2
Indications and Techniques for Meniscus Repair
The important functions of the meniscus have led to efforts to repair rather than resect the torn meniscus. The ability of the vascular region of the meniscus to heal is well established; furthermore, it is known that meniscal cells can proliferate and synthesize matrix proteins, providing further impetus for efforts to repair the torn meniscus. Most evidence supports repair over removal of meniscal tissue whenever possible.1, 2 Although there are several techniques of meniscus repair, the most important factor for a successful outcome is identifying those tears with good healing potential. The most important factor is the location of the tear, as tears in the vascular periphery have the potential to heal.
Indications
Several characteristics should be evaluated to determine the reparability of a torn meniscus, including tear location, chronicity, patient age, meniscal tissue quality, joint stability, and type of tear.3 The peripheral 25 to 30% of the meniscus is vascularized (the “red” zone) and can mount a healing response to injury, whereas tears in the inner, avascular (“white”) zones remain more difficult to treat (Fig. 2–1). Most studies demonstrate higher healing rates for lateral meniscus repairs compared with repairs of the medial meniscus, and thus, the lateral meniscus may have broader indications for repair.4–7 Axial valgus or varus deformity may play a role in atraumatic lateral and medial meniscal tears, respectively, and may affect healing due to increased loads in the affected compartment.8
Meniscus repair with concomitant anterior cruciate ligament (ACL) reconstruction results in higher rates of meniscal healing compared with patients undergoing isolated meniscus repair.3, 6, 7, 9 It is likely that the hemarthrosis associated with ACL reconstruction provides serum-derived growth factors to the healing meniscus tear that improve healing. In addition, because the medial meniscus is a secondary restraint to anterior tibial subluxation in the ACL-deficient knee, persistent knee instability likely results in excessive shear loads on the medial meniscus. Concomitant ACL reconstruction thus is recommended with meniscal repairs in the ACL-deficient knee, and more aggressive attempts at meniscal repair may be considered with ACL reconstruction.2, 10
Meniscus tears that occur as an isolated injury without major trauma may occur in the setting of intrameniscal degeneration, and successful repair is probably less predictable in these types of tears. Single vertical longitudinal tears heal most successfully after repair compared with more complex tears.11 Patient age may also influence treatment as there is an increased prevalence of mucoid degeneration and gradual decreases in meniscal blood flow in older individuals. However, successful repairs have been reported in patients over 50 years of age.2, 4, 11
Some tears, such as partial-thickness injuries, shallow radial tears, and tears that are stable when probed, may require nothing more than rasping for induction of a bleeding bed for healing. Full-thickness or nearly full-thickness vertical tears greater than 1 cm in length are strong indications for repair. Smaller tears that are seen during ACL reconstruction, particularly of the lateral meniscus, can be left in situ with successful clinical outcome in most cases.12 Acute bucket-handle tears are often reparable, though chronic tears may be deformed and fragmented and may require partial meniscectomy.
Surgical Technique
There are various techniques for meniscal repair, including open and arthroscopic. These different techniques each have specific advantages and pitfalls. Although open meniscal repair procedures have been utilized historically, arthroscopic techniques have gained favor because of smaller incisions and better access to most tear patterns. Open procedures are still utilized for some peripheral tears, such as meniscocapsular detachment.13
Outside-In Technique
The outside-in technique has proved especially useful for suturing meniscal tears in the anterior horn and body segment of the meniscus.14 Visualization is also unimpeded as no instruments are placed between the arthroscope and the meniscal tear. The outside-in technique is also advantageous in smaller knees, such as for repair of a Wrisberg-type discoid meniscus in children. Furthermore, this technique may be used to secure a synthetic collagenous meniscal replacement, meniscal allograft, or fibrin clot into the tear site. For example, by placing a suture across the tear, attaching the fibrin clot to the suture, and maneuvering the clot inside the knee, the surgeon has a reliable method to secure a fibrin clot to the tear site.
