Chapter 6 Imaging of Osseous Knee Trauma
Acute traumatic injury involving the knee is a relatively common occurrence that has the potential to result in significant morbidity. The anatomy and physiology of the knee joint, along with the external forces to which it is subject, may result in a broad spectrum of injury types.8 Osseous knee injury may be related to direct trauma, avulsion forces, or chronic microtrauma.4 Diagnostic imaging plays a crucial role in the accurate diagnosis of traumatic injury and is therefore a critical element in the proper management of patients with a suspected knee injury.
A variety of imaging modalities are available for evaluation of the posttraumatic knee. Conventional radiographs are utilized most frequently in the initial evaluation of acute knee injury and effectively demonstrate displaced fractures, although more subtle fractures may remain undetected.8 The utility of radiographs for the evaluation of soft tissues is limited. Computed tomography provides a more sensitive evaluation of the osseous structures and offers some improvement over radiographs in terms of evaluation of soft tissue injury. Magnetic resonance imaging provides superior evaluation of soft tissues and marrow edema, as well as of physeal injuries in children.4
Bone Contusions
Bone contusions occur commonly as a result of traumatic knee injury and may be related to direct trauma, compression forces, or avulsive injury. When bone contusions are present, the underlying pathologic lesion reflects trabecular microfracture. Contusions are not appreciable on radiographs or CT, but are easily identified on MR as patchy areas of low signal intensity on T1-weighted images, with corresponding bright signal intensity on T2-weighted images—the so-called bone marrow edema pattern (Fig. 6-1). Avulsive injuries tend to be associated with less marrow edema than injuries resulting from compressive forces. The pattern of marrow edema signal may allow one to discern the mechanism of injury and thereby predict expected patterns of associated soft tissue and ligamentous injury.35
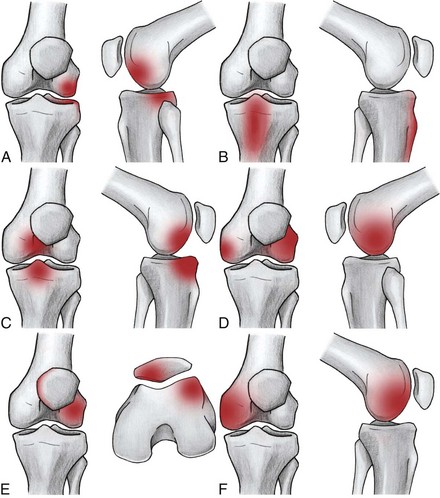
Six common patterns of bone contusions have been described (Fig. 6-2). Bone contusions involving the posterolateral tibial plateau and the midlateral femoral condyle are characteristic of pivot shift injuries, in which a valgus stress is applied to the knee with concurrent internal rotation of the femur while the foot is planted. The location of the femoral contusion varies depending on the degree of knee flexion at the time of injury, with a greater degree of flexion resulting in more posteriorly located edema. Commonly associated soft tissue injuries include those of the anterior cruciate ligament (ACL), posterior horn of the medial meniscus, and medial collateral ligament (MCL).19 Contusions involving the anterior tibia commonly occur secondary to direct trauma to the anterior tibia. Injury to the posterior cruciate ligament (PCL) and the posterior capsule may be seen in association with this edema pattern. Kissing contusions of the anterior proximal tibia and anterior distal femur result from hyperextension injuries. The cruciate ligaments, menisci, posterior capsule, and neurovascular structures may also be injured in the setting of this type of trauma. Clipping injury refers to a valgus stress applied to the lateral aspect of the knee with the joint in slight flexion. This type of injury typically results in edema of the lateral femoral condyle, with a smaller area of edema at the medial femoral condyle (Fig. 6-3). The MCL is commonly injured, and in the setting of more severe trauma, the ACL and medial meniscus may be injured as well. Lateral patellar dislocation may result in contusions involving the medial patellar articular surface and the anterolateral femoral condyle. Injury of the medial retinaculum, medial patellofemoral ligament, and medial patellotibial ligament may be associated with this injury mechanism.12,35 Injury to the posterolateral complex or corner of the knee is commonly associated with a characteristic pattern of marrow edema involving the weight-bearing surface of the anterior medial femoral condyle, typically due to hyperextension and varus forces. Associated soft tissue injuries of the posterolateral corner structures may include disruption of the fibular collateral ligament, popliteus muscle and tendon, and lateral and posterolateral joint capsular supports. Injuries to the PCL and ACL are also commonly observed in the setting of posterolateral corner injury.43
