Chapter 29 Knee orthoses for sports-related disorders
To offset some of the confusion, the American Academy of Orthopaedic Surgeons classified knee braces into three categories: (1) prophylactic braces, intended to prevent injury in a healthy individual; (2) functional braces, designed to provide stability to the unstable knee, and (3) rehabilitative braces, designed to allow protected range of motion during the rehabilitation or early postoperative period.4
Knee joint biomechanics
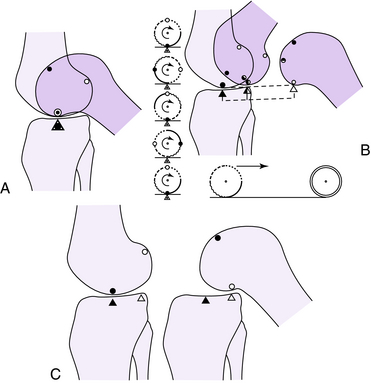
The knee joint acts as a hinge, allowing flexion and extension in the sagittal plane of motion (Fig. 29-1). However, flexion and extension occur about a constantly changing center of rotation, called polycentric rotation.42 This allows for a process called femoral rollback. As knee flexion starts in full extension, the femoral condyle begins to roll without sliding, and with further knee flexion sliding becomes more predominant. The knee joint also undergoes axial rotation during flexion and extension. Axial rotation occurs because of a differential radius of curvature between the medial and lateral femoral condyles, the convex shape of the medial tibial plateau, the concave shape of the lateral tibial plateau, and the ability of the MCL to stretch more rapidly than the lateral collateral ligament. As a result, when the knee joint continues to flex throughout the entire range of motion, there is inward rotation of the tibia, whereas the reciprocal is true with knee extension.
Knee stability
The function of the knee motion also depends on the four major ligamentous structures of the knee, specifically the ACL, PCL, MCL, and LCL structures. Kapandji50 described the dependence of knee stability on these structures as the four-bar linkage system. These ligaments are responsible for maintaining knee stability during femoral rollback and axial rotation of the knee joint. If the knee orthosis does not accommodate normal knee kinematics, range of motion may be limited, or the ligaments may be stressed leading to laxity.38
Brace design
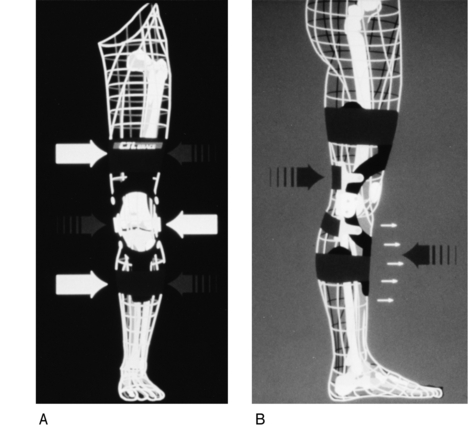
Knee braces are designed to transfer load while allowing for normal knee motion (Fig. 29-2). This depends on the amount of leverage the knee brace can provide. Longer braces produce a greater amount of leverage; therefore, athletes typically select the longest brace that provides the best fit to the extremity.18 The optimal position to apply the leverage depends on the goal of the knee brace. Prophylactic braces usually are designed with unilateral, single-hinge systems. Some newer designs have bilateral uprights and polycentric hinges. They are used to prevent MCL strain by applying leverage laterally on the femur and tibia to inhibit excessive valgus. Functional knee braces typically are designed with bilateral, polycentric hinge systems. These braces act to prevent recurrent instability in patients with ACL tears. They act by applying leverage to resist abnormal forward translation of the tibia on the femur.35
Off the shelf
Both off-the-shelf and custom-made designs have proven effective if the geometry of the brace matches the geometry of the extremity.12 Off-the-shelf knee braces are designed based upon the approximate geometry and length of the individual knee. Therefore, it is recommended that athletes try on different braces from different companies in order to determine the best fit.