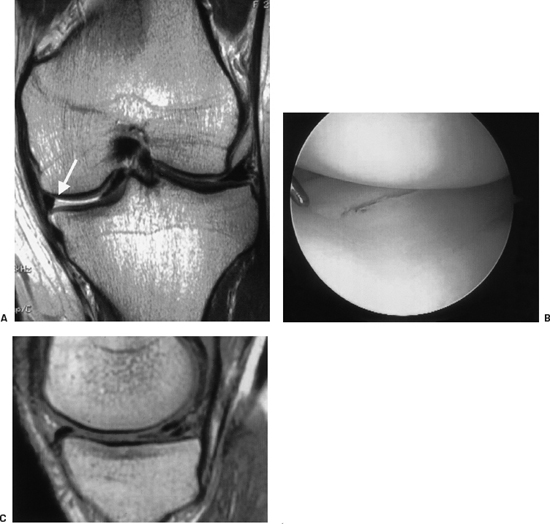
Figure 2-1 Magnetic resonance image of a repairable vertical longitudinal meniscus tear at the “red-white” junction (arrow).
Since it is likely that sutures placed obliquely across a tear may not effectively coapt the tear, the use of the outside-in technique for far posterior tears of the meniscus (near the tibial attachment) is not advocated because of difficulty placing the needle perpendicular to the tear in that location. Inside-out or all-inside techniques are recommended for meniscal tears adjacent to the posterior horn attachment site.
Outside-In Technique for Medial Meniscus Repair
An anterolateral viewing portal is used, and a posterior portal may be used for rasping the tear site. This portal is made proximal and posterior to the medial joint line, anterior to the pes anserinus tendons and saphenous nerve with the knee flexed. Valgus load facilitates repair by opening the medial compartment and approximating the capsule to the meniscus while passing the repair needles across the tear. The outside-in technique is performed by passing an 18-gauge spinal needle across the tear (Fig. 2–2). While viewing the meniscus arthroscopically, the first needle enters the joint from the outside, passing across the meniscal tear, piercing the femoral or tibial surface of the meniscus. The second needle is passed into the meniscus before passing the sutures to avoid cutting a previously placed suture with the second needle. A rigid suture (No. 0 polydioxanone) is then passed into the needle and retrieved inside the joint with an arthroscopic grasper.
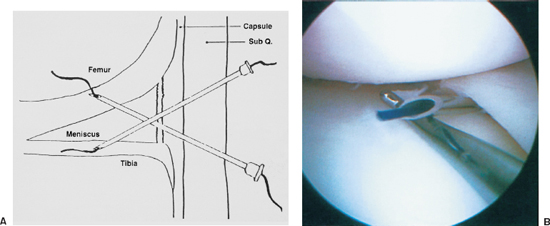
Figure 2-2 Outside-in meniscus repair is started by placement of spinal needles across the tear, with the needles entering into the joint under direct visualization. Sub Q, subcutaneous layer.
The authors use absorbable No. 0 polydioxanone suture (PDS, Ethicon, Somerville, NJ). The suture is placed into each needle, grasped inside the joint, and pulled out through the anterior portal. The adjacent sutures are pulled outside the joint through a 7 mm-diameter cannula through the anteromedial portal to prevent entrapment of the sutures in soft tissue. Each suture is then tied into single standard mulberry knots (Fig. 2–3), or the two exiting sutures are tied together and the knot is shuttled by pulling one limb from the medial side of the knee to exteriorize the knot, forming a horizontal or vertical mattress suture (Fig. 2–4). The sutures are then pulled into the joint to lie against the meniscus. The free ends of the pair of sutures should be clamped together until all sutures have been passed and collected outside the joint. The next set of sutures is passed about 4 mm away from the first pair.
Commercially available wire cable loops (Instrument Maker, Kalamazoo, MI) aid in placing mattress sutures without the need to pull sutures out through the anterior portal and also allow the use of braided suture. The wire cable loop is placed through the cannulated needle, and a suture is then placed into the loop inside the joint. The wire cable loop is then pulled out the cannulated needle. A simple PDS suture can also be used to place a braided suture by placing the PDS suture through the tear as described above, bringing this suture outside, and then tying the desired permanent suture to the PDS and pulling both sutures back into the joint across the tear. Adjacent permanent sutures are then tied together, and the knot is pulled back through the meniscus, resulting in a mattress suture.
Once the appropriate starting location on the outside of the knee is identified and the initial needle is placed across the tear, a 10 to 15 mm incision in the skin is made, and dissection is carried down to the capsule. It is imperative to identify, via transillumination if necessary, the saphenous nerve and vein on the medial side. All subsequent passes of the needle should be made through this incision if possible. If the tear extends far anteriorly, a second incision may be required more anteriorly. The tear is reduced, and adjacent sutures are then tied together subcutaneously over the capsule with the patient’s knee in full extension.
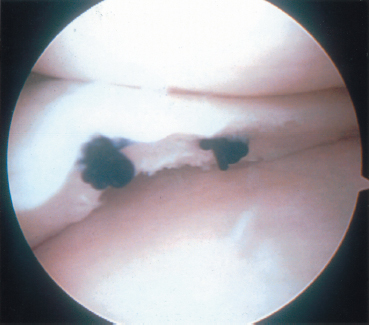
Figure 2-3 One way to secure the sutures involves using a knot at the end of the suture. After this knot is tied at the end of the suture, the suture is pulled back through the knee so that the knot lies against the meniscus. Adjacent sutures are tied together over the capsule outside the joint, reducing the meniscus tear.
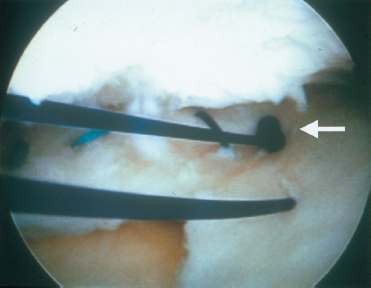
Figure 2-4 Outside-in sutures may be tied together to create a mattress suture. In this figure the knot holding the two sutures together is being pulled back through the meniscus to leave a mattress suture.
Outside-In Technique for Lateral Meniscus Repair
The basic procedure for lateral meniscal repair using the outside-in technique is similar to medial meniscus repair. Access to the posterolateral joint line is achieved by placing the patient’s leg in the position shown in Fig. 2–4, with an externally rotated hip and a flexed knee. The position shown in Fig. 2–4 also places varus force across the knee, opening the lateral compartment slightly, thereby improving access to the meniscus. The needles should always remain anterior to the biceps tendon with the knee at 90 degrees of flexion to avoid peroneal nerve injury, as the nerve falls posterior to the joint line in this position. Viewing is accomplished through either anterior portal. Placement of the arthroscope in the anteromedial portal allows visualization of the anterior aspect of the lateral meniscus. As with medial repair, the site of the tear is carefully rasped. An accessory posterolateral portal for rasping can be made posterior and proximal to the joint line and anterior to the biceps tendon with the knee flexed. The sutures are retrieved through an anterolateral portal and can be secured as described for medial meniscus repair. Placing sutures through the popliteus tendon is not recommended, although we have not seen any problems if this is done with absorbable suture. One must protect the inferior lateral geniculate artery coursing along the posterolateral joint line when making the incision to dissect down to the capsule to tie the sutures.
Inside-Out Technique
The inside-out technique is especially useful for posterior horn tears that are close to the tibial attachment, because this technique allows predictable placement of perpendicular sutures across the tear. Care must be taken to diminish the risk of scraping the articular surfaces with the rigid zone-specific cannula. Both single- and double-lumen cannulas can be used. The single-lumen is more maneuverable and easier to bend. Single-lumen cannulas also offer better placement of vertical sutures in small knees, but there is a risk of damaging the suture in the cannula when the second needle is passed. The inside-out technique also requires a posterior incision for retractor placement to protect the neurovascular structures.
The tear edges are debrided and prepared as described above for the outside-in technique. For medial meniscus repair, an accessory 4 cm longitudinal incision is made centered one third above the joint line and two thirds below the joint line with the knee in 90 degrees of flexion. The incision crosses the joint line posterior to the medial collateral ligament and is taken down to the sartorius fascia. The knee is then placed in slight flexion. The sartorius fascia is incised and the pes tendons retracted posteriorly along with the semimembranosus. The saphenous nerve and vein will lie posterior to the incision in this position. Dissection is then performed in the plane between the gastrocnemius tendon and the capsule (Fig. 2–5).
For posterior horn tears, the suture cannula enters the joint through the contralateral portal. Suture needles are advanced 3 to 4 mm beyond the cannula tip, pierced into the meniscus, and then advanced across the tear and out the capsule through the accessory incision. Vertical mattress sutures 4 to 5 mm apart are recommended. Caution must be used in placing the sutures the proper distance from the tear. Sutures too close to the tear margin can result in the suture pulling through the tear, and sutures too far away can pucker the meniscus. As with the out-side-in technique, the sutures are tied with the knee in extension after all have been passed. The meniscus is carefully probed to ensure that tight apposition was achieved. The sutures are tied over the capsule, and the incisions are closed.
The protocol for lateral meniscus repair includes knee flexion to 90 degrees, with the incision made just posterior to the lateral collateral ligament at the level of the joint line. The interval between the iliotibial band and the biceps tendon is developed. The interval between the capsule and the lateral head of the gastrocnemius must then be exposed (Fig. 2–5). It is generally easier to elevate the lateral head of the gastrocnemius off the posterolateral capsule by beginning the dissection slightly distal to the joint line. The retractor is placed in this space to again protect the posterior neurovascular structures. The repair then continues as above.
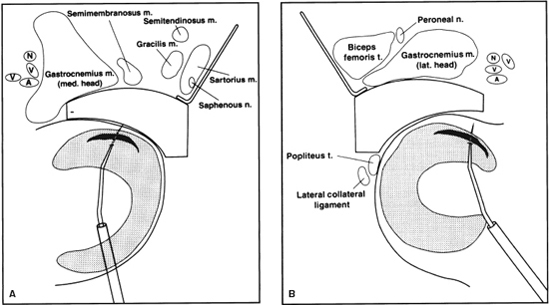
Figure 2-5Placement of a posterior retractor for insideout repair of the medial meniscus. The incision is made just posterior to the medial collateral ligament at the level of the joint line. The retractor is placed in the interval between the gastrocnemius tendon and the capsule, with the pes tendons retracted posteriorly. A posterior retractor for repair of the lateral meniscus is placed posterior to the lateral collateral ligament, with the knee in flexion to allow the peroneal nerve to fall posteriorly. Dissection is performed anterior to the biceps tendon to avoid injury to the peroneal nerve.
All-Inside Technique
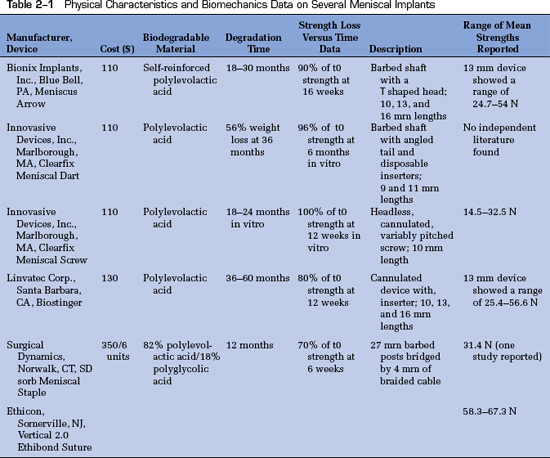
Implants and techniques for the all-inside technique continue to evolve as numerous implants, biodegradable and permanent, become available. The benefit of the all-inside technique is that no ancillary posterior incision is required, decreasing the risk of posterior neurovascular injury. The technique is especially appropriate for posterior horn vertical tears adjacent to the tibial insertion site of the meniscus.15 The earliest meniscal repair implants were single “fastener” types, whereas newer implants employ sutures. Despite the lack of long-term follow-up studies demonstrating their efficacy, all-inside implants are often used because of their technical ease of application. Table 2-1 summarizes the materials, degradation time, and strength profiles of several commonly used implants.
In addition to the absence of long-term studies, each type of implant carries short-term risks. Implant devices should not be left prominent, as this may cause irritation of chondral surfaces.16–18 Cases of implant failure have been reported with subcutaneous fragment migration and prominence, persistent effusion, and loss of fixation and implant breakage, perhaps due to uneven implant resorption.19–22 The best-studied meniscal repair implant is the Bionix Meniscal Arrow (Bionix Inc., Blue Bell, PA). Aseptic synovitis, cystic hematoma, and inflammatory foreign-body reactions have also been reported following the use of the meniscus arrow.23–25 Thus, although biodegradable implants are appealing due to their relative ease of use, given the lack of long-term studies available, the higher costs of these implants, and the potential complications, vertical mattress sutures may still provide the best option for meniscus repair. The arrow, which comes in 10, 13, and 16 mm lengths, can be used in the anterior, middle, and posterior thirds of the meniscus, respectively. The arrow length that best fits the tear location is placed into the cannula oriented parallel to the joint line and perpendicular to the tear. The arrow is tapped into place with a mallet to ensure that the arrow has been completely countersunk. The next arrow shaft should be placed no closer than 5 mm from the first. The number of arrows should roughly correlate to the number of sutures that would be used. Placing arrows on the tibial surface of the meniscus is challenging and not recommended.
Newer all-inside devices are available using sutures, including the Fast T-Fix (Smith and Nephew, Andover, MA) and the RapidLoc (Mitek, Norwood, MA). These devices have a small bar that is placed across the meniscus tear, exiting on the extraarticular side of the meniscus. This bar catches the capsule outside the joint and thus attains fixation on the extraarticular side of the meniscus. There is a suture attached to this bar, and the Fast T-Fix device has a pre-tied knot that slides down to the meniscus surface, achieving fixation. The RapidLoc implant has a small device (“top hat”) that slides down the suture to the meniscus surface, achieving fixation of the tear.
Postoperative Care
The most important factors to consider in tailoring a rehabilitation protocol include (1) weight-bearing status, (2) range of motion allowed, and (3) the timing for return to high-impact activities. Meniscal repair rehabilitation protocols from the senior author’s institution consist of the use of (1) a double-upright hinged brace to allow 0- to 90degree range of motion, (2) early weight bearing in full extension, (3) weight bearing without the brace beginning at 4 to 6 weeks, and (4) no high-impact athletics for 4 months.1 Still, rehabilitation programs for meniscal repairs should be individualized. One exception, however, to prescribing early weight bearing in extension would be a radially oriented tear where weight bearing may potentially cause distraction at the tear site. Axial malalignment may also increase stress in one compartment, and a less accelerated program should be considered in these cases (i.e., lateral meniscal repairs in a valgus knee). Progressive flexion over 90 degrees places higher stress on the menisci and should be avoided in the early postoperative period. Flexion should be limited to 90 degrees during the first month and slowly increased thereafter to protect posterior horn repairs. Early full extension is emphasized. Full weight bearing with a fully extended, locked brace is allowed immediately for bucket-handle and vertical longitudinal tears. Closed-kinetic-chain strengthening exercises are begun after 2 weeks and gradually increased as strength develops. At 4 weeks, the brace can be removed to allow walking range of motion, and running can be resumed as tolerated 3 to 4 months postoperatively. If ACL reconstruction is undertaken with the meniscal repair, the usual ACL repair protocol is followed, perhaps with limitations of flexion and delayed weight bearing after repair of radial tears as described previously.26
Tips and Tricks
When using the outside-in technique, it is helpful to use a probe on the meniscus to keep the meniscus reduced against the capsule to prevent the entering needle from displacing the meniscus into the joint. The tip of the needle also may strike the tibial articular surface as it enters the joint; using a probe to hold up the needle tip prevents this. When using the outside-in technique to place two adjacent sutures that will be used to create a mattress suture, these two sutures should be pulled out through a cannula in an anterior portal; otherwise, soft tissue can become entrapped between the two limbs and prevent the sutures from being pulled back into the joint. When making the posterior incision for inside-out repair, ankle dorsiflexion can be used to verify the location of the gastrocnemius tendon. This posterior incision and exposure should be made slightly below the joint line, because the needles tend to be directed inferiorly as they exit the joint. It is occasionally helpful to release a small amount of the semimembranosus insertion to the proximal tibia to improve exposure on the medial side. With either suture technique, vertical mattress sutures on the femoral and tibial sides of the meniscus are recommended because of their superior strength, as vertically oriented sutures are better able to capture the circumferentially oriented collagen fibers of the meniscus (Fig. 2–6). Placing a vertically oriented suture with the inside-out technique is often easier using a single-lumen cannula, because the wider, double-lumen cannula is sometimes too big to turn into a vertical orientation in a tight posterior compartment.
When concomitant ACL reconstruction is performed with meniscal repair, the meniscal repair sutures are placed first but are not tied until the ligament graft is secured. When repairing a large bucket-handle tear, the first suture should be placed in the middle of the handle fragment to reduce the tear, with subsequent sutures placed anterior and posterior to this first suture. Radially oriented tears are best reduced with a purse-string suture orientation, with one suture placed on each side of the tear. Ideally, all sutures enter near the inner edge of the meniscus, and one set of purse-string sutures is placed on the superior surface and one on the inferior surface.
Consideration should also be given to methods to improve the vascularity of the tear site. Abrasion of the adjacent synovium may help stimulate a healing response. Trephination is a technique to create “vascular access” channels using an 18-gauge needle placed into the peripheral meniscus to bring feeding vessels into an avascular meniscal lesion.27–29 However, to make large-enough channels, the meniscus’s circumferentially organized collagen fibers may be disrupted, resulting in weakening of the meniscus. Another method that has been tested and employed extensively in patients and that may extend the indications for meniscal repair is fibrin clot insertion at the tear site. The clot introduces growth factors and cytokines and may act as an angiogenic scaffold for the healing wound. The clot is prepared from 30 to 40 mL of the patient’s blood. Tying the clot to one or two previously placed sutures that have been brought out the anterior portal through a cannula will allow the surgeon to simply pull the clot back into the knee through the cannula. A large cannula without a diaphragm is used.
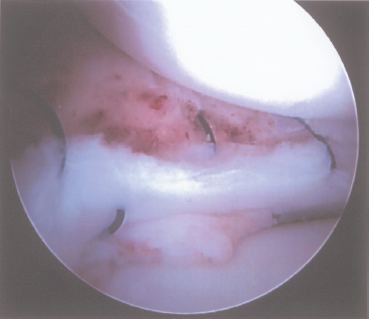
Figure 2-6A vertical mattress suture pattern is recommended. In this figure, vertical sutures have been placed for repair of a Wrisberg-type discoid lateral meniscus in a young child.
Pitfalls and How to Avoid Them
Perhaps the most important factor in arthroscopic meniscus repair is to avoid injury to neurovascular structures. On the medial side, maintaining the knee near full extension and passing the needle posterior to the semitendinosus tendon diminishes the likelihood of injury to the saphenous vein and nerve as well as to their infrapatellar branches. On the lateral side the needles entering from outside-in must remain anterior to the biceps tendon to avoid the peroneal nerve. When using the outside-in technique, be sure to retrieve each pair of sutures through a cannula in the anterior portal, or else soft tissue outside the portal may become entrapped and prevent the ability to pull the sutures back into the joint. With either the outside-in or the inside-out technique, adjacent sutures of a pair should not be placed too close together, or else the suture may pull through the meniscus, resulting in loss of fixation. The most important precaution when using an all-inside technique is to be sure the implant is not prominent on the meniscal surface to avoid articular surface injury. Motion loss can be prevented by tying the sutures with the knee in full extension in an effort to avoid inadvertent capture of the joint capsule.
Future Directions and Conclusion
Meniscal repair is an area of ongoing study. One of the most promising areas of development involves meniscal replacement with either allograft or synthetically engineered tissues. Allograft replacement may be particularly appropriate for restoring the meniscus cartilage in knees that previously underwent total meniscectomy or those with degenerative or complex radial tears that would require near-total meniscectomy.2, 30–34 The authors advocate the use of the outside-in technique for securing the anterior horn of meniscal allografts and the inside-out technique for the posterior aspect. All-inside implants are not currently recommended for securing a meniscus transplant.
Collagen scaffolds that aid regrowth of meniscal cartilage, gene therapy techniques, and meniscal glues are all currently in testing phases.35, 36 Although there are encouraging results thus far, at this time we must await further studies. Meniscal repair techniques will continue to evolve as we learn more about the underlying biology of meniscus healing, with the potential in the future to use biologic agents to enhance healing. Similarly, advances in implants and biomaterials will lead to improved techniques for meniscus repair.
References
1 Koski JA, Ibarra C, Rodeo SA, Warren RF. Meniscal injury and repair: clinical status. Orthop Clin North Am. 2000;31:419–436
2 Noyes F, Barber-Westin S. Arthroscopic repair of meniscus tears extending into the avascular zone with or without anterior cruciate ligament reconstruction in patients 40 years of age and older. Arthroscopy 2000;16:822–829
3 Cooper D, Arnoczky S, Warren R. Arthroscopic meniscal repair. Clin Sports Med 1990;9:589–607
4 Barrett G, Field M, Treacy S, et al. Clinical results of meniscus repair in patients 40 years and older. Arthroscopy 1998;14:824–829
5 Eggli S, Wegmuller H, Kosina J, et al. Long-term results of arthroscopic meniscal repair: an analysis of isolated tears. Am J Sports Med 1995;23:715–720
6 Morgan C, Wojtys E, Casscells C, Casscells S. Arthroscopic meniscal repair evaluated by second-look arthroscopy. Am J Sports Med 1991;19:632–637
7 van Trommel M, Simonian P, Potter H, Wickiewicz T. Different healing rates with the outside-in technique for meniscal repair. Am J Sports Med 1998;26:446–452
8 Habata T, Ishimura M, Ohgushi H, et al. Axial alignment of the lower limb in patients with isolated meniscal tear. J Orthop Sci 1998;3:85–89
9 Barber F, Click S. Meniscus repair rehabilitation with concurrent anterior cruciate reconstruction. Arthroscopy 1997;13:433–437
10 Arnoczky S. Building a meniscus. Biologic considerations. Clin Orthop Relat Res 1999;367 (suppl): S244–S253
11 Rubman M, Noyes F, Barber-Westin S. Arthroscopic repair of meniscal tears that extend into the avascular zone. A review of 198 single and complex tears. Am J Sports Med 1998;26:87–95
12 Fitzgibbons R, Shelbourne K. “Aggressive” nontreatment of lateral meniscal tears seen during anterior cruciate ligament reconstruction. Am J Sports Med 1995;23:156–159
13 DeHaven KE, Arnoczky SP. Meniscus repair: basic science, indications for repair, and open repair. Instr Course Lect 1994;43:65–76
14 Rodeo S. Arthroscopic meniscal repair with use of the outside-in technique. Instr Course Lect 2000;82:49:195-206
15 Hurel C, Mertens F, Verdonk R. Biofix resorbable meniscus arrow for meniscal ruptures: results of a 1-year follow-up. Knee Surg Sports Traumatol Arthrosc 2000;8:46–52
16 Anderson K, Marx R, Hannafin J, et al. Chondral injury following meniscal repair with a biodegradable implant. Arthroscopy 2000;16:749–753
17 Ross G, Grabill J, McDevitt E. Chondral injury after meniscal repair with bioabsorbable arrows. Arthroscopy 2000;16:754–756
18 Seil R, Rupp S, Dienst M, et al. Chondral lesions after arthroscopic meniscus repair using meniscus arrows. Arthroscopy 2000;16:E17
19 Calder S, Myers P. Broken arrow: a complication of meniscal repair. Arthroscopy 1999;15:651–652
20 Ganko A, Engebretsen L. Subcutaneous migration of meniscal arrows after failed meniscal repair. Am J Sports Med 2000;28:252–253
21 Oliverson T, Lintner D. Biofix arrow appearing as a subcutaneous foreign body. Arthroscopy 2000;16:652–655
22 Sims W, Simonian P. Delayed degradation of bioabsorbable meniscal fixators. Arthroscopy 2001;17:E11
23 Hechtman K, Uribe J. Cystic hematoma formation following use of a biodegradable arrow for meniscal repair. Arthroscopy 1999;15:207–210
24 Menche D, Phillips G, Pitman M, et al. Inflammatory foreign-body reaction to an arthroscopic bioabsorbable meniscal arrow repair. Arthroscopy 1999;15:770–772
25 Song E, Lee K, Yoon T. Aseptic synovitis after meniscal repair using the biodegradable meniscus arrow. Arthroscopy 2001;17:77–80
26 Buseck M, Noyes F. Arthroscopic evaluation of meniscal repairs after anterior cruciate ligament reconstruction and immediate motion. Am J Sports Med 1991;19:489–494
27 McAndrews P, Arnoczky S. Meniscal repair enhancement techniques. Clin Sports Med 1996;15:499–510
28 Shelbourne K, Rask BP. The sequelae of salvaged nondegenerative peripheral vertical medial meniscus tears with anterior cruciate ligament reconstruction. Arthroscopy 2001;17:270–274
29 Zhang Z, Arnold JA, Williams T, et al. Repairs by trephination and suturing of longitudinal injuries in the avascular area of the meniscus in goats. Am J Sports Med 1995;23:35–41
30 Ibarra C, Koski JA, Warren RF. Tissue engineering meniscus cells and matrix. Orthop Clin North Am 2000;31:411–418
31 Menetrey J, Jones D, Ernlund L, et al. Posterior peripheral sutures in meniscal allograft replacement Arthroscopy 1999;15:663–668
32 Rodkey WG, Steadman JR, Li ST. A clinical study of collagen meniscus implants to restore the injured meniscus. Clin Orthop Relat Res 1999;367S:S281–S292
33 Stollsteimer G, Shelton W, Dukes A, et al. Meniscal allograft transplantation: a 1- to 5-year follow-up of 22 patients. Arthroscopy 2000;16:343–347
34 Sweigart M, Athanasiou K. Toward tissue engineering of the knee meniscus. Tissue Eng 2001;7:111–129
35 Glossop N, Jackson R, Koort H, et al. The excimer laser in orthopaedics. Clin Orthop 1995;310:72–81
36 Stone KR, Steadman JR, Rodkey WG, et al. Regeneration of meniscal cartilage with use of a collagen scaffold. Analysis of preliminary data. J Bone Joint Surg Am 1997;79:1770–1777
< div class='tao-gold-member'>









