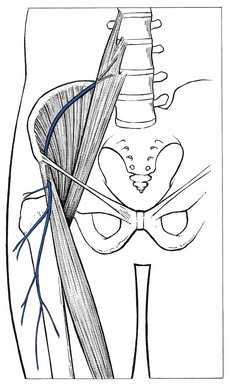
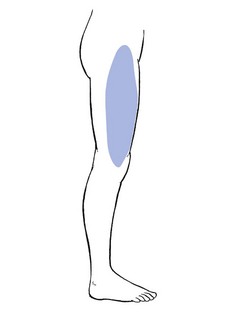
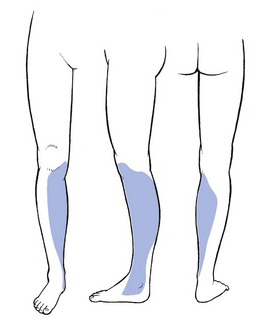
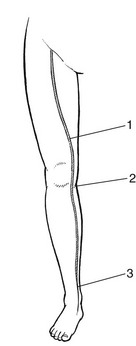
The main symptom of pressure on nerves is paraesthesia. Depending on the level of the compression, paraesthesia is accompanied by pain and numbness. The combination of these three symptoms and their interrelation are of importance in localizing the site of compression.1 The effects of pressure on the peripheral nerves of leg and foot are discussed in this chapter. Neurocompression syndromes of the sciatic nerve are not common. Some believe that the nerve can become compressed between the fibres of the piriformis muscle (the piriformis syndrome2). If the nerve becomes damaged or is chronically irritated, serious deafferentation pain can result and occurs in circumstances in which the sciatic nerve is locally bruised or has undergone damage after local injection of irritating substances. Continuous and burning pain, independent of posture, is then felt in the sensory distribution of the nerve. Local pressure on the nerve can increase the pain considerably.3–4 The lateral cutaneous nerve is sensory only. It originates at L2 and runs retroperitoneally to emerge at the outer edge of the psoas and then crosses the iliacus muscle at the lateral border of the pelvis, which it follows to the anterior superior spine of the ilium. It then passes under the lateral aspect of the inguinal ligament to follow the fibres of the sartorius muscle. Its course and the location as it exits the pelvis are very variable. Aszmann et al5 investigated its relation to soft-tissue and bony landmarks in the inguinal region through dissection of 52 human anatomic specimens and identified five different types: type A, posterior to the anterior superior iliac spine, across the iliac crest (4%); type B, anterior to the anterior superior iliac spine and superficial to the origin of the sartorius muscle but within the substance of the inguinal ligament (27%); type C, medial to the anterior superior iliac spine, ensheathed in the tendinous origin of the sartorius muscle (23%); type D, medial to the origin of the sartorius muscle located in an interval between the tendon of the sartorius muscle and thick fascia of the iliopsoas muscle deep to the inguinal ligament (26%); and type E, most medial and embedded in loose connective tissue, deep to the inguinal ligament, overlying the thin fascia of the iliopsoas muscle and contributing the femoral branch of the genitofemoral nerve (20%). Other studies located the nerve most commonly at 10–15 mm medial to the anterior superior iliac spine but in some cases it was located as far medially as 46 mm.6,7 A few centimetres below the anterior superior iliac spine it emerges through the deep fascia and continues its course subcutaneously (Fig. 1). The nerve supplies the anterolateral aspect of the thigh from the upper border of the trochanter to the level of the superior margin of the patella (Fig. 2). The nerve can become trapped at any point along its course, although most cases result from nipping at the inguinal ligament or beyond the fascial tunnel, usually at the point where the nerve becomes superficial. Occasionally the symptoms stem from an abnormality in the pelvis, the typical example of which is meralgia during pregnancy (Cyriax:1 pp. 297–298), encountered between the fourth and seventh months. In this condition, the symptoms are always unilateral and disappear spontaneously during the pregnancy. They have been ascribed to the pressure of a small fibromyoma against the nerve, close to where it emerges at the lateral border of the psoas. Meralgia paraesthetica has also been reported after pelvic osteotomies for Perthes’ disease,8,9 shelf operations for acetabular insufficiency10 and after the removal of bone from the iliac crest for a graft.11 However, most cases of meralgia paraesthetica are idiopathic, although some external causes such as tight trousers,12 obesity,13 the use of belts, corsets and trusses, or an overtight bandage round the pelvis14 after an operation or during pelvic traction can compress the nerve just medial to the anterior superior iliac spine. The symptoms are typical of any lesion of a small peripheral sensory nerve: pain, paraesthesia and numbness, confined to its distribution. The patient typically describes a burning or tingling sensation over the anterolateral aspect of the thigh. The edge is well defined and the centre is often completely anaesthetic. A common complaint is hypersensitivity: the patient even dislikes the touch of a cloth in the affected area.15 Clinical examination reveals the extent of anaesthesia, which has a clear edge. Tenderness to pressure can sometimes be evoked distal to the anterior superior iliac spine. In some cases, the paraesthesia can be aggravated by tapping the nerve.16,17 Differentiation of meralgia paraesthetica from a second lumbar root lesion remains the greatest problem in diagnosis18 and relies on the careful delineation of the paraesthetic area, the degree of numbness and a negative MR scan of the lumbar spine.19,20 Although the L2 area and the area supplied by the lateral cutaneous nerve correspond well laterally, the second root also contributes to the innervation of the groin and the inner aspect of the thigh. Furthermore, in L2 root lesions the analgesia is very slight because of the overlap between L2 and L3, whereas in lesions of the lateral cutaneous nerve, there is almost full anaesthesia, with a clear-cut border (Box 1). A 10 ml syringe is filled with procaine 0.5% and fitted to a thin needle 5 cm long. A point is chosen 5 cm below and medial to the anterior superior iliac spine. The needle is inserted and moved upwards along the anterior and medial side of the sartorius muscle. A fan-wise infiltration is made here.21 Two to four weekly infiltrations may be necessary. In intractable cases surgery can be considered.22 It should be remembered, however, that in about two-thirds of cases the symptoms subside spontaneously over 2 years.23,24 Although the femoral nerve can be compressed by different processes in the psoas region, the pelvis and the groin, neither pain nor paraesthesia ever result.25 The symptoms are a vague numbness in the anterior crural area and increasing weakness of the psoas and quadriceps femoris muscles. A new cause of femoral compression neuropathy has been reported during recent decades – retroperitoneal bleeding resulting from anticoagulant therapy.26–28 The anterior cutaneous nerve innervates the skin of the front of the thigh as far as the upper border of the patella (Fig. 3). It can be compressed at the point where it emerges through the fascia of the thigh, some 10 cm below the inguinal ligament. Local pressure or friction may cause pins and needles and cutaneous analgesia confined to the anterior aspect of the thigh, with a clear-cut border and almost complete numbness towards the centre of the area. Treatment is removal of the external pressure and procaine infiltrations. The saphenous nerve is the largest cutaneous branch of the femoral nerve. It leaves the subartorial canal about 8–10 cm above the medial condyle of the knee. Some of the branches there provide innervation of the medial aspect of the knee. Another branch follows the sartorius muscle and becomes superficial just below the medial condyle of the tibia.29 It then runs down on the leg to follow the great sapheneous vein over the anterior aspect of the medial malleolus (see Fig. 6). Its territory of distribution is the medial side of the leg, the medial malleolus and the medial border of the foot30 (Fig. 4). Traction on the saphenous nerve as it leaves the subsartorial canal may cause oedema, inflammation and thus compression31–33 (Fig. 5). Direct compression of the nerve may also occur in front of the inner tibial condyle.34,35 However, the usual site of compression is at the ankle, at the anterior aspect of the medial malleolus. Saphenous neuralgia is also a well-known and common complication after harvesting of great saphenous vein for coronary artery bypass grafting. The main symptom is anaesthesia which may persist for a considerable time postoperatively.36–38 Paraesthesia over the inner aspect of the ankle and along the medial border of the foot, together with aching and numbness along the subcutaneous border of the tibia, results from either a direct contusion or sustained compression. Combined plantiflexion and eversion of the foot or flexion of the hallux may stretch the nerve and cause sharp neuralgic twinges.39 The common peroneal nerve emerges at the upper and lateral aspect of the popliteal fossa, through the fascia between the biceps femoris tendon and the lateral head of the gastrocnemius.40 It follows the biceps to the neck of the fibula where, under a fibrous edge beneath the origin of the peroneus longus, it divides into two branches. The superficial peroneal nerve continues under the peroneus longus, first along the fibula and then between peroneus longus and brevis.41 The deep peroneal nerve winds around the fibular neck and runs through the anterior compartment between the extensor hallucis and tibialis anterior muscles until it traverses the ankle deep to the inferior extensor retinaculum. Compression or elongation of the common peroneal nerve classically occurs where it winds round the lateral aspect of the neck of the fibula.42 Direct compression follows immobilization in an over-tight plaster cast, fracture of the neck of the fibula or externally from pressure of the fibular head against a hard surface such as the side of a desk. Iatrogenic injury of the peroneal nerve can also occur from direct manipulation during orthopaedic surgery or with prolonged compression during lateral hip and leg rotation with knee flexion as occurs in operative positioning.43 Elongation is frequent from sitting with the knees bent and the foot in full passive plantiflexion and inversion44 or from prolonged squatting.45
Nerve lesions and entrapment neuropathies of the lower limb
Introduction
Sciatic nerve
Lateral cutaneous nerve
Technique: infiltration
Femoral nerve
Saphenous nerve
Common peroneal nerve
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Musculoskeletal Key
Fastest Musculoskeletal Insight Engine