Custom
Custom knee braces usually are cast molded or leg traced to match the shape of the brace to the geometry of the thigh, knee, and calf. Theoretically, custom designs more accurately recreate normal knee motion; however, studies have shown that even custom designs limit knee flexion in the swing phase of running compared to unbraced conditions.54,55
Ultimately, brace efficacy is dependent on how load is distributed across the limb. This is dependent on a number of factors, including geometry and mechanism of attachment, fabrication materials, and hinge design.74
Hinge design
In order for the knee brace to function properly, the knee hinge must recreate polycentric rotation and femoral rollback (Fig. 29-3). Simple unicentric hinges, as used in prophylactic braces, do not allow normal knee joint kinematics. Newer polycentric hinges, as used in functional braces with dual hinges, have been developed that more closely approximate normal knee kinematics.24 Ultimately, optimal brace performance depends on placing the hinge(s) in correct relation to the femoral condyles.74
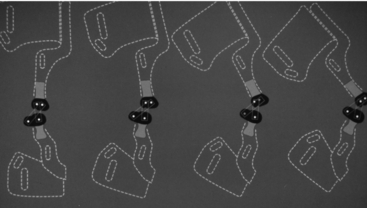
Fig. 29-3 Kinematic hinge designed to replicate femoral rollback with knee flexion.
From Goldberg B, Hsu JD: Atlas of orthoses and assistive devices, ed 3, St. Louis, 1997, Mosby.
There is a great deal of debate on which factor is the most important. Based on mathematical models, some authors have found that the mechanical characteristics of the brace, the structural integrity of the brace, and the interaction of the brace with the limb during loading are the most important.57 Others authors have suggested that hinge position is the most important.94
Brace design limitations
As previously stated, single-hinge knee braces have been criticized for prestressing ligaments and causing chronic ligamentous laxity, whereas double-hinge systems more accurately recreate normal knee motion and avoid these complications.38 Braces have a tendency to migrate distally because the soft tissue consists of compressible materials. This limits the knee brace’s ability to apply leverage. Authors recommend adequate sizing, tightening of straps, tape, or hook-and-pile fasteners, and shaving leg hair to decrease this potential for lost leverage.74 Additionally, braces provide little control of axial rotation because they offer limited ability to resist translational loads. Because of the exposed metal, brace-induced injuries have been known to be inflicted on other players. Finally, braces have an endurance limit, such that repetitive cyclic loading of the components eventually may lead to plastic deformation and ultimate failure of the knee brace.24
Clinical relevance
The actual ACL injury rate to the knee remains quite low, approximately 80,000 per year annually in the United States.29 The highest incidence appears to occur among 15- to 25-year-old athletes who participate in pivoting sports. Some studies have suggested that the rate of knee injuries, specifically ACL tears, may be increasing88; however, other authors have concluded that the injury rate remains unchanged.1 Gender differences in the rate of knee injuries do exist. In fact, data suggest that collegiate female athletes participating in the same activity are two to eight times more likely to sustain an ACL injury than are males.1,6 Some authors have suggested that delays in the treatment of these injuries may be associated with an increased risk of medial meniscus tears.66
The amount of force acting on the normal ACL depends upon the activity the knee is experiencing. Forces range between 400 N during normal daily activities to much higher forces during strenuous activity.70,71 Although the ultimate strength of the ACL is age dependent, the average ultimate strength is 2,100 N.97 Some researchers have attempted to use knee braces to limit the force experienced by the ACL in order to prevent injury. However, if the force exerted on the ACL is greater than its ultimate strength, an ACL rupture will still occur.
Approximately 30% of ACL injuries are thought to be due to direct contact between another player or object; the other 70% are believed to be the result of noncontact mechanisms, including pivoting and decelerating activity, “out of control play,” and awkward landings.40 Risk factors for noncontact injuries, including environmental, anatomic, hormonal, and biomechanical factors, have been suggested.
Because the ACL is composed of fibrocartilage, it does not have an intrinsic ability to heal itself.45 ACL-deficient athletes often note a “giving way” or instability after attempts to return to sport because the ACL is the primary restraint to anterior tibial displacement. As a result of the functional instability, the secondary restraints of the knee are often injured.23 Current recommendations for return to play in the ACL-deficient athlete mostly include surgical ACL reconstruction because of the repercussions of conservative management of the unstable knee. However, some have used knee braces to facilitate functional return to sport in an ACL-deficient knee and as an adjunct to surgical intervention in the postoperative rehabilitative period.
PCL tears represent approximately 3% to 37% of all knee ligament injuries, depending on the mechanism of injury.22,67 A PCL injury is sustained as the result of contact (posterior force directed against a flexed knee) and noncontact (hyperextension) mechanisms.44 No study has reported a trend toward an increasing incidence or gender difference in PCL injury. The PCL is the primary restraint to posterior tibial displacement and secondary restraint to external rotation.19 With PCL rupture there is posterior subluxation of the tibia on the femur. This has been shown to result in increased contact pressures in the patellofemoral joint and medial femoral condyle.60,87 Some older short-term studies have noted that patients with PCL injuries who are treated nonoperatively do well.28,34,92,93 Other long-term studies have shown that the clinical and radiological incidence of degenerative joint disease increases in proportion to length of time after PCL injury to the knee.22,26,52,75 Interestingly, the PCL has the intrinsic ability to heal itself because it is made of fibroblastlike cells.83,84 This may allow for full functional recovery with proper nonoperative management. In some cases this may include the use of rehabilitative braces.44 However, one must be aware that the PCL may heal in a lengthened position.32
The incidence of MCL injury is difficult to determine because of the wide spectrum of injury severity. Additionally, the ACL, PCL, or LCL may be injured concomitantly. Most injuries occur as a result of significant valgus stress applied to the lateral aspect of the knee, as the MCL is the primary medial restraint to valgus loading.95 Then, with increasing stress, the ACL and PCL provide medial restraint.36,77 The MCL also provides resistance to abnormal external tibial rotation.41
Historical perspective
Historically, casting was used to treat knee injuries and fractures about the knee.59 Unfortunately, some patients had residual knee stiffness and functional instability of the knee joint.53 Knee orthoses originally were designed to treat congenital and acquired deformities around the knee, including genu varum and quadriceps paralysis in polio patients. More recently, Sarmiento81 used knee orthoses in a rehabilitative setting to treat fractures about the knee while preventing loss of range of motion. In the 1960s and 1970s, physicians began using orthoses to treat athletes with functional knee instability from ACL injuries.25 In the late 1970s, Anderson et al.5 modified a rehabilitative brace, the Anderson Knee Stabler, to prevent recurrent injury to the medial collateral ligament. Physicians, coaches, and players then started to use these braces to prevent knee injuries.
Prophylactic braces
Prophylactic knee braces have been used mostly by football and lacrosse players to prevent MCL and ACL injury. The prophylactic knee braces attempt to limit the strain on the MCL and ACL by redirecting a lateral impact force away from the joint line to points more distal on the tibia or femur (Fig. 29-4).33 There is a great deal of controversy surrounding the use of a prophylactic knee brace in sport.
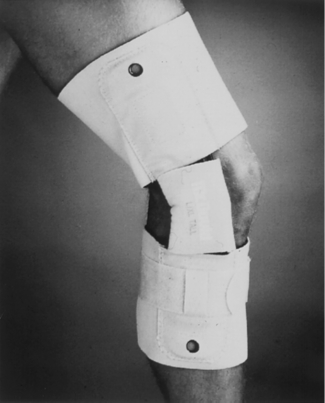
Fig. 29-4 McDavid lateral hinge prophylactic knee brace.
From Insall J, Scott W: Surgery of the knee, ed 3, Philadelphia, 2001, Churchill Livingstone.
Current research
Current research has attempted to document brace effectiveness more objectively. Biomechanical testing of surrogate limb models and cadaveric specimens have attempted to define the role of bracing in sports. However, these testing methods are limited by lack of active muscle contraction and poor soft-tissue compliance, both of which influence the measurement of strain on knee ligaments.12
Using a cadaveric model, Meyer et al.65 compared a lateral, upright brace (Anderson Knee Stabler, Omni Scientific, Lafayette, IL) and a bilateral, nylon upright brace (AmPro, APO, Iowa City, IA) to a nonbraced condition under dynamic valgus loading. They found a decrease in load-induced MCL elongation with the AmPro (25.1%) and the Anderson Knee Stabler (18.3%) versus the unbraced knee. However, the knees were loaded at relatively slow speeds of 100 mm/s, which does not emulate actual game play environment.
Using a surrogate knee model in 10 knee braces, Liu et al.58 found that only two braces, the Townsend (Townsend Design, Bakersfield, CA) and the Marquette Knee Stabilizer II (Vixie Enterprises I, Eugene, OR), effectively limited anterior tibial translation at 400 N. These braces were bilateral hinge, post, shell designs. Most other braces failed at forces less than 300 N.
France et al.36 tested six different knee braces—DonJoy (dj Orthopaedics Inc., Vista, CA), Anderson Knee Stabler (Omni Scientific, Vista, CA), Stromgren (Stromgren, Hays, KS), Mueller (Mueller, Prairie du Sac, WI), Tru-Fit, and McDavid—for their ability to prevent MCL or ACL injury. They reported that braces were most effective for large-mass, low-velocity impacts with the hip and ankle fixed and the knee extended. Only the DonJoy, a unilateral upright, dual-hinged knee brace, provided an impact safety factor (ISF) > 1.50 more than 50% of the time for the MCL testing conditions. None of the braces protected the ACL at ISF > 1.50. Overall, they concluded that braces with the greatest stiffness and that were offset from the knee to prevent premature joint contact had the greatest ISF, but that none of the braces provided the level of protection necessary to prevent MCL or ACL injury at high-impact loads.
Paulos et al.76 provided data from a surrogate limb model suggesting that bracing increased the impact duration, which protected the ACL more than the MCL. They concluded that bracing does provide some degree of protection to the ACL and MCL under direct lateral impact.
Brown et al.17 found a direct relationship between tightness of the brace tension and the degree of relative MCL strain attenuation achieved. Daley et al.27 used Brown’s model to test the effectiveness of knee braces with varying hinge length and offset, upright length, breadth, thickness, and cuff surface area. They showed that the best design simulated the original Anderson Knee Stabler.
Erickson et al.33 measured in vitro MCL and ACL strain values during dynamic loading in four unilateral, upright prophylactic knee braces (Anderson Knee Stabler, McDavid Knee Guard, DonJoy, SMI Preventive Knee Brace, and DePuy Knee Protector [BSN Medical, Charlotte, NC]). They found that the prophylactic brace was able to reduce the impact load at the point of contact and reduce the resulting lengthening in both the MCL and ACL. However, only the DonJoy brace significantly lowered the peak strain in the MCL at 30 degrees of knee flexion, whereas the McDavid brace significantly reduced the peak strain of the MCL at full knee extension. None of the braces decreased the amount of ACL strain from a valgus force.
Based on in vivo Hall data, Beynnon et al.10 suggested that any protective effects on ACL strain relief are minor. They have concluded that under weight-bearing conditions, a prophylactic knee brace probably would not protect an ACL from injury during a rapid valgus stress at high speeds.
Beynnon et al.12 loaded the knee while subjects were wearing three custom and four off-the-shelf braces and tested the Hall-effect strain behavior in the ACL. At low anterior shear loads, two braces provided some protection, but at higher anterior shear loads, no brace provided protection. Beynnon et al.11 also showed that because of the compressive load across the knee produced during weight bearing, braces are not able to reduce ACL strain.
Any strain relief for the MCL provided by a unilateral, upright, off-the-shelf brace appears to be minor (20%–30%) based upon the surrogate knee model studies. However, prophylactic knee braces may be able to help prevent ACL injury caused by excessive medial opening at the time of valgus loading at low loads only. Some authors have suggested that clinical and laboratory knee bracing studies should address different levels of play (high school, college, and professional) and different types of sports (football, skiing, and soccer).69
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree