CHAPTER 77 Injuries of the Lower Cervical Spine
Cervical spine injuries occur in 3% to 4% of all trauma patients.1 Spinal cord injury is much rarer occurring in only about 12,000 people per year in the United States. Because of the association with traumatic brain injury, the risk of spinal injury can be stratified by level of consciousness, occurring in only 2.8% of alert compared with 7.7% of nonevaluable patients.2 It is estimated that about 40% of these injuries will be unstable with potential for neurologic injury.
The importance of the evaluation and protection of the cervical spine is underscored by continued reports of neurologic deterioration that occurs after patients are admitted to hospitals. Levi and colleagues3 retrospectively reviewed 24 cases of patients who deteriorated after admission to level I trauma centers. Neurologic deterioration occurred overall in 0.026% of all trauma patients and 0.21% of patients with known spinal injuries. The common cause was inadequate radiographs, misreading, and poor-quality studies.
Positive changes documenting improvement of the overall care of spinal cord–injured patients have occurred. The time of admission to rehabilitation centers decreased from 23 to 7 days.4 A fivefold decrease in rehabilitation duration has occurred due to better overall management and greater financial constraints. Functional impairment at discharge has seen improvement for three consecutive decades. This is also consistent with decreasing admission of compete quadriplegia compared with increased incomplete quadriplegics. Overall mortality (occurring within the first year postinjury) decreased over 65% from the 1970s to 1990s.5
Many of these improvements resulted from better initial accident care, earlier diagnosis, improved resuscitation methods, and modern surgical techniques. The emergency care of the spinal cord–injured patient is discussed in Chapter 81. This chapter reviews the evaluation of the cervical spine in a trauma patient, new classification systems of lower cervical spine injuries, and their application to surgical decision making.
Anatomy
The anatomy of the cervical spine is reviewed in detail in Chapter 2. These remarks are aimed at the anatomy specific to cervical injuries and their treatment. The subaxial cervical spine is highly mobile but protective of its soft tissue contents, namely the spinal cord, nerve roots, and vertebral arteries. Each vertebra from C3 to 7 is progressively larger and is connected both above and below by three articulations, the disc complex and the paired lateral pillars. These form three columns that are essential for the weight-bearing function of the spine. The anterior column is connected to each lateral pillar by pedicles, and the lateral pillars are connected by the lamina. Thus the lamina and pedicle act as tie-rod connectors. The large spinous processes are levers for attachment of the paraspinal muscles and ligaments. These combined with the nuchal ligaments form the posterior ligamentous complex. which is essential to maintaining stability against flexion and anterior shear forces.
Biomechanics and Kinematics
Kinematically each segment of the subaxial spine normally has approximately 11, 5, and 5 degrees of movement in flexion-extension, lateral bending, and rotation.6 Small amounts (1 to 2 mm) of translation occur in both anterior-posterior and lateral directions. Normal passive motion requires little application of load, which is measured by the neutral zone. Injury will increase the dimension of the neutral zone and when this exceeds certain thresholds such that the neural structures are at risk, the spine is deemed unstable.
Anatomic Considerations for Surgery
Screw fixation into the lateral masses requires identification of a proper starting point and screw direction. The lateral mass is first examined and its borders defined. The cranial and caudal borders are the corresponding facet joints, the lateral border is the edge of the lateral mass, and the medial border is the valley at the junction of the lamina and lateral mass. Several starting points have been described.7–9 However, with modern fixation most authors use a modified technique where the starting point is 1 to 2 mm medial to center of the lateral mass. The author marks this point with a small burr so that when a pilot hole is started it is located at the selected point. The pilot hole is oriented upward attempting to be parallel to the facet articulations and outward about 15 to 30 degrees. This outward orientation is essential to avoid injury to the vertebral artery, which lies directly anterior to the starting point as seen on axial images. The outward angulation is often limited by the next caudal spinous process.
Assessment
Clinical Examination
The clinical examination is an essential component of the evaluation process. It depends on cooperation between examiner and patient, requiring normal mentation. Sensitivity is reduced by the patient’s inability to report symptoms due to conditions such as distracting pain, mild head injuries, or intoxication.10 The clinical examination is performed by reviewing the history of injury and symptoms of cervical pain, numbness, weakness, or paresthesias. The examination assesses spinal tenderness, which is best achieved by carefully logrolling the patient and palpating from the occiput to sacrum. Tenderness, swelling, hematoma, and gaps between spinous processes are indications for further evaluation.
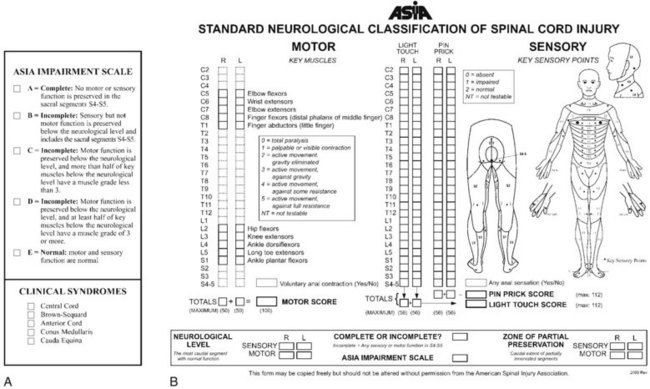
The neurologic examination is performed using standards established by the American Spinal Injury Association (Fig. 77–1).11 These should be recorded in the medical record in a timely manner. The neurologic examination includes testing of cranial nerves, motor and sensory function, and perineal function. Motor function of key muscle groups in the arms and legs are assessed from grades 0 to 5 (Table 77–1). Several sensory functions including pinprick, light touch, and proprioception or vibratory function are tested in both the upper and lower extremities. Sensory function is graded 0, 1, or 2 (absent, hypoesthesia, and normal, respectively). Deep tendon and pathologic reflexes are determined. Hyperreflexia and findings of clonus, Babinski signs, or Hoffmann signs are indications of spinal cord compression, although in cases of acute spinal cord injury areflexia is initially common. The level of spinal cord injury is defined as the lowest-functioning root level with at least grade 3 motor function. Complete spinal cord injuries are defined as the absence of any motor or sensory function including sacral roots distal to the zone of injury. Incomplete cord syndromes have some retained motor or sensory function and have a significantly better prognosis than complete lesions. The overall impairment is graded by the modified Frankel (ASIA) scale: A—motor and sensory complete; B—motor complete with sensory sparing; C—motor and sensory sparing but not functional strength; D—motor and sensory sparing with functional strength; E—normal motor and sensory.11
| Upper Extremity | |
| Biceps | C5 |
| Wrist extension | C6 |
| Triceps | C7 |
| Finger flexion | C8 |
| Finger abduction | T1 |
| Lower Extremity | |
| Iliopsoas | L2 |
| Quadriceps | L3 |
| Anterior tibialis | L4 |
| Extensor hallucis longus | L5 |
| Gastrocsoleus | S1 |
Clearing the Cervical Spine
Patient Presentation
After the clinical examination, a decision is made whether radiologic studies are indicated. To determine the proper course, patients can be divided into one of four groups: asymptomatic; temporarily nonevaluable but asymptomatic; symptomatic; and obtunded. Asymptomatic patients are those who have no pain, no cervical tenderness, neurologic signs and symptoms and who are awake, alert, and nonintoxicated.1 Additionally, they do not have any distracting injuries that may preclude pain assessment of a potential cervical spine injury. Distracting injuries include long bone fractures, burns, visceral injury, dislocations, and craniofacial or thoracic trauma. The temporarily nonevaluable patient is otherwise asymptomatic but is either intoxicated where sobriety is expected within 24 hours or will have resolution of other painful injuries through reduction or fixation. It is hypothesized that these patients can be evaluated similar to the asymptomatic patients in a delayed fashion.12 Symptomatic patients have cervical pain, tenderness, or neurologic symptoms such as paresthesias, weakness, or numbness. The obtunded patient is one who will not be able to fully participate in the clearance process and at the same time is at highest risk for injury. Included in this group are disabled and infant patients.
Asymptomatic Patient
Multiple large multicenter prospective trials, institutional prospective studies, systematic reviews, and meta-analyses demonstrate conclusively that the asymptomatic patient can be cleared after clinical assessment and does not require radiographic evaluation.13–17 Designation as asymptomatic will clear 99.8% of patients without radiographs and use of such protocol only rarely misses a significant injury.13 In more than 62,000 cases, no neurologic complication occurred after clearance of asymptomatic patients on clinical grounds.
Symptomatic Patients
Symptomatic patients are at significant risk of cervical injury and all authorities agree that imaging is required.14,15 In cases of obvious cervical cord injury, this may be by means of a lateral radiograph so that traction can be instituted immediately if a fracture dislocation is present. More commonly, a multidetector CT (MDCT) is performed. MDCT allows acquisition of thin-slice thicknesses (1.25 to 1.5 mm) and affords high-resolution reconstruction in all three planes. Compared with plain radiographs, it has significantly increased sensitivity and is cost effective if CT imaging of other body parts are required.18 Magnetic resonance imaging (MRI) is indicated after CT or plain radiographs when there are unexplained neurologic defects, progressive deterioration, preoperatively, and in cases of facet dislocation of neurologically intact patients. Further, MRI with fat suppression is useful to identify ligamentous disruption, which may aid surgical decision making.
Obtunded Patients
No agreement has been reached as to the best method to evaluate the cervical spine of cognitively impaired patients. However, all stakeholders agree that radiologic evaluation is warranted in this high-risk group.15 Current recommendation is divided into two groups: MDCT alone19,20 and MDCT with MRI.21 MDCT is easy to perform and likely identifies all osseous injuries. However, ligamentous injury may be missed if the spine is reduced in normal alignment. If restrictions are released, then displacement may occur when the patient is no longer immobilized. Given the high resolution of MDCT compared with older CT studies, proponents of this modality believe the risk of this is small. The latter technique takes advantage of both MCDT, which identifies osseous injury, and MRI, which is sensitive for ligamentous injury. A recent meta-analysis shows that MRI has a 100% negative predictive value, indicating that a negative study excludes any significant injury.1 However, there is a high false-positive rate, meaning that many patients will be treated unnecessarily. In the absence of proof of the superiority of either approach, the author recommends that each institution develop and use a protocol to evaluate these patients.
Classification
Classification of spinal injuries is difficult due to the complex anatomy of vertebrae, the presence of a three-joint complex, and the many ligamentous structures responsible for stability. Classification systems can be broadly categorized as morphologic, mechanistic, and by stability. Morphologic systems use common names that describe the pathoanatomy such as burst fracture or facet dislocation. These are useful but do not help to define treatment or imply prognosis. Mechanistic systems attempt to identify force vectors that cause injury.22 Using these, potential treatment strategies can be induced, usually by reversing the vector direction. Stability is hard to define but implies the ability of the spine to withstand physiologic loads. This is well grounded in sound biomechanical principles but is more difficult to use clinically. All of these classification systems have many limitations including not being comprehensive, not aiding treatment decision making, not using modern imaging, and lacking reliability and validity.
Stability and neurologic status are the most important factors when treating patients with cervical spine trauma. Stability was initially described by Nicoll, who identified patterns of injury that were associated with poor functional outcomes (i.e., inability to return to work as a miner).23 He found that posterior ligamentous injuries and dislocations were “unstable patterns.” Stability has been defined by White and Panjabi6 as “ability of the spine under physiologic loads to maintain a relationship between vertebral segments in such a way that there is neither damage nor subsequent irritation of the spinal cord or nerve roots, and, in addition, there is no development of incapacitating deformity or pain due to structural changes.” Stability as thus defined is dichotomous when in fact stability is a continuous variable with many shades of gray. In an effort to quantify clinical stability and thus make it useful for traditional decision making, White and Panjabi6 developed a checklist. Points are assigned for injury to anterior or posterior columns, translation, excessive angulation, distraction, and neurologic injury. Higher scores indicate greater degrees of instability. This concept is well founded with biomechanical studies but has not proven useful as a clinical tool or even been tested for validity.
White and colleagues24 performed elegant biomechanical studies on cadaveric spines with serial ligamentous sectioning. After each ligament was divided, loads were applied and motion measured. They found that the cervical spine developed excessive motions when all elements of one column (anterior or posterior) and one other ligament were sectioned. The amount of displacement at this time was 3.5 mm of translation and 11 degrees of greater angulation than adjacent levels. These parameters were exceeded only after injury and are accepted as rendering the spine unstable clinically. Practically, however, the cases most difficult to assess for stability do not have displacements or angulation exceeding these limits.
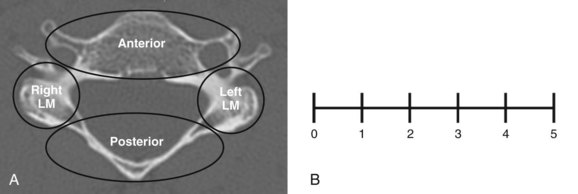
Cervical Spine Injury Severity Score
The Cervical Spine Injury Severity Score (CSISS) is based on independent analysis of four columns (anterior, posterior, right column, and left lateral column) (Table 77–2).25 The anterior column includes the body, disc including the annulus, anterior and posterior longitudinal ligaments, and transverse processes. Each lateral column is scored separately and includes the facet projections, lateral mass, pedicles, and facet joint capsules. The posterior column includes the lamina, spinous process, ligamentum flavum, and nuchal ligaments (Fig. 77–2A).
TABLE 77–2 Cervical Spine Injury Severity Score (CSISS)
| CSISS Analog Score | |
|---|---|
| Anterior column | 0-5 |
| Right pillar | 0-5 |
| Left pillar | 0-5 |
| Posterior column | 0-5 |
| Total | 0-20* |
* Scores < 5 are generally treated nonoperatively. Scores > 7 are usually treated surgically.
Each column is scored using a 0-5 analog scale (Fig. 77–2B). Fractional scores can be used. Scores increase proportional to either displacement of fracture fragments or separation as a result of soft tissue injury. For example, a nondisplaced fracture is scored 1 while the worst injury possible for that column (e.g., facet fracture dislocation with 10-mm displacement) is a 5. Each column is scored independently and summed, giving the CSISS ranging 0-20.
Anderson and colleagues25 assessed reliability in 34 cases with 15 examiners. Both intraobserver and interobserver reliability were excellent. Construct validity was also good as all patients with scores equal to 7 had surgery, whereas only 15% less than 5 had surgery (Fig. 77–3). Caput and colleagues26 retrospectively correlated CSISS score to surgical approach in 70 patients. They found a significant correlation with high CSISS scores (>11) to a posterior or combined anteroposterior approach. The anterior approach had lower scores with a mean 6.3, indicating that anterior surgery was used for less severe injuries, in accordance with well-known biomechanical studies.
Subaxial Cervical Spine Injury Classification
The Subaxial Cervical Spine Injury Classification system (SLIC) evaluates fracture morphology, the discoligamentous complex, and neurologic function, creating a comprehensive system to aid treatment decision making (Table 77–3).27 The system assigns points for each domain and if the score exceeds a threshold, surgery would be indicated.
Overall Subaxial Cervical Spine Injury Classification Score
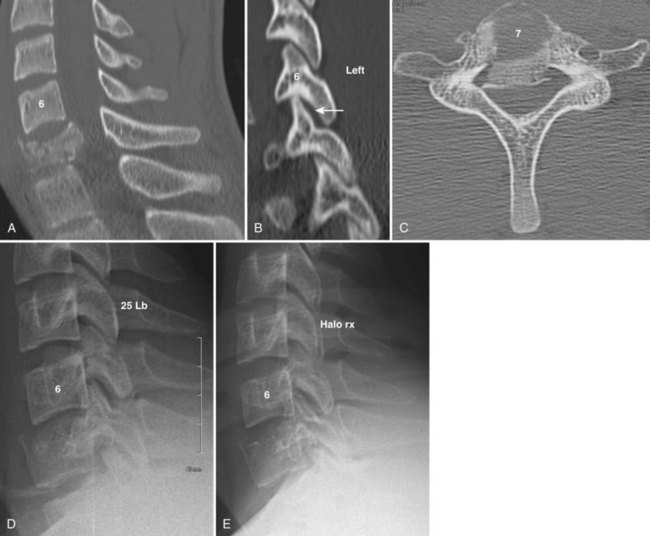
The SLIC score is the sum of the individual components. A patient with an SLIC score equal to 3 is treated nonoperatively, whereas surgery is recommended in a patient with a score equal to 5 (Fig. 77–4). Scores of 4 can be treated either operatively or nonoperatively.
Vaccaro and colleagues27 tested the reliability of the SLIC system. Interobserver reliability was only moderate, and both injury morphology and discoligamentous complex scores were only fair. Intraobserver reliability was excellent for overall and individual components. Similar to the CSISS, the system was valid when tested against treatment decisions. The SLIC system predicted accurately what the individual observers would recommend in 91% of cases.
Specific Injury Types
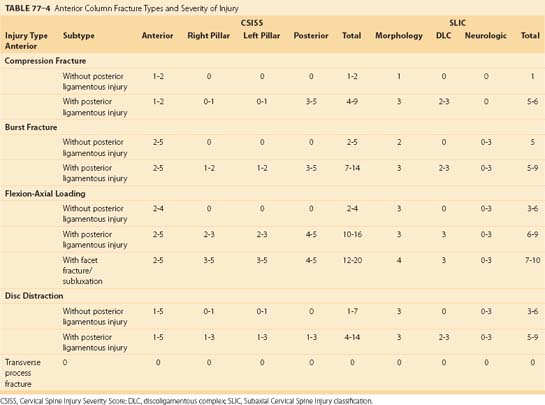
Anterior Column Injuries
Anterior column injuries include compression fractures, burst fractures, flexion axial loading injury, and disc distraction injuries (Table 77–4). Transverse process fractures are included in this group, although they have no effect on spinal stability but may be associated with vertebral artery injury. Most anterior column injuries are easily recognizable on plain radiographs or CT. When present, they suggest a hyperflexion mechanism and a search for a concomitant injury to the posterior ligamentous complex should ensue. The notable exception is the disc-distraction injury resulting from opposite forces (i.e., extension and posterior shear). These injuries can be subtle, especially in patients with preexisting spondylosis.
Anterior Compression Fractures
Mechanism of Injury
Anterior compression fractures, like burst fractures, occur from hyperflexion and/or axial loading forces. During this loading, the disc is pressurized, resulting in failure of the endplate and creating wedging of the vertebral body. This usually occurs along the superior endplate. During hyperflexion the posterior ligaments may be strained beyond physiologic limits, causing disruption. This injury pattern has been termed “hidden flexion injury” and often fails nonoperative treatment.28
Assessment
Isolated compression fractures without posterior or lateral mass involvement almost always score low CSISS (0-2) and SLIC (1) scores (see Table 77–4). When associated with posterior ligamentous injury or facet perching, CSISS and SLIC scores range 7 to 10 and 5 to 6, respectively, indicating a moderate degree of instability.
Burst Fractures
Radiographic Assessment
Burst fractures occur most commonly at C6 and C7 rather than the mid or upper cervical spine (see Fig. 77–4). On lateral views, both anterior and posterior vertebral body heights are shortened and a small fragment from the posterior superior body is rotated into the spinal canal. Interspinous widening or facet perching or subluxation, when present, indicate posterior ligamentous injury.
Flexion Axial Loading Injury
Mechanism of Injury
Flexion/axial loading injuries, also called tear drop fractures, are devastating injuries due to the propensity for neurologic injury and often are the result of diving or other sports-related activities. The injury occurs from a compression force obliquely applied in a downward and posterior direction. Forces are concentrated in the anterior inferior corner of the vertebral body, which is sheared off, giving the injury its name (see Fig. 77–3). The remaining part of the vertebral body shears through the disc space and rotates posteriorly into the spinal canal, crushing the spinal cord. Varying amounts of flexion strain occur in the posterior ligamentous complex, which accounts for a wide presentation of stability with this injury.
Assessment
In cases without posterior ligamentous disruption, CSISS scores range from 3 to 5 because of anterior displacement with minimal injury to lateral masses or posterior ligamentous complex. The SLIC score is 3 for a distraction injury with increasing scores being based on neurologic involvement. When associated with posterior ligamentous complex injury or facet fractures/subluxation, high scores on both CSISS and SLIC are present (see Fig. 77–3).
Transverse Process Fractures
Transverse process fractures are quite common, occurring in isolation or in association with other more severe injuries. These fractures are not involved with spinal stability and therefore are not significant in treatment decision making for the spine. However, transverse process fractures at C6 and above may warn of possible vertebral artery injury.29 No consensus has been reached regarding whether routine vascular evaluation and subsequent treatment with anticoagulants are required in patients with these injuries. This topic is discussed in detail in Chapter 82.
Disc-Distraction Injury
Radiographic Analysis
MRI is useful to identify questionable cases. Classic findings are increased signal in anterior soft tissues both rostral and caudal to the injured disc. Increased signal intensity across the disc space transversing the anterior annulus and anterior longitudinal ligament is pathognomonic (Fig. 77–5). Rarely the posterior longitudinal ligament will be involved. Disc herniation and spinal cord compression from stenosis or malalignment may be present as well. Posterior increased signal in the facet joints and ligamentum flavum are indicative of more extensive injury and greater instability.
Treatment of Anterior Column Injuries
Anterior column injuries with low SLIC or CSISS scores can be treated non-operatively (Table 77–5). These include compression injuries, stable forms of burst fractures and flexion/distraction injuries, and most disc-distraction injuries (see Fig. 77–4). Less significant injuries can be treated with a cervical collar, while burst fractures and flexion/axial loading injuries can be treated with a cervical thoracic orthosis (CTO) or halo vest.
TABLE 77–5 Treatment of Anterior Column Injuries
| Injury Type | Subtype | Treatment Options |
|---|---|---|
| Compression Fracture | ||
| Without posterior ligamentous injury | COLLAR, CTO | |
| With posterior ligamentous injury | Collar, CTO POSTERIOR FUSION | |
| Burst Fracture | ||
| Without posterior ligamentous injury | Collar, CTO HALO VEST Posterior fusion Anterior fusion | |
| With posterior ligamentous injury | Collar, CTO Halo vest Posterior fusion ANTERIOR FUSION Anteroposterior fusion | |
| Flexion-Axial Loading | ||
| Without posterior ligamentous injury | Collar, CTO HALO VEST Posterior fusion Anterior fusion | |
| With posterior ligamentous injury | Collar, CTO Halo vest Posterior fusion ANTERIOR FUSION Anteroposterior fusion | |
| With facet fracture/ subluxation | Collar, CTO Halo vest Posterior fusion Anterior fusion ANTEROPOSTERIOR FUSION | |
| Disc Distraction Injury | ||
| Without posterior ligamentous injury | COLLAR, CTO | |
| With posterior ligamentous injury | Collar, CTO Halo vest Posterior fusion ANTERIOR FUSION | |
| Transverse Process Fracture | ||
| No vertebral artery injury | OBSERVATION | |
| Vertebral artery injury | Observation ANTICOAGULATION | |
CTO, cervicothoracic orthosis.
Authors’ recommendations are in bold capitals.
Surgical indications for anterior column injuries are those with evidence of disruption of the posterior ligamentous complex as demonstrated by high CSISS and SLIC scores (see Table 77–5). In the case of compression fractures when surgery is warranted, the author recommends posterior fusion because a single-level anterior fusion may fail in the face of a vertebral fracture at the location of caudal screw fixation. Burst fractures and flexion/axial loading injuries can be reduced or significantly improved with tong traction. Although both anterior and posterior approaches may be used, the authors recommend addressing pathology at its major location (i.e., anteriorly) (see Fig. 77–3). After strut grafting or insertion of a cage, an anterior plate is applied. Although a rigid locked plate has theoretical advantages over a translational plate, the author has not observed any clinical differences in outcomes between the two plates. In rare cases of extensive comminution, associated facet dislocations, or those having residual displacement of lamina fractures, combined anterior and posterior approaches are indicated.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree