and middle part of the upper arm
Lesions at the distal part of the upper arm
Lesions at the upper part of the forearm
Posterior interosseous nerve of the forearm
Radial tunnel syndrome
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







 radial digits.
radial digits.