Bone contusions may be detected on imaging within an hour of injury and may persist well beyond the initial acute traumatic event, with a median healing time of approximately 42 weeks reported in one series.5,6 The time to resolution appears to be related to the presence of osteoarthritis, the age of the patient, and the type of bone bruise.6
Dislocations
Lateral Patellar Dislocation
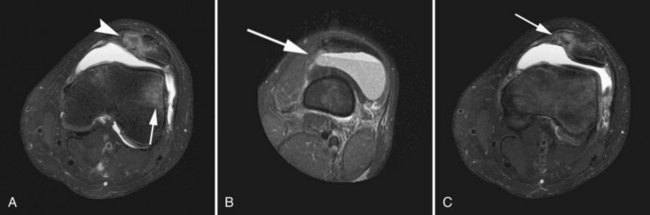
Traumatic lateral patellar dislocation is a common injury among young, athletic individuals and is generally transient in nature.35 Dislocation typically occurs in the setting of internal rotation of the femur on a fixed, externally rotated tibia. Lateral dislocation may also occur, less commonly, as the result of a direct blow to the medial aspect of the knee. Patellar dislocation tends to occur in a lateral direction because of the normal valgus alignment of the knee, as well as the relative weakness of the medial patellar retinaculum and vastus medialis as compared with the lateral stabilizers of the patella.12,35 MRI provides an ideal evaluation of transient lateral patellar dislocation, as the dislocation itself is typically brief, and many of the resultant injuries are not evident on radiographs owing to involvement of the soft tissues or occult osseous injury. Impaction of the medial patella against the lateral femoral condyle during relocation results in a characteristic pattern of bone contusions in these locations and often leads to an osteochondral injury of the medial patellar articular surface caused by a shearing force.35 Injury to the medial patellar retinaculum is a common finding, typically at the medial patellofemoral ligament. The relocated patella may demonstrate residual lateral tilt or subluxation. A hemarthrosis is also typically observed (Fig. 6-4).12,35
Femorotibial Knee Dislocation
Femorotibial knee dislocation is a rare injury that occurs secondary to high-energy trauma such as motor vehicle collisions, serious falls, and high-energy athletic injuries (Fig. 6-5). Patients with elevated body mass index also appear to be at higher risk for femorotibial knee dislocation, and seem to be more prone to suffer this type of dislocation in the setting of lower-energy trauma as compared with normal weight individuals.30
Knee dislocations may be classified according to the direction of tibial dislocation relative to the femur or, alternately, may be classified according to the observed pattern of ligamentous disruption.32 Utilizing a directional system, dislocations may be categorized as anterior, posterior, medial, lateral, or rotatory.32 Anterior dislocation is caused by hyperextension, typically of at least 30 degrees. Posterior dislocation is associated with a direct blow to the anterior tibia, such as a dashboard-type injury or fall on a flexed knee. Medial, lateral, and rotatory dislocations require components of varus, valgus, or rotatory stresses, respectively. Spontaneous reduction following dislocation may limit the utility of a directional classification system, as the original direction of the dislocation may no longer be discernible following spontaneous relocation. A system of classification of dislocations based on the pattern and extent of associated ligamentous injury has been developed and can provide useful insight into the mechanism and severity of injury.16,32
Soft tissue injuries associated with femorotibial knee dislocations are characteristically severe and commonly include extensive ligament, tendon, and neurovascular derangements.26,32 The likelihood of a particular structure being injured during femorotibial dislocation depends on the direction and severity of the initial traumatic force. The ACL is nearly universally injured in the setting of femorotibial dislocation, and injury to both cruciate ligaments is common. Injury to the collateral ligaments, menisci, and musculotendinous attachments is also commonly observed. The popliteal artery and the common peroneal nerve are the most commonly injured neurovascular structures, each being injured in an average of approximately 20% of cases. Careful clinical assessment is critical, as angiographic evaluation may be warranted to exclude popliteal artery injury.38
Fractures
A wide variety of radiologic descriptors may be utilized in the characterization of fractures. In terms of configuration, fractures may be described as complete, partial, impacted, physeal, avulsion, or osteochondral. A complete fracture involves both cortices and may be simple or comminuted. Directionally, fractures may be described as transverse, oblique, spiral, or vertical. Fracture alignment is described according to the displacement or angulation of the major distal fracture fragment relative to the proximal fragment. Displaced fractures are easily identified on radiographs as osseous disruption with displacement of fragment(s). A fracture of the knee involving the articular surface results in escape of blood and marrow fat into the joint space, creating a layering lipohemarthrosis, typically best appreciated on a cross-table or standing lateral view (Fig. 6-6).4 Subtle fractures may not be evident on conventional radiographs, and further evaluation with a more sensitive cross-sectional imaging technique is warranted in the setting of suspected occult injury. MRI provides not only more sensitive evaluation for suspected occult fracture, but also superior detection of associated soft tissue injuries.4,8
Distal Femoral Fractures
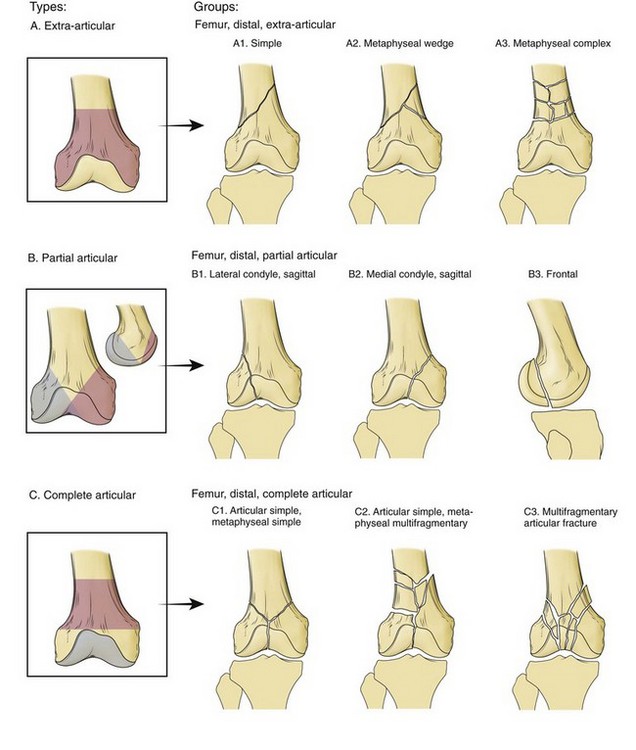
Distal femoral fractures occur less commonly than fractures of the proximal femur and account for approximately 6% of all femoral fractures.11 Fractures of the distal femur typically involve metaphyseal and condylar components (Fig. 6-7).11,31 A variety of systems exist for the classification of distal femoral fractures.11 One commonly utilized system developed by the Orthopaedic Trauma Association classifies fractures based on degree of articular involvement and comminution (Fig. 6-8).28 Initial radiographic evaluation for suspected distal femoral fracture should include dedicated images of the knee, as well as orthogonal views of the entire length of the femur, to exclude additional fractures.11 A dedicated CT may be obtained in cases of suspected intra-articular extension. Coronally oriented intra-articular condylar fractures (Hoffa fractures) are considered a marker of high-energy blunt trauma, and their recognition preoperatively is important in subsequent surgical planning. These fractures are commonly radiographically occult, emphasizing the importance of obtaining a preoperative CT in patients whose clinical presentation, mechanism, and associated injuries may suggest the possibility of this type of fracture.1
Tibial Plateau Fractures
Tibial plateau fractures are visualized on radiographs as cortical disruption and/or depression at the tibial articular surface, commonly with an associated lipohemarthrosis (Figs. 6-9 and 6-10).4 In some cases, lipohemarthrosis may be the only evidence of fracture on the radiographs, and in other cases, the fracture may be completely radiographically occult. Subtle fractures are best depicted on oblique radiographs of the knee, and visualization of a hemarthrosis is best accomplished with a cross-table lateral radiograph. Even in the case of easily identified displaced fractures, further imaging with a cross-sectional modality is generally warranted to define the extent of the osseous injury and assess for associated soft tissue injuries. CT is an excellent modality for evaluation of the osseous structures and provides visualization of fracture configuration, fragment positions, and degree of depression or separation of fragments. MRI is superior for the detection of occult fractures, as well as for evaluation of associated soft tissue injuries.22,25
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree