Chapter 129 Instability in Total Knee Arthroplasty
It has been said that total knee arthroplasty is a soft tissue procedure. Creating rectangular gaps and balancing the soft tissue envelope around the knee are recognized as prerequisites for successful and durable outcomes following total knee arthroplasty. Ligamentous instability is increasingly recognized as a common mode of prosthetic knee failure. Reports in the literature suggest that instability is a reason for 10% to 22% of total knee revisions.* Early failure in the first 5 years following the index arthroplasty is common when stability is not achieved,6 and instability is second only to infection as the cause of revision surgery less than 2 years after the index operation.35
The clinical presentation of instability is variable and the symptoms must be clarified. Symptoms may be apparent immediately after the index arthroplasty or may manifest late and largely depend on the underlying cause of instability. It has been noted that the patient’s report of “instability” does not make the diagnosis.37 Buckling and giving way can have many causes, including pain, fixed flexion contracture of the knee, quadriceps weakness, and patellar dislocation.37 Whereas gross instability may present with frank dislocation, subtle mechanical instability often presents with vague complaints of anterior knee pain, recurrent effusions, soft tissue tenderness to palpation, and above average range of motion.29 Patients with subtle instability may also note difficulty in starting ambulation after being seated.
An accurate history is important in determining the factors that led to failure. Considerations include obtaining information on the original diagnosis that precipitated the knee replacement, any preoperative deformity or contracture, previous knee procedures, type of prosthesis, the specifics of the operative technique for knee replacement, the postoperative rehabilitation program, and any trauma to the knee after surgery.37,43,44 Extra-articular deformity, neuromuscular pathology, and large surgical corrections with ligament releases all have been cited as risk factors that predispose to postoperative instability.37 Obesity has also been reported as a risk factor for intraoperative collateral ligament injury and complicates both intraoperative and postoperative assessment of soft tissue balance.42
The patient’s complaints must be carefully reconciled with objective physical examination findings. The physical examination requires assessment of generalized ligamentous laxity and muscle strength. Observation of gait may reveal a varus or valgus thrust and may suggest coronal plane instability. The knee should be examined for anteroposterior and varus/valgus stability and symmetry in extension, 30 degrees of flexion, and 90 degrees of flexion. Subtle instability may be challenging to appreciate if the patient is guarding. Flexion laxity is often most evident when an anterior or posterior drawer test is performed with the patient sitting and the knee flexed to 90 degrees.29 The precise amount of laxity and translation that is considered pathologic has not been defined. However, reproduction of a patient’s symptoms during laxity testing is at least suggestive of a pathologic link. An above average range of motion may be observed commonly in an unstable knee replacement.29 The integrity of the extensor mechanism should be assessed as a potential cause of global instability. Aspiration of synovial fluid from the knee may reveal hemarthrosis with elevated red blood cell counts.32
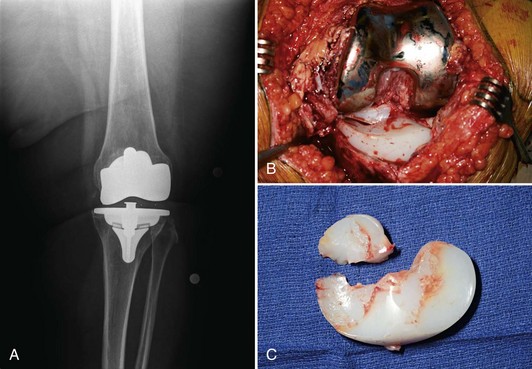
A complete set of radiographs, including full-length weight-bearing views, should be obtained. The size and position of the components should be assessed and the mechanical and anatomic axes determined. Weight-bearing views may stress and accentuate the instability (Fig. 129-1). Apparent instability may be readily explained by component wear or loosening, implant breakage, fracture, and bone loss (Fig. 129-2).37 A large modular tibial insert often suggests problems with intraoperative balancing. Ligament attenuation may have occurred as the result of component overhang. Stress radiographs may provide an objective way to diagnose prosthetic knee instability, although they are rarely used in our clinical practice.
Extension Instability: Symmetrical
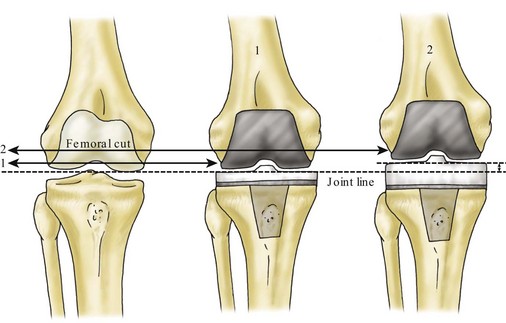
Symmetrical extension instability occurs when medial and lateral collateral ligament tensions are lax in extension. In this relatively rare situation, the combined thickness of the components is not sufficient to restore physiologic tension to the ligaments in extension only; this has been termed instability due to bone resection.43,44 Excessive bone removal from the femur will selectively increase the extension gap without altering the flexion gap; this is termed gap inequality.17
Management of isolated symmetrical extension instability caused by excessive femoral bone loss can be challenging. A thicker tibial insert will not solve the problem. Increasing the tibial insert thickness will elevate the joint line and excessively tighten the flexion space (Fig. 129-3).37,44 Elevation of the joint line can adversely affect knee kinematics (particularly the patellofemoral joint) and lead to worse clinical outcomes.31 Distal femoral augments should be used to move the joint line distally. Such augments are available in most contemporary revision total knee systems.
Extension Instability: Asymmetrical
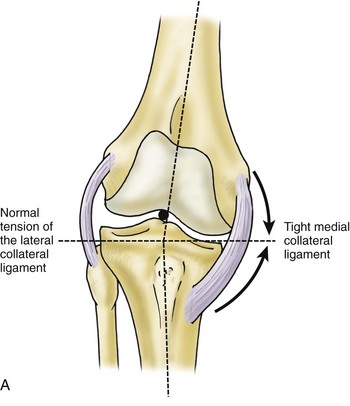
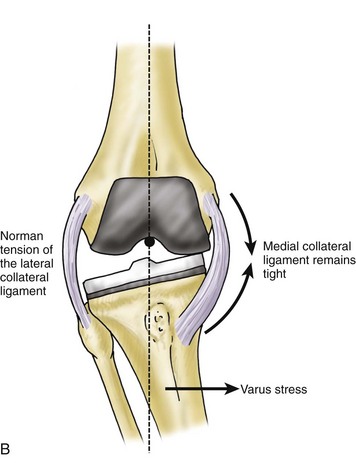
Asymmetrical extension instability is much more common than symmetrical extension instability.30 This situation is typically related to preoperative angular deformity of the knee and is caused by persistent or iatrogenic ligamentous asymmetry after the knee is replaced (Fig. 129-4).29,30,37,44 Fear of creating iatrogenic ligamentous instability in the opposite direction is a frequent reason for incomplete ligament balancing and undercorrection of deformity.
In the case of a varus knee, concerns about over-releasing the medial collateral ligament can leave the knee tight on the medial side—a situation exacerbated by leaving the limb alignment in varus.29,37,44 Excessive medial collateral ligament tension and varus malalignment can result in medial overload with polyethylene wear and further stretching out of the lateral ligaments.29,37,44 Recurrence of deformity may occur postoperatively. An appropriate medial release as originally described by Insall and associates should be performed when necessary.15 A thicker tibial insert may be required following medial release to restore tension in the collateral ligaments. Lateral collateral ligament advancement can be considered if complete medial release fails to balance the knee.18
Asymmetrical extension instability may result from undercorrection of a valgus knee deformity. Failure to appropriately release contracted lateral tissues will leave laxity or redundancy in the medial collateral ligament. The medial collateral ligament has no ability to tighten over time, and the valgus deformity will recur.37,43 Minimal laxity of the medial collateral ligament should therefore be accepted. Sequential lateral ligament release approaches12,15 have been associated with frequent over-release of the lateral soft tissues.27 As a result, the “pie-crust” multiple puncture technique has gained widespread use.4,27 To check for an over-released lateral side, the trials can be inserted and the knee placed in a “figure-of-four” position (90 degrees of knee flexion while the surgeon holds the foot and allows the hip and knee to maximally externally rotate). If the post of a posterior stabilized insert subluxates from the femoral housing, a thicker or more constrained tibial insert should be used.4
Complete correction of severe valgus deformity incurs the risk of peroneal nerve stretch.5 Satisfactory results have been reported with intentional deformity undercorrection and the use of a varus/valgus constrained implant to compensate for residual medial collateral ligament laxity.5 This approach carries the theoretical concern that a constrained implant will impart additional stresses to the implant and fixation interfaces and should be reserved for elderly, lower demand patients.
Intraoperative iatrogenic collateral ligament injury can occur, most commonly when the proximal tibia is cut. Vigorous attempts to assess stability intraoperatively can lead to ligament stretch or rupture, typically of the medial collateral ligament. Surgical reapproximation of the ligament is the recommended approach.21 The hamstring tendons may be used to augment the repair, and a condylar constrained implant may be used to enhance stability.5,21 Postoperative bracing may help reduce stresses on the healing ligament.21
Flexion Instability: Symmetrical
Symmetrical flexion instability is likely under-reported as the diagnosis can be elusive. This distinct clinical entity can occur with both posterior stabilized and cruciate retaining designs and is characterized by painful subluxation of the tibia on the femur. This situation is often seen in patients in whom the total knee prosthesis is well aligned axially and well fixed.29 Manifestations of flexion instability differ depending on the cause of the problem and the implant design.
A large flexion gap may result from inadequate filling with the implant, often due to under-resection of the distal femur in an attempt to avoid elevating the joint line. In this scenario, the surgeon will typically preferentially balance the resulting tight extension gap at the expense of a loose flexion gap. With trials in place, the tibia should have less than 5 mm of anteroposterior translation when the knee is tested intraoperatively at 90 degrees of flexion with the patella reduced.30 The “figure-of-four” position, as described earlier, can be used to establish that the knee will not dislocate.
Dislocation of a posterior stabilized total knee arthroplasty is rare but dramatic, with a reported incidence between 0% and 0.5%.9,14,22 If the flexion gap is large enough, the cam mechanism may jump over the post, resulting in posterior dislocation of the tibia on the femur. Dislocation typically occurs with marked knee flexion plus a valgus or varus stress (such as occurs when crossing the legs to put on socks or shoes).8 At-risk patients include those who had correction of a large valgus deformity, particularly if they quickly regained knee flexion postoperatively.34 First-time dislocations should be treated with closed reduction, a trial of bracing, and avoidance of the activity that induced the dislocation, although severe laxity will often lead to repeated dislocations. Mobile-bearing designs may require open reduction.13 Recurrent dislocation may require revision with thicker polyethylene (if the extension space permits). A constrained condylar implant may be helpful but will not prevent repeat dislocation in the setting of continued gap imbalance (Fig. 129-5). The “Figure 4” maneuver can be used to assess correction of the instability.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree