CHAPTER 9 Instability of the Ankle and Subtalar Joints
Ankle sprains are the most common sports-related injuries, and they account for almost 10% of emergency department visits. Most ankle sprains are inversion-type sprains that injure the lateral ankle ligaments. Chronic lateral ankle instability develops in 20% to 30% of patients after acute ankle sprains despite adequate nonoperative treatment.1 The cause of chronic lateral ankle instability after ankle injury is not well understood and is probably multifactorial. Symptoms may result from inadequately healed torn ligaments or ligaments that have healed in a stretched manner.2 Generalized hyperlaxity, strength and proprioception deficits are likely contributing factors.
ANKLE INSTABILITY
Anatomy and Physiology
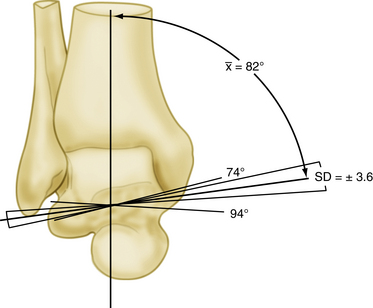
Stability of the ankle joint depends on the contributions of bony architecture, ligamentous attachments, and the dynamic stability provided by muscles around the ankle.3 The ankle is a composite joint that includes the distal tibiofibular syndesmosis and a diarthrodial mortise between the distal tibia and fibula and the talus. The subtalar joint provides sagittal rotation about a single oblique axis, from the neck of the talus to the lateral wall of the calcaneus. In the coronal plane, the axis of the ankle runs medial cephalad to lateral caudad, with a mean angulation of 82 ± 4 degrees in relation to the tibia (Fig. 9-1).
The ankle joint axis tends to change throughout the functional arc range of motion from dorsiflexion to plantar flexion. The distal fibula moves distally with weight bearing, deepening the mortise and increasing ankle stability. The talus is not as well contained by the mortise during plantar flexion compared with dorsiflexion, because the talus is wider anteriorly than posteriorly. The dorsal surface of the talus has a slight longitudinal groove that corresponds to a longitudinal ridge on the tibial plafond. The ridge and groove help to confer transverse plane stability to the tibiotalar joint. The distal fibula gives attachment to the lateral ligaments of the ankle joint, and its posterior aspect is grooved to accept the tendons of the peroneus longus and peroneus brevis muscles.4 Bony anatomic variations may contribute to increased ankle instability. For example, Scranton and colleagues showed that the fibula is located more posterior in patients with instability.5 One study compared hindfoot varus measurements on computed tomography (CT) scans of patients with lateral ankle instability to those of patients without instability and found a statistically significant increased amount of varus in patients with instability.6
The ankle ligaments provide supplemental stability to the ankle and also contribute to hindfoot stability. Ligaments of the ankle joint include the syndesmotic ligaments, the deltoid ligament complex, and the lateral collateral ligaments. The syndesmotic ligaments include the anterior inferior and posterior inferior tibiofibular ligaments and the strong interosseous ligament.
The deltoid ligament is formed by four to six main ligaments on the medial side. Four of these are always constant; from anterior to posterior, they are the anterior tibiotalar ligament (ATTL), the tibionavicular ligament (TNL), the calcaneotibial ligament (CTL), and the posterior tibiotalar ligament (PTTL). Occasionally, calcaneonavicular and tibiospring ligaments can be part of the deltoid ligament. The deltoid ligament includes superficial and deep parts. The superficial ligaments cross two joints, namely the ankle and the subtalar joints. The deep ligaments cross only the ankle joint, though the demarcation is not always absolutely clear.3,7 The deltoid ligament is the primary restraint against pronation and abduction of the talus, with the superficial and deep components equally effective.7
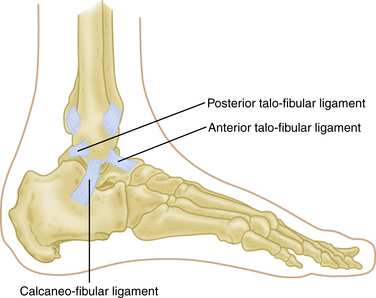
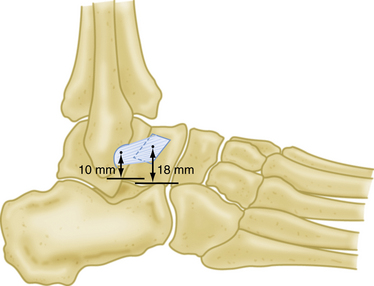
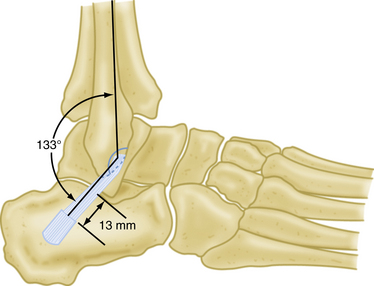
The lateral ankle joint ligamentous complex provides primary restraint to inversion and consists primarily of three structures: the anterior talofibular ligament (ATFL), the calcaneofibular ligament (CFL), and the posterior talofibular ligament (PTFL) (Fig. 9-2). Intimate knowledge of the anatomy is paramount to the success of surgical reconstruction. The ATFL, which is possibly a thickening of the joint capsule, is the most anterior structure. It averages about 24.8 mm in length and 7 mm in width and is the weakest and most easily injured of the ankle ligaments (Fig. 9-3). It originates about 10 mm proximal to the tip of the fibula and inserts on the lateral aspect of the talus, on average 18 mm superior to the subtalar joint.3,7,8 The ATFL courses obliquely from posterolateral to anteromedial with respect to the tibiotalar joint. It resists internal rotation of the talus as well as anterior translation. The CFL is a round, cordlike, extracapsular structure that originates from the inferior medial surface of the distal fibula. It extends posteroinferiorly, deep to the peroneal tendons, and attaches on a small tubercle on the lateral calcaneal surface, on average 13 mm inferior to the subtalar joint and posterior to the long axis of the fibula.3 It is about 35.8 mm long and 5.3 mm wide (Fig. 9-4). The CFL is vertical and coplanar with the fibula at 10 to 20 degrees of ankle dorsiflexion. In that position, it resists inversion and becomes the primary ankle stabilizer and a secondary subtalar joint stabilizer.8,9
