Assessment by the means of questionnaire is not, of course, a new methodology, but the integration with functional and physical tests to form a holistic process is. The way in which the screening elements are integrated into the injury prevention process can have a large impact on the athletes involved. If athletes feel part of this process then they could take ownership and really fully commit to the measure that is ultimately proposed. If athletes are insufficiently involved then they might see the process and resultant programme as unnecessary and therefore not worthy of expending too much energy on. The other situation is where the athlete could learn too much and become de-motivated about their long-term future in the sport and as a result not commit. The latter two scenarios will mean that the practitioners plans may fail and the problems identified will probably arise with a negative effect on performance.
A more simplistic approach to questionnaires can also produce good results in reducing the amount of tests that an athlete needs to perform. The reduction of testing time is important in large squads as the amount of time the practitioner spends with the athlete reduces the amount of time the coach can spend working on sport-specific training. Therefore, the need to develop a useful tool to identify the members of the squad who do not need any further testing or those who can be dealt with in a reduced fashion is important. The process shown in Figure 2.2 indicates a simple pathway to group the squad into different levels of testing through a simple set of questions. This has been shown to be reliable in identifying conditions and more importantly not missing any problems. The questionnaire again needs to be administered by a practitioner to insure the validity of the answers (Berg-Rice et al. 2007).
Figure 2.2 Initial screening questions (Berg-Rice et al. 2007). Reproduced, with permission, from Berg-Rice, V.J., Conolly, V.L., Pritchard, A., Bergeron, A., & Mays, M.Z. (2007). Effectiveness of a screening tool to detect injuries furing army health care specialist training. Work, 29, 117–188, © 2007 IOS Press.
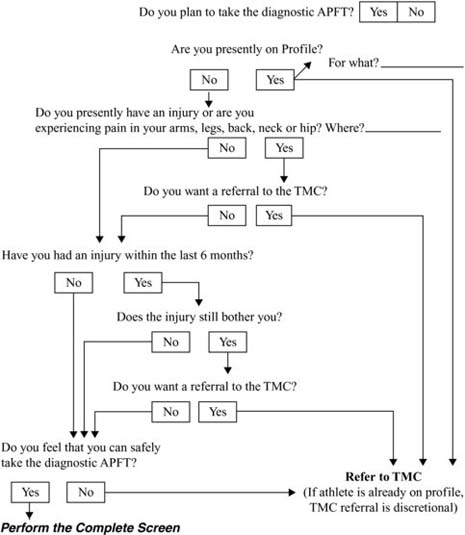
When the screening questions shown in Figure 2.2 were completed by a practitioner the potential injuries were correctly found in 92% of athletes screened. When the same process was completed by a non-practitioner only 80% of cases where positively screened. Although the results of the screening process show that it needs to be conducted by the relevant practitioner, the overall impact on the average number of days lost through injury was still similar 23 (non-screened) versus 21 days. This suggests that stringent follow-up tests are still needed to ensure that problems are dealt with effectively (Berg-Rice et al. 2007).
The initial questionnaire used for screening can also access the athlete’s psychological state towards injury and the social factors that could affect their own approach to problems. The Orebro Musculoskeletal Pain Screening Questionnaire (OMPSQ) has been used in research to look at potential problems and the subject’s pain avoidance. The athlete’s injury history will have an effect on their ability to deal with injury and how they rate their current musculoskeletal state. The OMPSQ factors into the score: fear avoidance; how well the person perceives they can deal with pain; how distressed they have been in the past about injuries; and the athlete’s own rating of their function. These scores were then combined and factors given to the rating to produce three predicting factors of how many days the athlete will miss on average a year. The first predicting factor was the function group of questions, which significantly (p = 0.001), predicted the amount of ‘Sick’ days the athlete would have over the course of a three-year period (Westman et al. 2008). The functional assessment questions looked into how athletes perceived the injury affected them and their ability to perform. The second factor that significantly predicted the amount of the missed training days due to problems was the pain factor. The athletes’ pain and injury history was factored into this predictor to significantly predict the amount of days the athlete would miss during the next three years, (p = 0.0026) (Westman et al. 2008). The final factor in this questionnaire, which was labelled fear-avoidance and was the pain that the athlete had experienced, did not significantly predict the amount of missed training days. The last factor included the athlete’s fear of training due the perceived affect it would have on an injury and therefore the length of time away from competition (Westman et al. 2008).
The scale by which athletes are often asked to report pain can be varied but the most reliable and most common is the Visual Analog Scale (VAS). The characteristics of the VAS can be seen in Figure 2.3. The scale can have a variety of anchor points and reporting periods. The way in which it categorises pain can also be varied with global, intense and general terms, all being used to interact with the patient to help them identify their pain. There is a need for a ‘golden measure’ of assessment of patient pain, and the VAS seems to be the most commonly used method at present (Litcher-Kelly et al. 2007).
Figure 2.3 VAS characteristics (Laslett et al. 2004). Reproduced, with permission, from Litcher-Kelly, L., Martion, S.A., Broderick, J.E., & Stone, A.A. (2007). A systematic review of measures used to assess chronic musculoskeletal pain in clinical and randomized controlled clinical trials. The journal of pain, 8 (12), 906–913, © 2007 Elsevier.
| Characteristic of Assessment | Coding | N |
| Quality of pain studied | Intensity | 12 |
| General pain | 8 | |
| Severity | 2 | |
| “Axial, peripheral, and global pain” | 1 | |
| “ Intensity, steady, brief (“shock-like”) and skin pain (‘pain elicited by nonpainful stimulation of the skin’)” | 1 | |
| “ Maximum, minimum, and current pain. The mean of the 3 measurements provided the pain index.” | 1 | |
| “Subjects’ overall perception of back pain.” | 1 | |
| Not provided | 4 | |
| Scale type | 100-mm line | 12 |
| 10-cm line | 9 | |
| 0–100 | 4 | |
| 0–90 mm | 1 | |
| Not provided | 4 | |
| Scale anchors | Anchors provided | 13 |
| Anchors not provided | 17 | |
| Reporting period | Current | 5 |
| Previous week/Last 7 days | 5 | |
| Daily | 2 | |
| “At rest and during activity” | 1 | |
| Hourly | 1 | |
| Morning, evening, and mean | 1 | |
| Not provided | 15 |
Functional assessments can follow a screening questionnaire or be the injury prevention process in its entirety. The test used to functionally assess an athlete can be varied and differ depending upon the area of the body and the activity the athlete competes in. The back and knee are two of the major areas that the screening process needs to assess due to their importance to locomotion and therefore the resultant sporting performance. The flexibility and posture can be governed extensively by the back and in particular the lower back strength of the athlete. If the athletes suffer from lower back pain (LBP) then they can often miss training sessions due to the lack of mobility or work at a reduced level. The importance to screen this area of the body properly and plan for any potential problems is essential in an athlete’s sporting life.
Revels model can be used as screening test for LBP, with no specific conditions. Athletes with specific LBP would need to be further screened to assess the full extent of their problems. These findings were shown in research to be applicable for 11% of the population, as the testing procedure lacked specificity (Laslett et al. 2004). The Revels testing procedure involves the patient being asked to assess the back pain currently experienced using a VAS, then the highest amount of pain and then the lowest amount of pain experienced. Subjects were then asked to complete the exercises shown in Figure 2.4. On completion of the exercises the subjects were then asked to re-evaluate their pain scores on the VAS. Using the Revels model the subjects were categorised into groups that had met the criteria and those that had not. The groups that had met the criteria had a further assessment on the lower back joints. As previously stated this only produced a positive result in those subjects with very general problems, but was significantly linked (p = 0.04) to the patients amount of ‘sick days’, i.e. those with a positive Revels test had a greater number of ‘sick days’ (Laslett et al. 2004).
Figure 2.4 The Revels model physical examination (Laslett et al. 2004). Reproduced from Laslett, M., Oberg, B., Aprill, C.N., & McDonald, B. (2004). Zygapophysial joint blocks in chronice low back pain: A test of revel’s model as a screening test. BMC Musculoskeletal Disorders, 5 (43), 1–6, public domain information courtesy of BioMed Central Ltd.
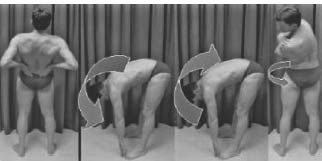
The safety of tests like the Revels model has been questioned due to the danger imposed by possible further damage to existing injuries. The condition of most concern is vertebral artery dissection (VAD). When assessing the back, practitioners must ensure that the patient’s history is fully recorded before examination, ruling out any symptoms for VAD. The patient should be assessed initially by means of non-provocative manipulation. If the area of the cervical spine needs to be manipulated then the practitioner should ensure that all symptoms for VAD have been eliminated and decide whether the provocative manipulation results are necessary or conclusions can be drawn through other means (Thiel and Rix 2005).
Another area on the body that is of paramount importance to the practitioner is the knee. An injury to the anterior cruciate (ACL) is one of the most serious problems that can happen to an athlete and have a serious effect on their career (Bonci, 1999). The prevention of injury to the ACL and the knee is very important and is dependent on identifying a series of risk factors. The major risk factors associated with ACL injuries include lower extremity malalignments, ligamentous laxity, lower extremity muscular strength considerations, neuromuscular control, hormonal influences, intercondylar notch width and the biomechanics of the athletes’ sporting techniques (Bonci, 1999). The rehabilitator can only improve and modify the strength and neuromuscular control risk factors, which is why these are key areas of a screening process (Bonci, 1999). The misalignment of the body can increase risk of injury, particularly in the back and knee. and this is very important in the lower limbs in athletes. The locomotion part of any sport technique means that any problem with the lower limb will be subjected to extreme forces. The knee in particular can only absorb a certain amount of these forces and through the nature of sport the athlete will at some point suffer injury as a result. The degrees of misalignment that will cause sufficient risk to cause potential knee problems is varied, depending on several assessments (Bonci 1999). (For greater detail regarding ACL injuries see Chapter 21, The Knee.) In order to gain a full assessment of these risks, the athlete’s foot pronation, knee recurvatum, tibial torsion and posture need to be measured. Neuromuscular control tests for the lower limb often involve a variety of movements but with common goals: to obtain an objective assessment of function and to challenge dynamic knee stability during landing and deceleration (Bonci 1999). A range of tests can be used to achieve these goals, with the single-leg hop, one-leg vertical jump, timed hop, figure of eight running, side stepping and stair running being a few of the commonly used ones (Lephart et al. 1991). These tests can also be combined with isokinetic testing to give a rounded picture of the knee (Barber et al. 1990; Lephart et al. 1991). The way the athlete’s foot lands during their gait has a large impact on the distribution of the force created. If the level of pronation is too high then one of the body’s natural shock absorbers, the heel, will be unable to prevent force from travelling up to the knee. The contact phase is where the level of pronation in the foot is critical. If the correct amount is present the movement will be inefficient and shock absorption will not occur adequately in the heel.
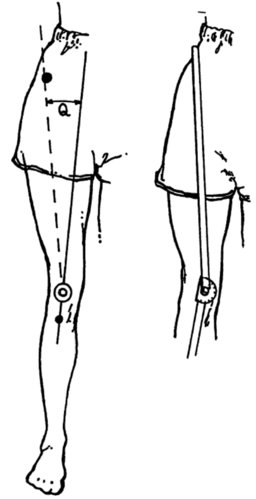
Pronation is important to the support phase, but not as stated in the contact to the shock absorption problems (Bonci 1999). The navicular drop test is commonly used to assess the pronation of the foot, and identifies the difference between the subtalar joint (STJ) in a seated neutral position (position A in Figure 2.5) and a weight bearing position (position B in Figure 2.5). Athletes who have had ACL problems generally have a difference of 13mm when compared to healthy individuals who will have a difference of just 8mm (Bonci 1999). Genu recurvatum is also known as knee hyperextension and is normally due to problems in the athlete’s skeleton and/or movement pattern abnormalities and proprioception. The problem is often increased due to soft tissue laxities, which cause occasional hyperextension of the knee. Over the course of the athlete’s career the extent and occurrences of the hyperextensions will begin to place extra strain on the ACL. This measurement is normally assessed through the extent of laxity of the thumb, fingers, elbows and hyperextension of the knee (Bonci 1999). An athlete with two or more postural problems that can be interlinked can have an increased risk of knee injuries. The increase of the Q angle can be an indicator of a problem occurring in the knee and of increased strain being placed on the ACL. The Q angle is the angle between the force line of the quadriceps and the line of pull of the patella tendon (see Figure 2.6) (Merchant, et al. 2008). The Q angle in a normal athlete is between 10 and 15 degree (Bonci, 1999). The Q angle is a useful measure of potential knee problems but the validity of this is under discussion (Merchant, et al. 2008). The varity of methods used to assess the Q angle has caused problems with the standardisation of the results found. Therefore, the use of an athlete’s Q angle must be used in conjunction with other tests to complete the screening picture (Smith et al. 2008).
Figure 2.5 Navicular drop test (Bonci, 1999). Reproduced, with permission, from Bonci, C.M. (1999). Assessment and evaluation of presisposing fators to anterior cruciate ligament injury. Journal of athletic training, 34 (2), 155–164. © 1999 National Athletic Trainers’ Association, Inc., www.nata.org/jat.
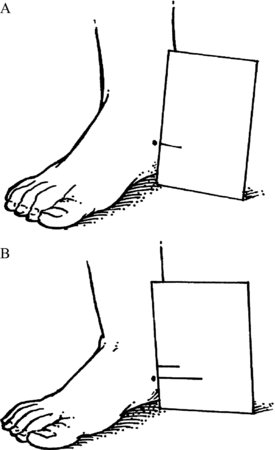
Figure 2.6 The Q angle (Bonci, 1999). Reproduced, with permission, from Bonci, C.M. (1999). Assessment and evaluation of presisposing fators to anterior cruciate ligament injury. Journal of athletic training, 34 (2), 155–164. © 1999 National Athletic Trainers’ Association, Inc., www.nata.org/jat.
The strength of the muscles around the knee has an important role to play in stabilising the joint and therefore reducing the chances of injury. If, for example, the hamstring is more than 15% weaker than the other lower limb muscles than the athlete is 2.6 times more likely to suffer lower limb injury (Knapik et al. 1991; Gabbe et al. 2009). Muscle imbalances between limbs as well as within are important in assessing the potential for injury in the knee, particularly in females where such imbalances are found in 20–30% of athletes (Bonci 1999; Gabbe et al. 2004). The ratio of flexion and extension of the joint is also a measure of potential injury, where an athlete with a ratio (eccentric to concentric) of less than 0.75 are 1.6 times more likely to suffer knee injuries (Moul 1998). Isokinetic testing at 60, 180 and 300 degrees can help accurately establish these ratios and therefore identify potential problems, but this is very sensitive to velocity changes in the testing protocol (Moore and Wade 1989). Traditional functional assessments can also provide this information, albeit, at a lower degree of accuracy, but still establish the athletes’ readiness for competition. The neuromuscular control of the athlete can be measured through a series of jumps and hops to assess the stability and awareness the athlete has of their knee movement. This is normally assessed on recovery from an injury and the most reliable test results are found using two or more jump types (Bonci 1999).
Isokinetic testing can be used in a variety of ways to profile an athlete to identify potential areas of injury concern. The simplest method is to evaluate the power output of the movements associated with the sport played and compare these against the competitive requirements. If there is a deficit then the athlete is more likely to be at risk to injury when performing that movement and can be discouraged from doing it until their power output is improved (Rosenblum and Shankar 2006). When this is complete it has been found to offer about a 10% reduction in injuries (Rosenblum and Shankar 2006) (see Chapter 3, assessing performance for greater detail regarding isokinetic assessment).
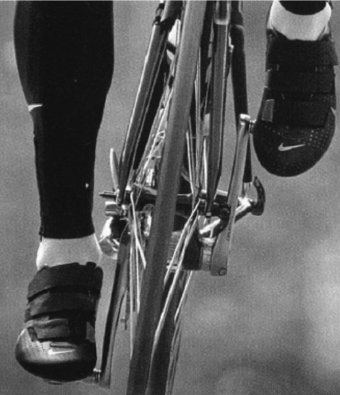
The flexibility of the muscles in the lower limbs plays an important role in the prevention of injuries to the area and should go hand in hand with a muscle development programme. The role of equipment used in the athletes’ chosen sport can also have a major effect on the potential injuries that they could suffer. For example, the height of the saddle in cycling can have implication for a range of conditions in the knee of cyclists. If the saddle is too high the athlete could suffer from illotibial band (ITB) pain and potentially suffer from ACL strains (Callaghan 2005). If conversely the saddle is too low then the athlete could suffer from patellofemoral pain, LBP and anterior knee pain (Callaghan 2005).The technique of the athlete needs to be addressed to ensure that there are limited biomechanical faults, which could also lead to injury. The way in which cyclists position their feet on the pedal (see Figure 2.7) is important for two main reasons. If the position is incorrect then the cyclist’s cadence and resultant power will be affected and performance will be hindered. Secondly if the foot is incorrectly positioned it can cause knee and back problems depending on whether it is either too far forward or too far back. The ability to rotate the heel using the toe as a fixed pivot is also important to reduce stress on the knee and also increase efficiency of movement (Callaghan and Jarvis 1996). Through kinematic analysis using pressure plates in the clips the optimum reduction of pain in the knee whilst minimising the impact on the power phase of cycle can be found. The clip system now recommended to cyclists bearing in mind these two factors is the ‘floating clip’ system, due to the amount of rotation given (Callaghan 2005). The role of the practitioner in assessing the athlete for potential injury should not just involve functional anatomical test but should look at the sport as a whole (Callaghan 2005; Callaghan and Jarvis 1996).
Figure 2.7 Metatarsal head position (Callaghan 2005). Reproduced, with permission, from Callaghan, M.J. (2005). Lower body problems and injury in cycling. Journal of bodywork and movement therapies, 9, 226–236, © 2005 Elsevier.
The problems that an athlete could potentially have are not just confined to the major joint of the back and the knee, the musculoskeletal system also needs to be assessed for any potential abnormalities. A simple Gait Arms Legs Spine (GALS) test can be used to help identify abnormalities (Beattie et al. 2008). The testing procedure has been found to be 95% accurate at helping to identify musculoskeletal abnormalities. Figure 2.8 shows the characteristics that the athlete will be assessed with, with an overall score worked out at the end. The Gait is simply classified as abnormal or normal, and then the arms, legs and spine are identified by appearance and movement. The appearance of the limb will first be assessed for abnormality and then the movement of the limb will follow using the same process. The subjects are also asked general questions about any pain or stiffness in their muscles or joints (Beattie et al. 2008).
Figure 2.8 GALS testing characteristics (Beattie et al. 2008). Reproduced, with permission, from McClean, S.G., Walker, K., Ford, K.R., Myer, G.D., Hewett, T.E., & Van den Bogert, A.J. (2005). Evaluation of a Two dimensional analysis method as a screening and evaluation tool for anterior ligament injury. British Journal of Sport Medicine, 39, 355–362 © 2005 BMJ Publishing Group Ltd.
| GAIT |
| • Symmetry & smoothness of movement |
| • Stride length & mechanics |
| • Ability to turn normally & quickly |
| ARMS (Hands) |
| • Wrist/finger swelling/deformity |
| • Squeeze across 2nd to 5th metacarpals for tenderness (Indicates synovltls) |
| • Turn hands over, Inspect muscle wasting & forearm pronation/suplnation |
| ARMS (Grip Strength) |
| • Power grip (tight fist) |
| • Precision grip (oppose each finger to thumb) |
| ARMS (Elbows) |
| • Full extension |
| ARMS (Shoulders) |
| • Abduction & external rotation of shoulders |
| LEGS (Feet) |
| • Squeeze across metatarsals for tenderness (indicates synovitis) |
| • Calluses |
| LEGS (Knees) |
| • Knee swelling/deformity, effusion |
| • Quadriceps muscle bulk |
| • Crepitus during passive knee flexion |
| LEGS (Hips) |
| • Check internal rotation of hips |
| SPINE (Inspection from behind) |
| • Shoulders & iliac crest height symmetry |
| • Scoliosis |
| • Paraspinal, shoulder, buttocks, thighs & calves muscles normal |
| • Popliteal or hind foot swelling or deformity |
| SPINE (Inspection from front) |
| • Quadriceps normal in bulk & symmetry |
| • Swelling or at Varus or valgus deformity at knee |
| • Forefoot of midfoot deformity action normal |
| • Ear against shoulder on either side to check lateral cervical spine flexion |
| • Hands behind head with elbows back (check rotator cuff muscles, acromioclavicular, sternoclavicular & elbow joints) |
| SPINE (Inspection from side) |
| • Normal thoracic & lumbar lordosis |
| • Normal cervical kyphosis |
| • Normal flexion (lumbosacral rhythm from lumbar lordosis to kyphosis) while touching toes |
| SPINE (Trigger point tenderness) |
| • Supraspinatus muscle tenderness (exaggerated response) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







