Fig. 24.1
Classification of knee instabilities
In recent years, the diagnostic and therapeutic procedures to treat knee ligament injuries have changed. New imaging methods, such as three-dimensional reconstructions of CT scans and MRI slices and sequences, help to complete imaging information. Despite these new imaging methods, the clinical examination of the knee is still crucial. The manual examination provides essential information about the function and the functional stability of the knee.
24.2 Anterior Cruciate Ligament (ACL)
No single structure in the knee joint has created more interest in the scientific community than the anterior cruciate ligament.
24.2.1 Anatomy
The ACL consists of two functional bundles: the anteromedial bundle (AM) and the posterolateral bundle (PL) (Fig. 24.2). Their tension differs depending on joint position. They show a reciprocal tension pattern. In extension, the PL shows maximal tension. The AM shows maximum tension in flexion. These two bundles stabilize the tibia against anterior translation in different joint positions. Because the PL bundle shows maximal tension during extension, it also plays an important role in providing rotational stability [21].
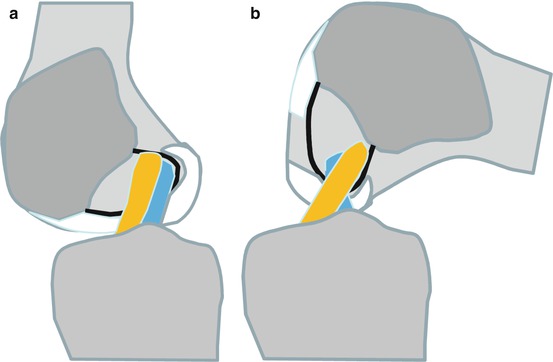
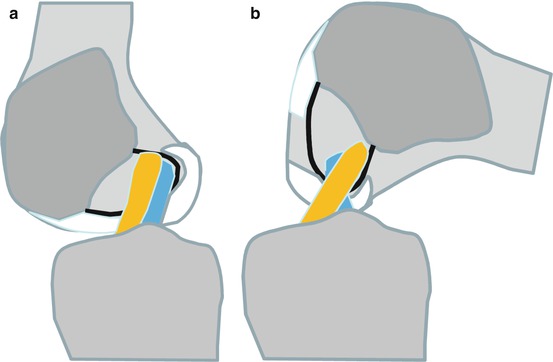
Fig. 24.2
Anatomy of the anterior cruciate ligament. (a) The PL bundle is tight in extension. (b) The AM becomes tight with flexion
24.2.2 Trauma Mechanism
The reported incidence of ACL rupture is 1 per 3,500 habitants [9]. The main reasons are accidents in sports. Sports requiring pivoting and jumping, such as soccer, basketball, and handball, are especially high-risk activities for ACL rupture. Alpine skiing should also be mentioned in this context. Many analyses have shown that ACL ruptures are more frequent in female than in male athletes [2, 16, 22].
Video analyses have provided information about the rupture mechanism. According to these analyses, ACL rupture mainly occurs without direct contact with an opponent athlete. The majority of ACL ruptures occur in so-called noncontact situations [22]. The most dangerous situations are:
1.
Landing after a jump
2.
Sudden stops
3.
Sudden rotation moves
At time of injury, the body shows a straight position and the knee and the hip are flexed slightly (5–25° flexion in the knee joint). The lower leg is rotated externally and is in a valgus position. These joint positions produce maximal tension on the ACL fibers. Most athletes report a fixed foot at time of injury, so that a rotation of the foot isn’t adequately possible. The center of gravity is behind the center of the knee in most cases, and the foot has complete contact with the ground. In that position, the force of the M. quadriceps is strong enough to rupture the ACL. In that position, the hamstrings have an unfavorable arm of lever to protect the ACL.
In alpine skiing injury the mechanisms have also been identified. Most ACL ruptures in skiing occur while the knee is flexed maximally and the center of gravity is behind the knee while the lower leg is internally rotated. In the literature, this mechanism is called the “phantom foot mechanism” [8].
24.2.3 Prevention
Motion analyses reveal women show a straighter landing position after a jump compared with men. The female knee and the hip joint show lower flexion but more valgus position during the landing after a jump. From these analyses, different prevention strategies have been developed in order to reduce incidence of ACL rupture in sports [4, 11, 16, 22, 24]. These prevention strategies might be divided as follows:
1.
Education about injury mechanism and modification of dangerous movement patterns
2.
Hamstring and hip rotator training
3.
Training of proprioception
4.
Jump exercises under supervision
24.2.4 Diagnostics
Most ACL ruptures do not show external signs of injury [26]. Acute ACL ruptures mostly present an extensive hemarthrosis. A puncture of this effusion, however, is only necessary if there is painful tension from the capsule.
The anterior drawer test is a classical test that provides information about anterior instability. Unfortunately, sensitivity of this test in acute ACL injuries is low because of the effect of the hamstrings. The Lachman test is known to be more sensitive (drawer test in 20–30° of flexion that reduces the lever arm of the hamstrings). In case of acute anterior instabilities, the part of positive Lachman test ranges from 78 to 99 % in contrast to the anterior drawer signs with 22–70 % [13]. The Lachman test can be quantified using the KT-1000 Arthrometer. The quantitative Lachman test might be useful for scientific purposes but also for the diagnosis of partial ruptures (Fig. 24.3).


Fig. 24.3
Lachman test in 20° of flexion
In daily activities or in sports, patients mainly feel unstable when the knee shows light flexion (20–30°) and the foot is fixed in light internal rotation. This mechanism can be evaluated with dynamic anterior subluxation tests, such as pivot shift phenomenon. The pivot shift phenomenon is the most popular dynamic subluxation test. The examiner holds the leg in valgus with internally rotated foot. This produces an anterior subluxation of the lateral tibia plateau. When the knee is flexed, the iliotibial tract reduces the lateral tibia plateau at approximately 30° of flexion. This reduction is visible or palpable as a clicking phenomenon. Other well-known subluxation tests are the Losse test, the Slocum sign, or the jerk test.
Clinical studies revealed that a positive pivot shift test after ACL reconstruction may be associated with poor clinical outcome.
On plain X-rays, the ACL cannot be seen. However, an anterolateral tibial plateau fracture (Segond fragment) is considered to be pathognomonical for an ACL injury. The same is true for the anterior impression fracture of the lateral femoral condyle.
The MRI is a sensitive method to make a diagnosis of ligament injuries and their concomitant injuries. The sensitivity of MRI to identify an ACL lesion ranges from 92 to 100 %, its specificity is 85–100 % [13, 29, 31, 33]. Direct findings of an ACL injury such as disruption or the lack of a ligament signal can be differentiated from indirect signs such as effusion or bone bruises of the lateral femoral condyle or at the posterior tibial plateau. The bone bruise pattern seen in MRI can give important information regarding severity and time from trauma to MRI; this might be important for legal reasons. The MRI does not allow a dynamic functional examination. This is the most important disadvantage of this method. Therefore, the findings in MRI must always be interpreted in relation to the findings of clinical tests (Fig. 24.4).
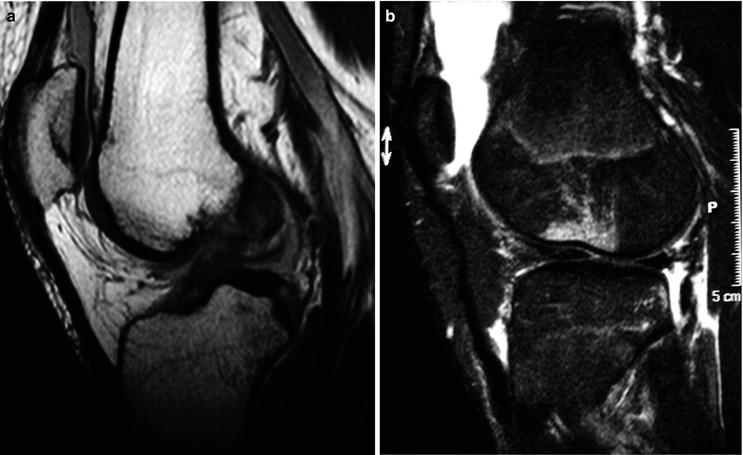
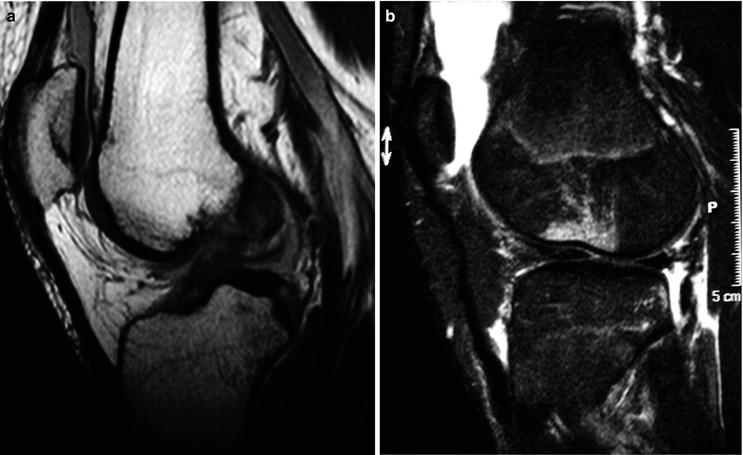
Fig. 24.4
(a) MRI showing a proximal rupture of the ACL. (b) Indirect signs of an ACL rupture: Anterolateral impression fracture of the lateral femoral condyle and posterior bone bruise at the lateral tibia plateau
Computer tomography (CT) should be performed in case of suspicion of an associated tibia plateau fracture. After surgery, the CT scan can provide adequate information about tunnel placement. This method is helpful in case of failed ACL reconstruction to plan revision surgery. It provides information about the width of the tunnel. The three-dimensional CT-scan reconstructions allow a precise identification of the tunnel positions (Fig. 24.5).
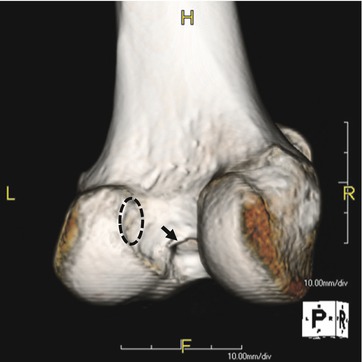
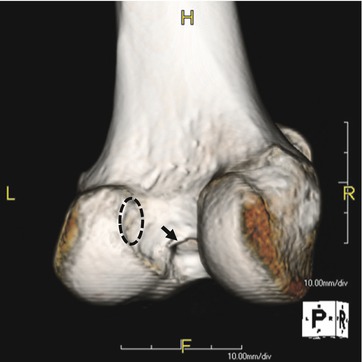
Fig. 24.5
CT scan showing an anterior ACL tunnel at the roof of the intercondylar fossa. The dotted circle shows the anatomical position of the femoral ACL insertion. The arrow shows the malpositioned ACL tunnel at the roof of the intercondylar fossa.
24.2.5 Partial ACL Ruptures
The incidence of partial ACL ruptures has been the subject of controversy for a long time [25]. In the meantime, isolated ruptures of the PL and the AM bundle have been described [25]. The rupture of the PL bundle is supposed to occur close to extension; the isolated rupture of the AM occurs in flexed knee position. The diagnosis of isolated ruptures of only one bundle of ACL is difficult. Clinical findings, findings of imaging methods, and arthroscopical findings must be well interpreted. In clinical examination, an isolated rupture of PL may cause a positive pivot shift phenomenon. In most cases of isolated AM rupture, however, the pivot shift sign is negative.
Rupture of the AM may lead to an extension deficit if fibers of the ruptured bundle impinge at the anterior edge of the notch. If there is only a short time between the accident and the MRI procedure, the MRI may reveal edema or a gap in the fibers’ continuity in the correlative bundle. The arthroscopical examination and evaluation of chronic PL ruptures are complicated because of relaxation of the PL bundle in flexion. Only acute trauma signs such as hematoma and a discontinuity of PL fibers can give a hint of an isolated PL rupture.
24.2.6 Natural History After ACL Rupture
The loss of ACL may lead to anterior and rotational instability [5]. This instability may impair the patient directly (instability, giving way). In the long-term, an anterior instability can cause secondary damage to the knee joint. A chronic anterior subluxation raises the applied load on the posterior parts of the tibia plateau and the posterior horns of the menisci. The pathological loading on the posterior parts of the tibia plateau and the menisci may be cause for a posteromedial osteoarthritis. Patients with secondary posttraumatic osteoarthritis and ACL deficiency are 15–20 years younger compared to the patients with primary osteoarthritis [28]. This was described by Daniel et al. [5] and was called the “ACL injury cascade.” However, the ACL injury cascade model describes the onset of a posttraumatic gonarthrosis incompletely. Initial injuries (concomitant ligament injuries, damage of cartilage and menisci) are ignored, although they have an important influence on the postoperative results after ACL reconstruction. Anterior subluxation of the lateral tibia plateau may cause lesions of the lateral meniscus such as root tears and cartilage damage (Fig. 24.6). Therefore, we should better speak about the “knee trauma cascade” [27] instead of the ACL injury cascade (Fig. 24.7). Initial lesions of menisci and cartilage may explain findings in clinical studies reporting radiological signs of osteoarthritis after ACL reconstruction. ACL reconstruction can only treat anterior instability but not associated meniscus and cartilage damage.
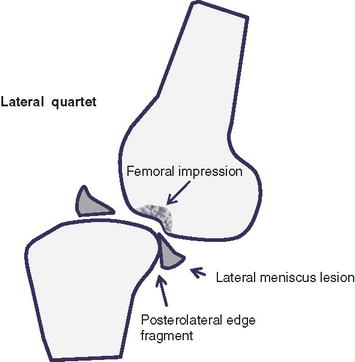
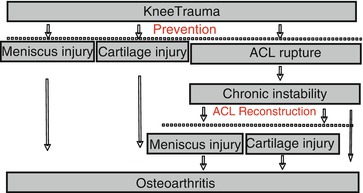
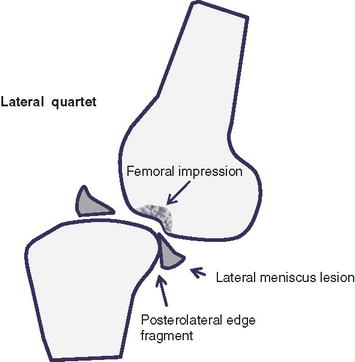
Fig. 24.6
Schematic drawing of the injury mechanism of associated lateral injuries. The so-called “lateral quartet” is the rupture of the ACL, impression fracture of the lateral femoral condyle, posterior bone bruise at the lateral tibia plateau, and injury of the lateral meniscus
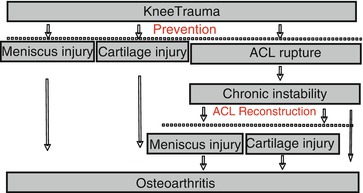
Fig. 24.7
Knee injury cascade
24.2.7 Indication for ACL Reconstruction
A prospective study revealed that reconstruction of the ACL may prevent the onset of secondary intraarticular damage and of degenerative joint lesions in patients with symptomatic instability and risk factors [12]. Risk factors are high activity level, giving way phenomena during sports or daily life activities, and a positive pivoting. Some patients may cope with an unstable knee [7]. This ability is independent from activity level. Different criteria can be used to identify such patients: one leg jump test >80 % of the contralateral leg, more than one giving way phenomenon, impairment of daily activities of less than 80 % due to knee injury and a knee function score < 60 % [7].
The indication for ACL reconstruction remains an individual decision. Patients and athletes showing a symptomatic instability who do not want do modify their activity level are candidates for ACL reconstruction. A concomitant bucket-handle tear of menisci is another indication for ACL reconstruction because of the high rate of menisci re-ruptures in unstable knees. The same is true for secondary intraarticular lesions due to a symptomatic chronic instability. An age over 40 years is not a contraindication for ACL reconstruction. However, in patients older than 40 years, the prevention of secondary osteoarthritis is less important. In case of concomitant presence of osteoarthritis and varus knee, the indication of high tibial osteotomy (HTO) should be considered. In case of persisting instability, the HTO can be combined with the ACL reconstruction in a one- or two-step procedure.
In children and adolescents with open epiphysis, the indication of ACL reconstruction is still under discussion. Prospective studies revealed a high incidence of secondary posttraumatic lesions in children with a persisting anterior instability due to ACL deficiency [1]. A newer study from Scandinavia showed that some children may develop strategies to cope the anterior instability [14].
If there is an indication for ACL reconstruction, the risk of damage to the epiphysis using a tendon graft without a bone block is very low.
24.2.8 Reconstruction of the ACL
Today, the replacement of the ACL with the use of autologous tendon grafts is the gold standard of operative treatment. The most frequently used tendon grafts are the semitendinosus tendon and the patella tendon. Many studies compared both grafts. The differences in long-term stability were small [10]. The donor site morbidity after harvesting the patella tendon is supposed to be higher than in cases of harvesting the semitendinosus tendon. A further graft option is the quadriceps tendon.
Experience from revision surgery after ACL reconstruction showed that the main reason for graft failure is incorrect placement of bone tunnels. The function of the ACL can only be restored if the bone tunnels match the femoral and tibial insertion zones. The technique, respecting the anatomic landmarks for ACL reconstruction, is called “anatomical ACL reconstruction” [20, 21].
The complete femoral insertion zone of the ACL is difficult to visualize from the classical anterolateral arthroscopy portal. An adequate overview on the wall of the lateral femur condyle is only possible using the anteromedial portal (Figs. 24.8 and 24.9).
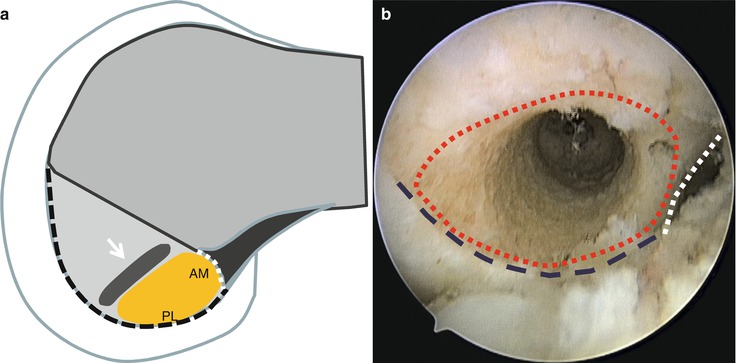
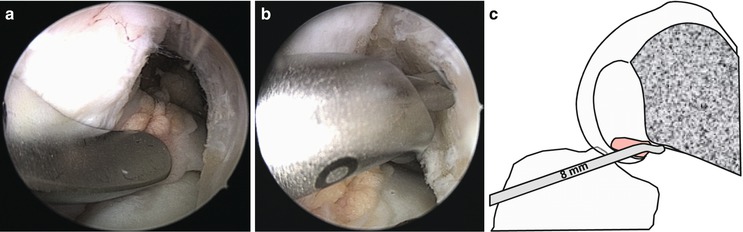
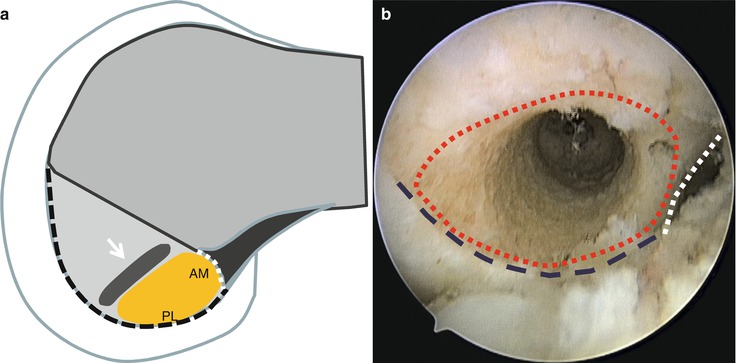
Fig. 24.8
Anatomical ACL reconstruction (a) Schematic drawing of the femoral insertion of the ACL (white dotted line: intercondylar line, black dotted line: cartilage border). The white arrow indicates the resident’s ridge. (b) Anatomical femoral bone tunnel for ACL reconstruction (view from the medial portal) white dotted line: intercondylar line, blue dotted line: cartilage border, red dotted line: anatomical insertion zone of the ACL
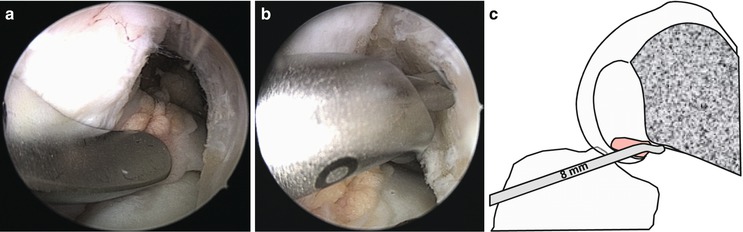
Fig. 24.9




Anatomical femoral tunnel placement via the medial portal. (a) Insertion of the medial portal aimer via the medial portal (Karl Storz, Germany). (b) The hook of the offset guide is placed behind the Facies poplitea. (c) Schematic drawing showing the offset guide in place
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