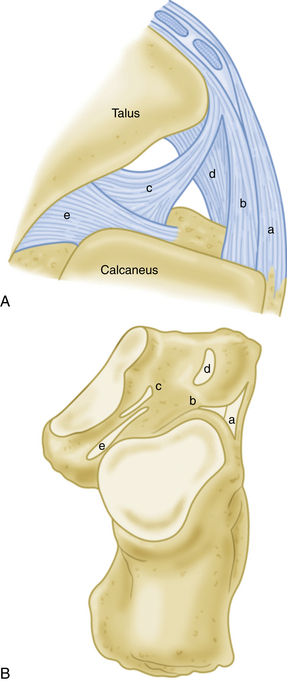
Isolated rupture of the PTFL is rare because it is the strongest and least vulnerable of the lateral ankle ligaments. The PTFL originates from the posterior portion of the distal fibula and inserts onto the lateral tubercle of talus posteriorly. It may be injured in combination with rupture of the ATFL and CFL in severe ankle sprains and ankle dislocations.7,10 The lateral subtalar joint is further stabilized by the interosseous talocalcaneal ligament (ITCL), the cervical ligament, the inferior extensor retinaculum, and the lateral talocalcaneal ligament (LTCL) (Fig. 9-5). In a biomechanical study, Tochigi and Amendola showed the ITCL to be the main stabilizer of the subtalar joint.11
The musculotendinous units that cross the ankle joint provide secondary or dynamic stability to the ankle and hindfoot. The most important of these are the laterally positioned peroneal tendons, which are the primary evertors of the ankle12; the tibialis posterior tendon; and the toe flexors medially. In a cadaveric study, Hatch and Labib demonstrated that the peroneal tendons, along with the superior peroneal retinaculum (SPR), provide static resistance to anterior talar displacement with the ankle in neutral position. In that study, sectioning of the retinaculum and removal of the tendons caused an average increase of 15% in anterior ankle displacement, indicating that the peroneal tendons may impart some static stability to the ankle joint.13 This finding may explain the increased incidence of peroneal tendon problems in patients with chronic ankle instability.
Mechanisms of Chronic Lateral Ankle Instability
When the ankle is dorsiflexed, the talus fits snuggly into the mortise and the ATFL is loose, but when the foot is plantar flexed, the ATFL becomes vertical and serves as the primary stabilizing structure of the ankle in inversion. Injury to the ATFL occurs with inversion of a plantar-flexed ankle with or without internal rotation. Commonly, the CFL is injured in combination with injury to the ATFL. Injures to the CFL occur with inversion of a dorsiflexed ankle. Subtalar ligament injury may be in continuum with a CFL injury. It has been shown that rupture of the ATFL occurs as an isolated injury in 50% to 75% of cases. With increasing force, the CFL also is ruptured. A rupture of the ATFL and the CFL occurs in 15% to 25% of cases. Isolated rupture of the CFL happens in approximately 1% of patients, and injury to the PTFL is extremely rare.8–10,14 Isolated ligament injuries of the deltoid ligament are infrequent.
Chronic lateral ankle instability results when the injured ligaments do not regain the mechanical integrity necessary to stabilize the ankle against physiologic stress. Possible risk factors for ankle instability that have been implicated in the literature include (1) environmental factors, such as the condition of the playing field, the level of neuromuscular training, the position an athlete plays, and the available equipment15 and (2) a patient’s unique anatomy, including variations in ankle anatomy, multiligamentous laxity, limitation of ankle range of motion, a history of recurrent ankle sprain, diminished muscle strength, poor postural control and proprioception, and delayed muscle reaction time.16 A varus tibial plafond alignment, a varus hindfoot alignment, and a posterior fibular position have also been proposed as possible predisposing factors in chronic ankle instability.17
Chronic lateral instability of the ankle usually manifests as a mechanical or a functional instability. Mechanical instability is objective abnormal motion of the talus relative to the ankle mortise, as measured on standardized stress radiographs or by clinical measurement of an anterior drawer sign or varus tilt.7,15 Functional instability is manifested as a symptomatic feeling of the ankle’s repeatedly giving way, combined with pain and difficulty walking on uneven terrain. Functional instability is most likely caused by increased laxity of the injured ligaments, inhibition of proprioceptive function, peroneal muscle weakness, or a combination of these factors.7,15 Some patients manifest functional instability without the mechanical components or vice-versa.
PATIENT EVALUATION
History and Physical Examination
Physical examination should include an evaluation of gait, generalized laxity, and hindfoot varus malalignment (Fig. 9-6). Proprioception testing is done by asking the patient to balance on the affected foot (single leg balance) or to perform a single leg jump-landing test with comparison to the contralateral side.18 Local ankle examination is often positive for tenderness to palpation over the affected ligaments with guarding, apprehension, and peroneal weakness.19
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree