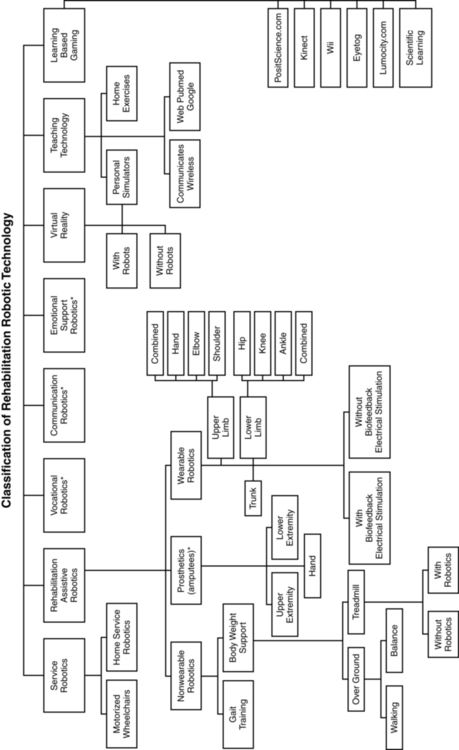
KATIE BYL, PhD, NANCY N. BYL, PT, MPH, PhD, FAPTA, MARTEN BYL, PhD, BRADLEY W. STOCKERT, PT, PhD, SEBASTIAN SOVERO, MS, CLAYTON D. GABLE, PT, PhD and DARCY A. UMPHRED, PT, PhD, FAPTA After reading this chapter the student or therapist will be able to: 1. Summarize the need, demand and principles for integrating advanced robotic technology in neurological rehabilitation. 2. Define common terminology used in the field of rehabilitation robotics and technology. 3. Classify the different types of advanced technology used in neurorehabilitation. a. Rehabilitation robots and assistive technology including: i. Service robots for movement ii. Service robots for physical assistance and indoor and outdoor navigation iii. Nonwearable robotic assistive device for mobility, unweighting, and object manipulation iv. Wearable robotic assistive device for upper-limb object manipulation v. Wearable robotic assistive device for lower-limb mobility and gait training vi. Communication robotics to enable interpersonal interaction vii. Interactive entertainment robotics for companionship and emotional support b. Advanced clinical technology including: i. Virtual reality training systems for improved neural recovery of upper- and lower-limb function ii. Computerized learning-based gaming systems for home training of individuals with physical disabilities and memory impairments iii. Computerized patient simulators for teaching clinical diagnoses and intervention strategies to medical professionals iv. Computer technology for teaching home exercise programs to patients 4. Use the guidelines for integrating robotics and assistive technology into a patient’s rehabilitation program. 5. Summarize the challenges and basic engineering principles involved in creating rehabilitation robotics and interfacing with advanced technology to help individuals to design: a. Robots that operate independently b. Controllers, actuators, and sensors required for service and assistive rehabilitation robots c. Human interfaces (physical, sensory physical, cognitive, and brain machine) d. User-friendly interfaces and controllers to maximize kinematics (e.g., force, velocity, timing) e. Rehabilitation robotics based on the materials and control technology currently available f. Safe robotics for rehabilitation 6. Discuss the benefits of performing a cost-effectiveness analysis when considering the application of robotic technology in rehabilitation. 7. Describe the challenges of commercializing robotic devices. 8. Discuss the future of advanced technology and rehabilitation. The objective of rehabilitation technology is to empower clinicians and individuals to take responsibility and control of the environment, facilitate physical and cognitive recovery, and comply with learning-based practice to drive neural adaptation and neural reorganization. The principles underlying technology and rehabilitation are summarized in Box 38-1. Since the early 1990s, medical science has been able to minimize damage to the nervous system postinjury. It is known that the central nervous system (CNS) possesses the potential for spontaneous healing and recovery. Learning-based sensory and motor training can be used to drive recovery of function. Rehabilitation robotics are a logical addition to supervised, one-on-one therapeutic interventions.1–9 Robotic technology can provide service, unweighting, passive assistance, active assistance, variable and on-demand assistance, or a combination of service and assistance.10 Computerized and robotic technology provides the foundation for patients to practice and attend to purposeful, goal-oriented, progressive tasks spaced over time. This technology can also minimize the risk of injury during retraining. Robotic interfaces, actuators, and controllers can convert sensory, physical, and cognitive signals to control robots, permit perception of spatial relationships, mobilize individuals in space, assist in object manipulation, provide emotional support, and allow individuals to call for help and communicate with others. In addition, through creative virtual training environments and gaming technology, patients can improve memory, motor skills, and movement quality. In addition, patient simulators can help medical professionals learn diagnostic processes, treatment interventions, and manual techniques. Computer-assisted technology can also improve our ability to teach home exercise programs to patients. Over the next 10 years, robotic technology will expand the opportunities for clinicians to assist patients to achieve maximum independence and quality of life with less dependence on others. The idea of interfacing technology with rehabilitation was introduced into practice by George J. Kelin in the 1940s. Kelin was a productive inventor from Canada who invented the power wheelchair for patients with quadriplegia, the microsurgical staple gun, and a wide range of industrial gearing systems. He also contributed to internationally important innovations in aviation and space technology. During the early 1970s, a new field emerged known as mechatronics, which combines mechanical, electrical, and control engineering design principles to produce a diverse range of useful practical devices.11,12 The science of biomechatronics then developed as a unique engineering discipline responsible for integrating neuromusculoskeletal appliances with biological systems to control and facilitate human-machine interactions as well as developing interfaces, sensors, actuators, and energy supplies to create functional devices for human use.13 The first conference on rehabilitation robotics was held in 1990. There are now multiple conferences each year on rehabilitation robotics. In 1999 the Robotics and Automation Society created the Rehabilitation Robotics Technical Committee to improve definitions and understanding about rehabilitation and assistive robotics.14 The scope of this technical committee has been recently specified as rehabilitation and assistive robotics. This modification is the direct outcome of the scientific progress and maturity reached in this broad research area. The goal of rehabilitation robotics is to investigate the application of robotics to therapeutic procedures for achieving the best possible motor, cognitive, and functional recovery for persons with impairments associated with aging, disease, or trauma (e.g., stroke, neuromotor disorders, brain trauma, orthopedic trauma, cognitive disease). Some clinicians have been skeptical of robotics in rehabilitation. Some health care providers worry that robots will replace therapists; others worry that robots are unsafe.8 However, researchers have persisted in developing innovative hardware, new control strategies, improved compliance, and feed-forward and adaptive control systems, as well as computerized modeling. In addition, new assistive, wearable robotic arm devices have been developed (e.g., MIT-Manus, the MIME, the ARM, and the iARM) to more carefully outline and address the engineering challenges related to what the robot can do, the logical physical targets for active assistance, and the joints and the types of movements that can safely be assisted. The field of rehabilitation robotics is still considered to be in its infancy. However, with the increasing demand for effective rehabilitative strategies, many new and exciting innovations are being developed. There are many robotic systems in various stages of research and development, but only a few are commercially available. Improvements in engineering, materials, human physical interfaces, software, and robotic designs will require constant analysis and adjustment in the future. It is projected that the market for personal robotic devices will be worth $15 billion by the year 2015.15,16 The challenges of robotic engineering are broad. Clinicians will need to participate in research to help document cost-effective outcomes as well as to develop efficient screening criteria to match patient needs with available robotic devices. One of these challenges will be to bridge the gap between the mechanical attributes of robotic sensors, actuators, controls, microprocessors, force, velocity, friction, unweighting, pressure tolerance, software design, and flexibility with the human limb, brain, and nervous system. Important issues related to safety, materials, technology, and the quality of matching machine and human movements must constantly be considered. These engineering issues are discussed later in this chapter. There is a variety of ways to classify computerized technology for rehabilitation. For this chapter, we will group robotic technology first in terms of how robotics are used with or by the client relative to rehabilitation. This classification system is summarized in Figure 38-1 and Box 38-2. Rehabilitation technology can be further classified by a variety of variables summarized in Box 38-3. Rehabilitation robotics can also be classified by type of interface used. Some classification systems classify technology by multiple parameters. Service robots usually focus on task performance, movement assistance, and stability. These devices can be fixed, can be movable, or can be attached to a wheelchair (Box 38-4). Assistive robotic devices help patients perform a task with direct or indirect assistance. Some of the assistive robotics are nonwearable but assist through unweighting or movement assistance (Box 38-5). Wearable robotics are specifically designed to be worn by patients to assist movements. These are designed for the upper or lower limb (Box 38-6). There are some new assistive training devices for the spine such as the Valedo Shape, Valedo Motion, and Hocoma devices (Figure 38-2). Prosthetic devices help patients maintain function despite the loss of a limb. Vocational robotics can enhance performance at work either in terms of repetitive motions or high-force task production that would otherwise be dangerous to humans. Communication robotic devices are designed to improve communication potential for subjects who cannot adequately speak or hear. Emotional support robotics are designed to provide emotional support for isolated individuals at home. VR training technology (with and without robotics) provides the opportunity to simulate simple and complex environmental and clinical situations to facilitate learning (Box 38-7). Game-oriented computerized learning systems are currently popular for fun and recreation, but they can also facilitate memory as well as sensory and motor skill development. Finally, computerized technology can also enhance teaching home exercises to patients. In this chapter, we will not address prosthetics for amputees, vocational robotics, communication robotics, emotional support robotics, or socially assistive devices,17,18 as these areas are considered specialty oriented and may or may not be included in traditional neurorehabilitation programs coordinated by physical or occupational therapists. However, information about the impact of the sound of the robot voice on patient motivation and compliance may be relevant to effectiveness. It is also important to acknowledge there are a number of motorized chairs, lifts, and walkers available that can be used to transition a patient from sitting to standing, or provide unweighting while walking or working on balance. Examples can be found in Box 38-8. Many of these systems are electromechanical systems controlled by the patient or the therapist. These devices are not usually programmable and are not classified as “rehabilitation robotics” or “advanced technology.” However, these types of devices are very beneficial for helping patients maintain walking and training to improve safety and quality of gait at home and with supervision. It is important for therapists to be sure these types of assistive devices have been integrated into a patient’s rehabilitation program and at home before recommending more sophisticated technology. Service robotics assist individuals with severe disabilities. Most commonly, the robot performs everyday activities (e.g., assisting with eating, drinking, object replacing, ambulating). There are three main types of schemes: desktop-mounted robots, wheelchair-mounted robots, and mobile autonomous robots. In general, these robots are used in the home, are interconnected to a variety of control systems, and are programmed to the environment and consequently are not very portable.19–21 Several examples of service robotics are described in Box 38-9.22–30 A major issue is patient control options for service robotic devices. For example, through the use of headpieces on robotic devices, information can be detected from flexion and extension, rotation, and side bending of the head to operate wheelchairs, TV sets, telephones, doors, and security systems. There are also some new interfaces that are sensitive to facial movements and optoelectronic detection of light-reflective head movements.31 Other interfaces are sensitive to eye movements or use voice recognition, brain control,32,33 and gesture recognition.34 These interfaces not only may allow control of the robot but also may be applied to move a limb or perform a task. There is a variety of nonwearable assistive robotic devices. Some of these nonwearable assistive robotic devices are summarized in Box 38-10.35–43 This group of robotic devices primarily includes powered wheelchairs with autonomous intelligence, body-weight–supported mobile walking aids, robots for body support with indoor and outdoor navigation, hands-off service robotic devices, and body-weight–supported treadmill systems (BWSTSs) with and without robotics.37,41–45
Integrating technology into clinical practice in neurological rehabilitation*
Introduction to the application of robotics and technology in rehabilitation
General overview
History supporting the use of technology in neurological rehabilitation
Classification of rehabilitation robots
General principles
Description of robotic systems by type
Service robotic systems that provide movement assistance
Assistive robotics
Nonwearable assistive robotic devices.
Types of nonwearable assistive robotic devices.




































 ed (
ed ( pper •imb)
pper •imb)















 ’ Go wa•ker
’ Go wa•ker






