I. Joint Injuries of the Hand
A. Overview
1. Anatomy (Figs. 24-1 through 24-4)—The small joints of the hand are hinged joints. The metacarpophalangeal (MCP) joints have a cam configuration, whereas the proximal interphalangeal (PIP) and distal interphalangeal (DIP) joints have a spherical shape. Stability depends on the articular contour, collateral ligaments, and volar plate. The volar plate has strong lateral attachments, but a weak distal attachment.
2. Small joint injuries—A partial or complete tear of the collateral ligaments, volar plate, or extensor tendon results in subluxation or dislocation of the finger joint. Intra-articular fractures, including avulsion fractures and fracture-dislocations, may be associated with these injuries.
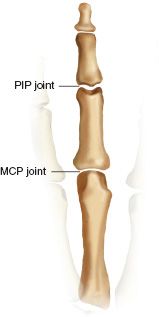
FIGURE 24-1 Metacarpophalangeal joints are unicondylar, and proximal interphalangeal joints are bicondylar, giving the PIP joints more stability.
3. Evaluation—Swelling, tenderness, or ecchymosis of a finger should raise suspicion for a joint injury. Stress testing may reveal instability as a result of underlying fracture or ligamentous injury. Comparison stress testing to the noninjured opposite side is helpful in cases of ligamentous laxity. Limited motion of a joint may result from joint subluxation or a displaced articular fragment. Evaluation of these injuries requires excellent quality radiographs, including an anteroposterior (AP) X-ray view, a true lateral X-ray view centered on the injured articulation, and one or two oblique views. Tomograms may occasionally be necessary to obtain better visualization of a centrally depressed fracture.
4. Treatment and outcome—Pain-free motion and joint stability are the treatment goals for these injuries. Treatment must correct subluxation and restore an acceptable joint surface. Studies suggest that pain and motion may improve for up to 1 year after injury to a small joint of the hand.
B. DIP Joint Injuries
1. Mallet finger (Fig. 24-5)—A sudden forceful flexion to the DIP joint may rupture the extensor tendon from the distal phalanx, with or without a bone fragment. Large fracture fragments involving more than 30% of the articular surface are at risk for volar subluxation of the distal phalanx.
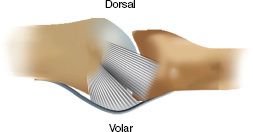
FIGURE 24-2 Collateral ligaments have a cordlike dorsal component and a fan-shaped volar component.
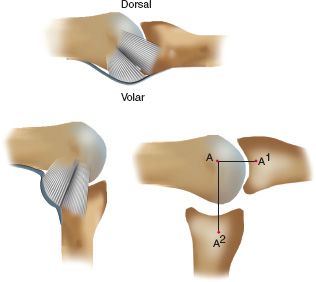
FIGURE 24-3 The shape of the metacarpal head is eccentric. This creates a cam effect that makes the collateral ligaments more taut in flexion than in extension (the distance from A to A1 is less than the distance from A to A2.
• Evaluation—Examination may reveal pain, swelling, and a dropped finger at the DIP joint. X-ray films demonstrate a flexed DIP joint and may demonstrate a fracture fragment still attached to the extensor tendon. Volar subluxation of the distal phalanx may accompany the fracture, particularly if the fragment is large.
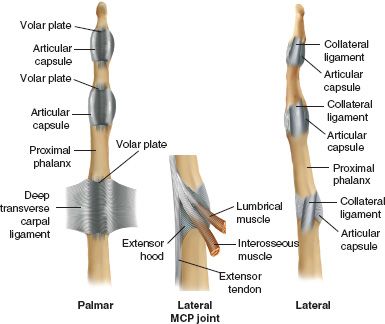
FIGURE 24-4 Structures about the MCP and interphalangeal joints.
• Classification of Mallet Finger
(a) Type I—It involves closed or blunt trauma with loss of tendon continuity, with or without a small chip fracture.
(b) Type II—It involves a laceration at or proximal to the DIP joint with loss of tendon continuity.
(c) Type III—It involves a deep abrasion with loss of skin, subcutaneous cover, and tendon substance.
(d) Type IV—It involves a physeal fracture in children, a hyperflexion injury with a fracture involving 20% to 50% of the articular surface, or a hyperextension injury with a fracture of the articular surface usually greater than 50% and with early or late volar subluxation of the distal phalanx.
• Treatment
(a) Closed treatment—Splinting or casting is indicated for mallet finger injuries with small fracture fragments that involve less than 30% of the articular surface or are displaced less than 2 mm. The mallet finger is treated in extension for 6 weeks full time, followed by another 4 weeks at night (Fig. 24-6).
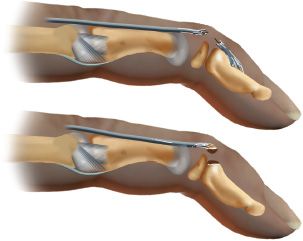
FIGURE 24-5 Mallet finger. Soft-tissue (terminal extensor tendon tear) mallet (top) and bony mallet (bottom).
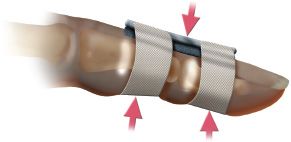
FIGURE 24-6 Extension splinting of the DIP joint for mallet injuries. The dorsal padded aluminum splint uses the three-point fixation principle (arrows).
(b) Surgery—Mallet finger deformities require surgery when they are associated with fracture fragments greater than 30% of the joint surface, are displaced more than 2 mm, or are associated with volar subluxation of the distal phalanx. Volar subluxation of the DIP joint is the strongest indication for surgery. Open reduction with internal fixation (ORIF) of the fracture fragment is recommended to correct the volar subluxation of the DIP joint with a longitudinal K-wire in extension (Fig. 24-7); tendon repair is performed as needed. The use of a pullout button may lead to skin slough (beneath the button). Suture anchor fixation may be preferable.

FIGURE 24-7 A. X-ray film showing a mallet finger of bony origin. B. Postoperative film showing stabilization using a suture anchor and a Kirschner wire.
• Complications—Complications include persistent mallet deformity, secondary swan-neck deformity (Fig. 24-8), and traumatic arthritis of the DIP joint as a result of an incongruent joint or volar subluxation.
2. Dorsal dislocation of the DIP joint—A hyperextension force at the tip of the finger may disrupt the volar plate and the collateral ligaments, whereas the insertion of the profundus tendon remains intact. These injuries are frequently associated with a volar laceration (64% of cases), since the skin is firmly bound to the underlying bone.
• Evaluation
(a) Clinical examination—There is tenderness and deformity at the DIP joint. The patient is unable to flex or extend the joint.
(b) Radiographic evaluation—AP and true lateral X-ray studies should be taken before manipulation. Dislocations are usually dorsal and rarely lateral. Associated avulsion fractures should be identified.
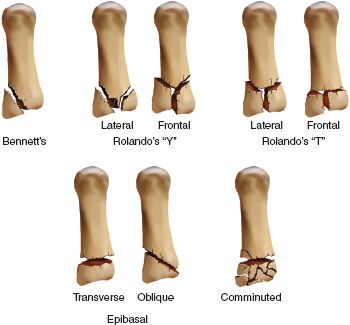
FIGURE 24-8 Swan-neck deformity from dorsal subluxation of the lateral bands.
• Classification—Types include closed dislocation, open dislocation, and fracture-dislocation.
• Treatment
(a) Closed reduction—Gentle closed reduction is performed under metacarpal block anesthesia. The distal phalanx is extended and then reduced over the condyle. Stability after reduction should be assessed, although there is usually little tendency for redislocation. Postreduction X-ray studies should demonstrate a congruent reduction and no associated fractures. A short period of immobilization (10 to 14 days) is usually adequate. Thorough irrigation and debridement of any open laceration should be performed before reduction.
(b) Surgery—Irreducible dislocations of the DIP joint may result from interposition of the volar plate, interposition of the profundus flexor tendon, or a displaced osteochondral fracture fragment. In these cases, open reduction may be necessary to extract the interposed volar plate, sesamoid bone, or fracture fragment. Interposition of the profundus tendon should imply rupture of at least one collateral ligament, and in this case, immobilization should be continued for 3 weeks.
• Complications—Complications include posttraumatic stiffness, recurrent instability, posttraumatic arthritis, and infection (septic arthritis and osteomyelitis).
C. PIP Joint Injuries
1. Collateral ligament sprain of the PIP joint—An abduction or adduction force to the extended finger may result in tearing of the radial or ulnar collateral ligament at the PIP joint. The radial collateral ligament is injured more frequently than the ulnar collateral ligament.
• Diagnosis—Clinical examination demonstrates point tenderness over the specific site of injury. Ligament failure usually occurs at the proximal phalanx or less frequently, in the mid-portion of the ligament. Stress testing should be performed with the joint in extension or 20° of flexion. Lack of a firm end point is diagnostic of a complete tear. Angulation greater than 20° on an AP stress X-ray film is also diagnostic of a complete tear. Small chip fractures may be noted at the origin of the collateral ligament. Digital block may facilitate examination.
• Treatment
(a) Closed treatment—Partial tears and most complete tears can be treated with static splinting for 7 to 14 days, followed by buddy-taping to the adjacent digit for 3 weeks. Active motion is encouraged from the outset. Residual joint discomfort and thickening of the collateral ligament as a result of underlying scar tissue formation are common, lasting for 3 to 6 months.
(b) Surgery—Indications for surgery include radiographic evidence of soft-tissue interposition, a displaced condylar fracture of the phalanx, or continued instability after 3 weeks of static splinting. Surgery for the radial collateral ligament to the index finger may be necessary to restore lateral key-pinch strength.
2. Volar plate injury of the PIP joint—Hyperextension injury to the PIP joint may cause the volar plate to tear from the middle phalanx, with or without a bone fragment.
• Diagnosis
(a) Clinical examination—There is fusiform swelling of the PIP joint, with point tenderness greatest over the volar plate.
(b) Radiographic evaluation—Lateral X-ray films may show a small avulsion fracture fragment at the base of the middle phalanx, usually less than 10% of the joint surface. The PIP joint is usually reduced without subluxation.
• Treatment—Closed management is indicated. Stable injuries are immobilized in a dorsal splint with 20° of flexion for 1 week, followed by an active range-of-motion program using buddy-taping.
• Complications—Complications include posttraumatic flexion contracture, pain with limited range of motion, and late swan-neck deformity.
3. Dorsal dislocation of the PIP joint—One of the most frequently encountered articular injures of the hand is dorsal dislocation of the PIP joint. Hyperextension of the PIP joint forces the finger backward, resulting in dislocation of the middle phalanx dorsally relative to the proximal phalanx, tearing the volar plate.
• Diagnosis
(a) Examination—The finger usually has an obvious deformity as a result of the dislocation, unless it has already been reduced by a trainer or a bystander. Hyperextension stress testing determines residual instability. Collateral ligament stability may be satisfactory with a pure dorsal dislocation.
(b) Radiographic evaluation—X-ray films demonstrate the dislocation of the PIP joint (Fig. 24-9). A small avulsion fracture from the middle phalanx may be seen, identifying the distal location of the volar plate.
• Treatment—Closed reduction is performed under a metacarpal block anesthesia with longitudinal traction. Most dorsal dislocations are easily reduced. With stable reduction, range of motion may begin early with continuous buddy-taping for 3 to 6 weeks. Less stable injuries may require an extension blocking splint to prevent the last 20° of extension for 3 weeks. If the volar fracture fragment contains more than 15% of the volar surface, operative intervention may be needed. Open dislocation should be thoroughly irrigated in the operating room, with extension of the skin lacerations if needed. Rotational deformity of the finger may suggest entrapment of the middle phalanx condyle between the lateral band and the central slip. This situation is often irreducible with closed traction and may require open reduction with repair of the extensor mechanism.
• Complications—Complications include posttraumatic flexion contracture, pseudo-boutonnière deformity, and hyperextension instability.
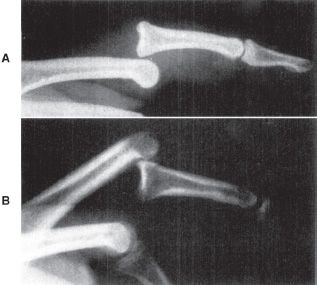
FIGURE 24-9 PIP joint dislocation. A. Dorsal dislocation (most common) can usually be treated by closed reduction and buddy-taping. Loss of reduction in extension may require extension block splinting. B. Volar dislocation (unusual) may require operative repair of the extensor tendon central slip. (Reprinted with permission from Green DP, Strickland JW. In: DeLee JC, Drez D Jr, eds. Orthopaedic Sports Medicine: Principles and Practice. Philadelphia, PA: WB Saunders; 1994.)
4. Volar dislocation of the PIP joint—The central slip insertion on the proximal phalanx is ruptured.
• Diagnosis
(a) Examination—Deformity and limited motion are usually obvious. If the joint has spontaneously reduced, lack of active extension of the middle phalanx against resistance should suggest rupture of the central slip. An irreducible dislocation can occur if the lateral bands or central slip becomes trapped under the head of the proximal phalanx.
(b) Radiographic evaluation—X-ray films demonstrate volar dislocation of the PIP joint (see Fig. 24-9). A small avulsion fracture may be seen at the dorsum of the middle phalanx as a result of the ruptured central slip insertion.
• Treatment—Closed reduction may be attempted with longitudinal traction and flexion of the MCP and PIP joints. The stability and strength of the central slip are tested after reduction. If the central slip is intact, a short period of immobilization can be followed by a carefully controlled range-of-motion program. A disrupted central slip must be treated with static splinting in extension for 6 weeks or open operative repair of the disrupted central slip mechanism.
• Complications—Complications include extension contracture, PIP or DIP joint stiffness, and progressive boutonnière deformity. Failure to diagnosis the central slip rupture results in progressive volar subluxation of the lateral bands of the extensor mechanism and a resulting boutonnière deformity (Fig. 24-10). Global instability is another complication.
5. Fracture-dislocation of the PIP joint—Hyperextension, impaction, shear, and pilon fracture-dislocation may occur. These injuries are the most disabling PIP joint injuries.
• Diagnosis
(a) Examination—Swelling, pain, and limited motion, often without severe deformity, is seen. This injury is commonly mistaken as a sprain.
(b) Radiographic evaluation—Radiographic evaluation is imperative. In a true lateral X-ray film centered on the injured joint, articular fracture fragments are seen; they range from a small fleck to up to 50% of the joint surface, with a variable degree of dorsal subluxation of the middle phalanx. A lateral view in flexion is helpful for assessing the relocation potential of the PIP joint in flexion.
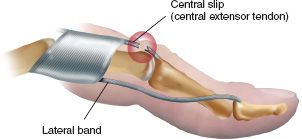
FIGURE 24-10 Central slip injuries, if left untreated, can result in volar displacement of the lateral bands and a boutonnière deformity. Volar dislocations of the PIP joint, although uncommon, can result in central slip injuries. Splinting the PIP joint (not the DIP joint) in extension and encouraging passive DIP flexion is the correct treatment for acute central slip injuries as long as the patient has active PIP joint extension to within 30° of full extension.
• Treatment—Effective treatment modalities may include dorsal extension block splinting, skeletal traction, ORIF, and volar plate arthroplasty.
(a) Closed management—Stable PIP joints in flexion may be managed with dorsal extension block splinting. Full active flexion is allowed; progressively more extension is allowed over 4 weeks. Fracture fragments less than 30% of the articular surface are well suited to this approach.
(b) Surgery
• ORIF—Large fracture fragments involving 50% or more of the joint surface may be repaired with surgery, using a pullout wire, a Kirschner pin, or a compression screw. Pilon fractures with depressed joint surfaces may require elevation, bone grafting, and K-wire stabilization.
• Volar plate arthroplasty—Comminuted fractures may require excision of the volar fragments and advancement of the volar plate to the middle phalanx to restore stability and resurface the damaged articular surface.
• Skeletal traction—With highly comminuted fractures, there may be no option but continuous longitudinal distraction until the fracture has molded.
• Complications—Complications include recurrent subluxation, limited joint motion (hinged motion on a subluxed PIP joint), and posttraumatic arthritis.
D. MCP Joint Injuries
1. Thumb MCP ulnar collateral ligament injury—An injury to the ulnar collateral ligament of the thumb is also known as gamekeeper’s thumb or ski-pole thumb. A competent ulnar collateral ligament of the MCP joint is critical for effective lateral key pinch.
• Evaluation
(a) Examination—Tenderness is noted over the ulnar aspect of the MCP joint. A palpable fullness may suggest Stener’s lesion (interposition of the adductor pollicis aponeurosis between the torn end of the ulnar collateral ligament and the proximal phalanx). Stress testing of the ulnar collateral ligament with radial stress in some flexion should be compared with the opposite noninjured thumb. Stress in some flexion tests the proper collateral ligament. Stress in extension tests the more volar accessory ligament. A poor endpoint in both flexion and extension confirms a complete tear of the ligament, and an unstable joint. A digital block may be required before the examination.
(b) Radiographic evaluation—Radiographs of the thumb should be taken before stress testing to look for associated fractures. Stress radiographs demonstrating more than 35 ° of opening should suggest complete tear of the ligament (Fig. 24-11).
• Treatment
(a) Closed treatment—Partial tears of the ulnar collateral ligament that have good endpoints and do not open 35° with stress can be treated with cast immobilization or with a functional brace with the MCP joint held in slight flexion for 3 to 4 weeks.
(b) Surgery—A complete tear of the ulnar collateral ligament associated with instability of the MCP joint (opening >35° with stress) or a displaced fracture fragment requires surgery to reattach the ulnar collateral ligament. In these cases, Stener’s lesion is usually present and will not heal back to the proximal phalanx without surgery. Operative repair of the ligament can be performed with a suture anchor or a pullout button. Chronic injuries of the ulnar collateral ligament may require ligament reconstruction or advancement of the adductor pollicis to the proximal phalanx.
• Complications—Complications include residual instability with pain, decreased lateral key-pinch strength, volar subluxation of the MCP joint, and late arthritic changes.
2. Thumb MCP radial collateral ligament injury—Injury to the radial collateral ligament of the MCP joint of the thumb is less common. However, the diagnosis is often missed, so treatment may be delayed.

FIGURE 24-11 A thumb MCP ulnar collateral ligament stress test demonstrates significant radial deviation (and angulation) at the thumb MCP joint (as seen on this stress radiograph). (Reprinted with permission from O’Donoghue DH. Treatment of Injuries to Athletes. Philadelphia, PA: WB Saunders; 1986.)
• Evaluation
(a) Examination—There is localized swelling and tenderness on the radial aspect of the thumb MCP joint. Stress testing elicits pain or demonstrates opening on the radial aspect of the joint. Volar subluxation is commonly associated with radial collateral ligament injury of the thumb MCP joint.
(b) Radiographic evaluation—Two views of the thumb are needed to evaluate for an associated fracture. A small osteochondral fracture fragment from the metacarpal is frequently noted.
• Treatment
(a) Cast—Almost all injuries of the radial collateral ligament can be treated conservatively with a cast or thumb spica splint for 4 to 6 weeks if diagnosed acutely. The cast must prevent volar subluxation of the MCP joint.
(b) Surgery—If the MCP joint is unstable or has volar subluxation, surgery to repair the radial collateral ligament may be required. The ligament is usually torn from the metacarpal head and requires repair with a suture anchor or a pullout button.
• Complications—Complications are the same as those listed for thumb MCP ulnar collateral ligament injury.
3. Finger MCP collateral ligament injury—Forced spreading into the web space may result in injury to the radial or ulnar collateral ligament of a finger MCP joint. The collateral ligament at the MCP joint usually fails at its attachment to the proximal phalanx and at times includes an avulsed bone fragment.
• Diagnosis
(a) Examination—Subtle swelling is noted in the web space between the two metacarpal heads. Local tenderness confirms the site of injury. Gentle stress testing to the MCP joint, in both extension and flexion, may reproduce pain or demonstrate instability.
(b) Radiographic evaluation—X-ray films may demonstrate a small avulsion fracture fragment from the metacarpal head.
• Treatment
(a) Closed treatment—The majority of collateral ligament injuries to the MCP joints of the fingers can be treated with conservative management. Buddy-taping of the fingers to protect the collateral ligament of the MCP joint is recommended, with intermittent use of a splint incorporating 50° or more of flexion for unstable injuries. Slow improvement in symptoms may be expected over 3 months.
(b) Surgery—Surgical treatment may be considered for an avulsion fracture fragment that involves 20% of the articular surface or is displaced more than 2 mm. Relative indications for surgical repair include injury to the radial collateral ligament of the index finger or the little finger.
• Complications—Complications include instability, laxity, and weakness or pain. Chronic pain and secondary adhesions are more frequent sequelae than instability, and it is suggested that static splinting should not exceed 3 weeks. Extension contracture may also occur.
4. Dorsal dislocation of the MCP joint—MCP joint dislocations most often occur in a dorsal direction and most commonly involve the index finger, thumb, and little finger. Dorsal dislocation may be simple (reducible) or complex (irreducible).
• Evaluation
(a) Simple dislocation—There is a notable deformity with marked MCP joint hyperextension. X-ray films demonstrate the proximal phalanx at 60° to 90° of hyperextension on the dorsum of the metacarpal head.
(b) Complex dislocation (Fig. 24-12)—Deformity is not as obvious, with the joint only slightly hyperextended. A common finding is a skin dimple (puckering) at the distal palmar crease. Radiographs demonstrate nearly parallel alignment of the proximal phalanx and the metacarpal. The presence of a sesamoid in a widened MCP joint indicates volar plate entrapment.
• Treatment
(a) Simple dislocation—Gentle closed reduction should be performed by hyperextending the joint before pushing the proximal phalanx onto the metacarpal head. Straight longitudinal traction should be avoided because it may convert a simple to a complex dislocation.
(b) Complex dislocation—A single attempt at closed reduction may be performed, but most complex dislocations require open reduction in the operating room. Open reduction can be achieved through either a dorsal or a volar approach and requires extraction of the interposed volar plate. The radial digital nerve may be tented over the index metacarpal head, or the ulnar digital nerve may be tented over the metacarpal head of the little finger, when performing the volar approach. The volar plate can be split longitudinally to assist reduction of the joint if needed. The dorsal approach eliminates the risk of damage to the digital nerves and allows treatment of any associated metacarpal head fracture. After reduction, the MCP joint is typically stable and allows early active range-of-motion exercises with buddy-taping.
(c) Complications—Complications can include digital nerve damage, stiffness, and arthritis (if associated with a metacarpal head fracture).
E. Carpometacarpal (CMC) Joint Injuries
1. Dislocation (and fracture-dislocation) of the CMC joint—The CMC joints of the index, middle, and ring fingers are stable (fixed) joints that allow minimal gliding motion and are classified as arthrodial diarthroses. The CMC joint of the little finger is more mobile and is similar to the thumb CMC joint. As a saddle joint, the CMC joint of the little finger allows motion not only in a gliding but also in rotation to allow its opposability to the thumb. The CMC joints are stabilized by very strong intermetacarpal and CMC ligaments that support the dorsal and volar aspects of the joint. Fracture-dislocation of the CMC joint occurs with severe force. Dislocation is generally in the dorsal direction (unless the dislocation results from a direct blow from the dorsal direction, causing a volar CMC dislocation). Volar dislocations are much rarer than dorsal dislocations but are relatively more common in the CMC joint of the little finger because of its increased mobility.
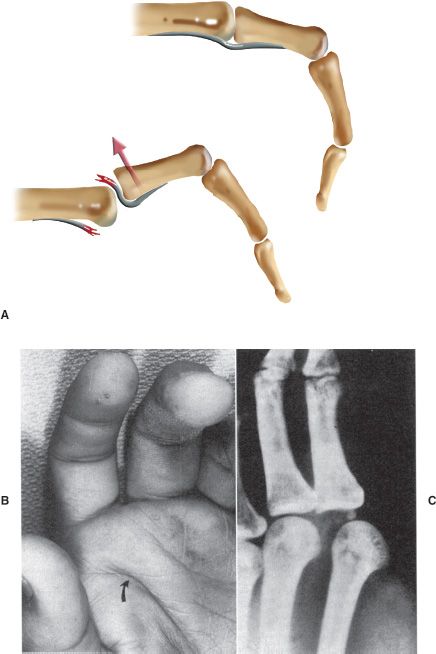
FIGURE 24-12 Complex dorsal dislocation of the MCP joint. A. Diagram demonstrating how the volar plate can become displaced dorsally, blocking reduction of the MCP joint dorsal dislocation. B. Clinical photograph demonstrating puckering (arrow) of the palmar skin. C. Radiograph showing entrapment of a sesamoid within the (widened) MCP joint. (B and C reprinted with permission from Green DP, Strickland JW. In: DeLee JC, Drez D Jr, eds. Orthopaedic Sports Medicine: Principles and Practice. Philadelphia, PA: WB Saunders; 1994.)
• Evaluation—Because of the overlap of the adjacent bone structures, X-ray interpretation of the CMC joint is often difficult, and various views are required for accurate interpretation. Radiographs demonstrate a subluxated or dislocated CMC joint (with or without a fracture fragment involving the CMC joint surface) (Fig. 24-13). Computed tomography (CT) may be indicated for more difficult diagnostic problems. A 30° pronated view of the hand may be necessary for assessing the congruency of the joint surfaces.
• Treatment—Closed reduction is easily obtained with longitudinal traction but cannot be maintained in a cast alone. Percutaneous transarticular K-wire fixation, in addition to cast immobilization, is necessary. Redislocation or incomplete reduction of the CMC joint often occurs in index- and little-finger CMC fracture-dislocations as a result of the pull of the extensor carpi radialis longus tendon to the index metacarpal and the extensor carpi ulnaris to the metacarpal of the little finger. Closed reduction and cast immobilization often result in recurrence of the CMC dislocation because of the instability and significant swelling that occur with these injuries.
• Complications—Complications include recurrent dislocation, pain, weakness, and arthritis. Posttraumatic arthritis of the CMC articulation can be effectively treated with arthrodesis.
II. Fractures of the Hand—Phalangeal and metacarpal fractures are common, comprising nearly 10% of all fractures.
A. Phalangeal Fractures
1. Classification—Extra-articular phalangeal fractures are described by location, including base, shaft, or neck for the middle and proximal phalanges, as well as tuft fracture for the distal phalanx. These injuries may be further described as displaced or nondisplaced, as open or closed, as associated with a rotational or angular deformity; they may have associated injuries to the skin, nerve, digital artery, or tendons.
2. Deforming forces—The bony anatomy is an intercalated osseous chain. Fracture of a phalanx in this chain results in a predictable deformity.
• Middle phalanx
(a) Fracture proximal to flexor digitorum superficialis (FDS) insertion causes the middle phalanx to angulate dorsally.
(b) Fracture distal to the FDS insertion causes the middle phalanx to angulate volarly.
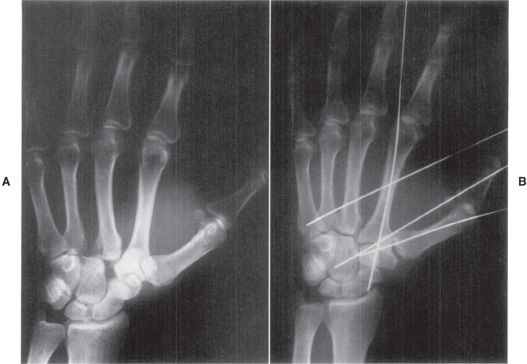
FIGURE 24-13 A. Injury film showing dislocation of the CMC joint of the index and long fingers. B. Postoperative film after reduction of the dislocations and stabilization with Kirschner wires.
• Proximal phalanx—Interosseous attachments to the proximal phalanx flex the proximal fragment, whereas the central slip extends the distal portion, resulting in volar angulation at the fracture.
3. Evaluation—Swelling, pain, limited motion, or deformity should suggest fracture and merit radiographic evaluation. Some 30% of phalangeal fractures may be open. Associated flexor tendon or digital nerve injuries should be identified. Nonunion and infection rates are higher with open fractures. A splay lateral X-ray study of the digits with various amounts of flexion is required to prevent overlap of the phalanges during radiographic examination.
4. Treatment
• General principles—Accurate fracture reduction is recommended, followed by remobilization of the injured finger as early as allowed by fracture stability. Uninvolved fingers should be mobilized early to prevent stiffness. The PIP joint is the most important joint for motion and function of the digit.
• Stable fractures—Stable phalangeal fractures with good radiographic alignment can be treated with buddy-tape, a splint, or a cast. X-ray studies should be repeated in 7 to 10 days.
• Displaced fractures—Displaced fractures that can be reduced and converted to a stable position can be treated with closed management, including a cast or splint, followed by protected range-of-motion exercises. Percutaneous pinning may be necessary to prevent fracture displacement.
• Unstable fractures—Fractures that cannot be reduced or have persistent instability despite attempted closed reduction require ORIF with skeletal fixation. Treatment options include K-wire fixation, intraosseous wiring, interfragmentary screws, and plate and screw fixation.
• Segmental bone loss—Segmental bone loss is frequently associated with a severe soft-tissue injury. Primary treatment should include soft-tissue management with thorough irrigation and debridement, followed by open packing. These fractures are typically highly comminuted and may require external fixation to maintain length until definitive bony reconstruction can be performed with bone graft. Delayed flap coverage may be required as well.
5. Complications
• Loss of motion—Close adherence of the flexor and extensor tendons over the phalanges may lead to tendon adhesions to the bone. Tenolysis may be required to improve motion after fracture healing. PIP flexion contracture is also common with phalangeal fractures. If not improved with therapy, joint release may be required.
• Malunion—A closing wedge osteotomy of the phalanx may be needed to correct an angular deformity. Rotational deformity with overlap of the digits may require a transverse derotational osteotomy of the phalanx.
• Infection
• Nonunion
• Symptomatic hardware—Exposed K-wires may be complicated by superficial pin-tract infection. Plate and screw fixation for a phalangeal fracture is often complicated by symptomatic hardware, requiring delayed removal after fracture healing, with tenolysis of the extensor mechanism.
B. Metacarpal Fractures—Metacarpal fractures account for 36% of all fractures of the hand.
1. Classification—Metacarpal fractures are described by location, including metacarpal head fractures, metacarpal neck fractures, metacarpal shaft fractures, and metacarpal base fractures. These fractures are typically further described as nondisplaced or displaced, as closed or open, or as associated with angulation, rotation, or a shortening deformity.
2. Evaluation—X-ray studies define fracture alignment. The Brewerton X-ray view is particularly useful for evaluating metacarpal head fractures.
3. Treatment
• Metacarpal head fractures—Nondisplaced metacarpal head fractures can be treated with cast protection or buddy-taping. Displaced oblique fractures require ORIF with K-wires or small screws. Small osteochondral fractures may be excised. Avascular necrosis of the metacarpal head may occur after even a nondisplaced transverse fracture.
• Metacarpal neck fractures (Fig. 24-14)—Metacarpal neck fractures are also referred to as boxer, fighter, or frustration fractures. A direct blow on the metacarpal head of the little or ring finger may result in fracture with angulation at the metacarpal neck. If angulated less than 15°, the fracture can be treated in an ulnar gutter splint for 2 weeks, followed by range-of-motion exercises. If angulated 15° to 40°, the fracture should be reduced, followed by ulnar gutter splint treatment. If angulated more than 40° with unacceptable clinical deformity, closed reduction and percutaneous pinning of the fracture is recommended. A total of 40° of dorsal angulation for a fracture of the metacarpal neck of the little finger can be accepted, with good resulting function, because of the compensatory motion at this metacarpal’s CMC joint. Residual angulation greater than 15° for metacarpal neck fractures of the index and long fingers is unacceptable because of the lack of compensatory CMC motion for these metacarpals.
• Metacarpal shaft fractures—Transverse metacarpal shaft fractures are often caused by a direct blow, resulting in dorsal angulation. These fractures are often amenable to closed reduction, followed by cast treatment. Spiral and long oblique fractures of the metacarpal shaft are inherently unstable with shortening and rotation. Rotational deformity manifests as overlap of the digits when making a fist (Fig. 24-15). ORIF is recommended for metacarpal shaft fractures with (a) malrotation, (b) dorsal angulation greater than 10° for the index and long finger metacarpals, (c) dorsal angulation greater than 20° for the ring and little finger metacarpals, and (d) any shortening greater than 3 mm. Multiple displaced metacarpal shaft fractures are an indication for internal fixation as well. Treatment options may include K-wires, interosseous wiring, interfragmentary screws, and screws and plates. Long oblique and spiral fractures are well suited to interfragmentary screw fixation. Short oblique and transverse fractures require a neutralization plate and screw fixation (Fig. 24-16). Open metacarpal fractures require treatment of the associated soft-tissue injuries and may require external fixation if highly comminuted or associated with segmental bone loss (Fig. 24-17).

FIGURE 24-14 Boxer’s fracture of the metacarpal neck of the little finger. (Reprinted with permission from Gartland JJ. Fundamentals of Orthopaedics. 4th ed. Philadelphia, PA: WB Saunders; 1987.)
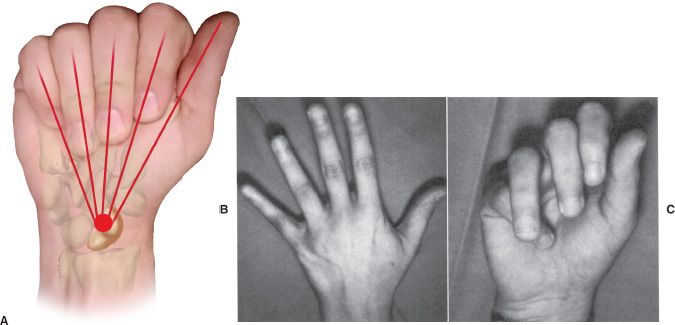
FIGURE 24-15 Assessment for rotational deformity of the fingers. A. Normally, the four flexed fingers converge at the scaphoid tubercle, and the nails are aligned. B. Rotational malalignment cannot be appreciated with the fingers extended. C. Same patient as in (B) with the fingers flexed. Note malrotation of the ring finger. (B and C reprinted with permission from Culver JE, Anderson TE. Clin Sports Med. 1992;11:101–128.)
• Metacarpal base fractures—Stable metacarpal base fractures can be treated with a cast alone. Displaced metacarpal base fractures require closed reduction and percutaneous pinning.
4. Complications
• Malunion—Dorsal angulation of a metacarpal shaft fracture may disturb the intrinsic or extrinsic tendon balance. Dorsal closing wedge osteotomy or volar opening wedge osteotomy may be necessary to correct this angular deformity. Derotational osteotomy through the base of the metacarpal corrects a rotational deformity. Other complications include nonunion, MCP joint contractures, intrinsic muscle contractures, and refracture.
C. Fractures at the Base of the Thumb Metacarpal—Fractures at the base of the thumb metacarpal can impair effective lateral key pinch and opposition of the thumb to the other digits.
1. Classification (Fig. 24-18)
• Bennett’s fracture—dislocation
• Rolando’s Y or T condylar fracture
• Epibasal fracture
• Comminuted fracture
2. Evaluation
• Clinical examination—There is swelling and pain at the base of the thumb, often with bruising in the thenar region.
• Radiographic evaluation—AP, lateral, and oblique views are obtained. Oblique views are necessary to assess for congruency of the CMC joint.
3. Treatment
• Nondisplaced fractures—Nondisplaced well-aligned fractures can be treated with a cast for 4 weeks, followed by a removable splint.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







