Fig. 3.1
Normal MRI appearance of menisci. (a) Coronal fat-saturated proton density-weighted sequence showing the normal, hypointense, and rectangular appearance of the posterior horns of the medial (arrow) and lateral meniscus (dashed arrow) in the coronal plane. (b) Sagittal fat-saturated proton density-weighted sequence showing the normal, hypointense, triangular appearance of the anterior (arrow) and posterior horn (dashed arrow) of the medial meniscus
Abnormal Meniscal Signals
A grading system exists for meniscal signal abnormalities. Higher grades are associated with more meniscal body involvement [14].
Grade 1 meniscal signals are focally increased signals that are globular in appearance and contained within the substance of the meniscus without coming into contact with the articular surface of the meniscus. These signals can be representative of mucinous and myxoid changes within the meniscus as a consequence of aging or areas of increased vascularity in children.
Grade 2 meniscal signals are linear regions of increased signal intensity that also do not extend to the articular surface of the meniscus. These signals are believed to be associated with meniscal degeneration, representing disruption of the normal collagen orientation.
Grade 3 meniscal signals are globular, linear, or complex areas of increased signal that extend to at least one articular surface. In the setting of grade 3 signal visualization on MRI, tears are identifiable arthroscopically in greater than 90 % of cases [16, 17]. Additionally, grade 3 signals can serve to heighten the index of suspicion for a closed meniscal tear and assist in the surgeon’s ability to identify these lesions via arthroscopic probing.
Classification of Meniscal Tears
The two primary criteria for the diagnosis of meniscal tears are intrameniscal signal that contacts the superior and/or inferior articular surface and/or abnormal meniscal morphology [8].
A commonly used classification of meniscal tears includes the following types: longitudinal, radial, displaced flap, bucket-handle, and complex.
Longitudinal tears, the most frequent type, are classified as horizontal (dividing the meniscus into an upper and lower segment), or vertical (dividing the meniscus into an inner and outer segment).
Longitudinal horizontal tears, also known as cleavage tears, are oriented parallel to or at a slight angle relative to the joint surface and perpendicular to the meniscocapsular junction (Fig. 3.2). Longitudinal horizontal tears are often associated with mucoid degeneration, and the associated signals may be difficult to distinguish on MRI (Fig. 3.3).
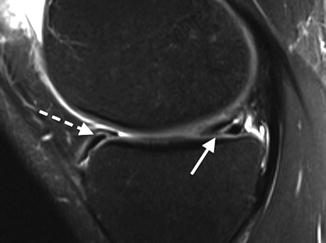
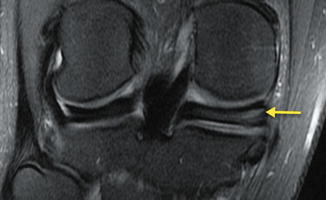
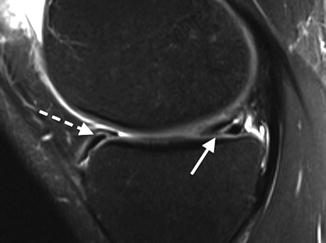
Fig. 3.2
Posterior horn horizontal tear. Sagittal fat-saturated T2-weighted image in a 39-year-old male shows linear internal meniscal signal contacting inferior medial meniscal surface (arrow). Note normal transverse (intermeniscal) ligament (dashed arrow) associated with the normal anterior horn, not to be confused with a meniscal tear
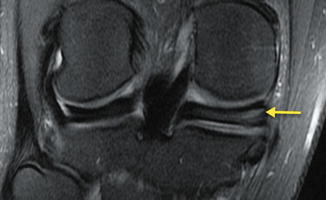
Fig. 3.3
Mucoid changes versus longitudinal horizontal tear. Coronal fat-saturated proton density-weighted image in a 41-year-old male shows abnormal horizontal signal (arrow) in the posterior horn of the medial meniscus, which may represent myxoid degenerative changes and/or a longitudinal horizontal meniscal tear
Longitudinal vertical tears are oriented perpendicular to the joint surface (Fig. 3.4). The etiology of these tears is commonly acute injury.
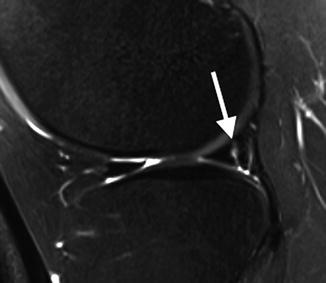
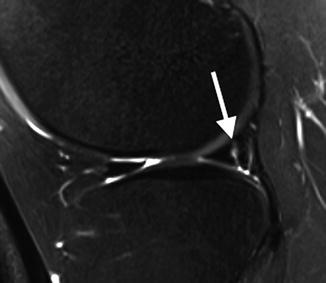
Fig. 3.4
Peripheral longitudinal vertical tear of posterior horn. Sagittal fat-saturated proton density image in a 27-year-old male shows a peripheral vertical signal within the posterior horn of the lateral meniscus (arrow) representing a tear
When the portion of the meniscus central to a longitudinal tear becomes displaced or “flips” into the intercondylar notch, this is referred to as a “bucket-handle” tear [10] (Fig. 3.5).
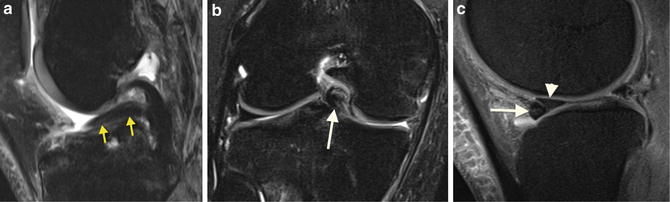
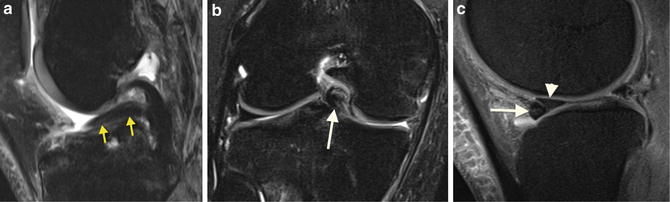
Fig. 3.5
Bucket-handle tears. Bucket-handle tear of the medial meniscus in a 25-year-old male with a large central meniscal fragment, seen on sagittal fat-saturated T2-weighted image (a) (“double PCL sign,” arrows) and on coronal fat-saturated proton density image (b) (arrow). (c) Bucket-handle tear of lateral meniscus in a 20-year-old male seen on sagittal fat-saturated proton density image as a fragment flipped interiorly (arrowhead), abutting the anterior horn (arrow) (“flipped meniscus sign”)
Radial tears extend from the central portion of the meniscus radially outward toward the periphery and may be partial or full thickness (Fig. 3.6). These tears are oriented perpendicular to the longitudinal collagen bundles of the meniscus [20]. Such tears sometimes extend anterolaterally or posterolaterally and are then referred to as parrot-beak or flap tears. Radial and flap tears account for approximately 5–10 % of meniscal tears.
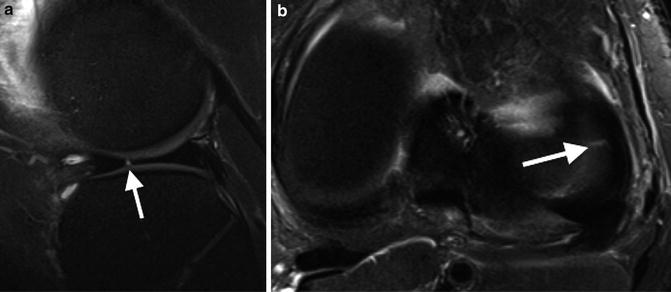
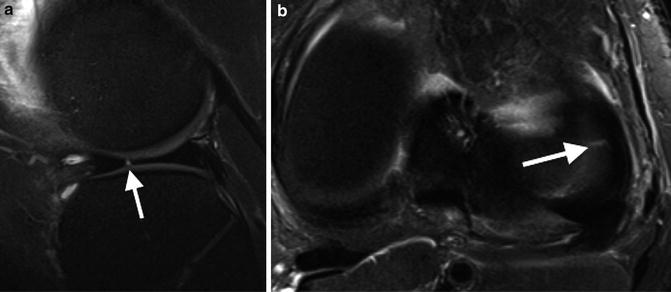
Fig. 3.6
Radial tear at junction of body and anterior horn. Sagittal fat-saturated T2-weighted image (a) and axial fat-saturated proton density image (b) in a 20-year-old male shows a fine linear fluid cleft (arrows), typical for a partial radial tear
A meniscal fragment may become displaced away from the site of tear, referred to as a displaced flap tear. Patients may present with locking in addition to knee pain. Like a radial tear, a displaced flap tear is manifested by a truncated or shortened appearance, but with a meniscal fragment that is typically flipped peripherally (Fig. 3.7).
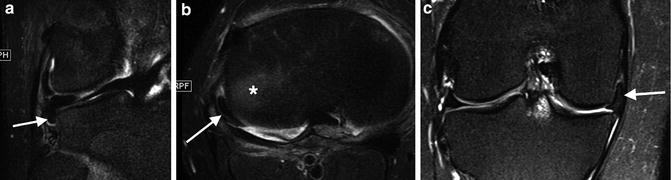
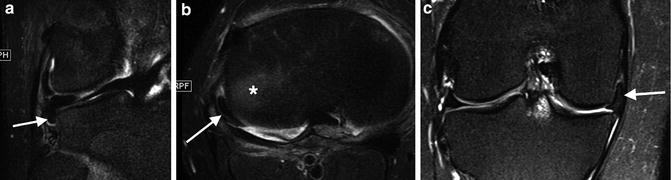
Fig. 3.7
Displaced flap tears lateral meniscal flap in popliteal hiatus in a 15-year-old male, on coronal fat-saturated T2-weighted image (a) and on axial fat-saturated proton density-weighted image (b) (arrows). Note reactive marrow edema of the adjacent tibia in B (asterisk). (c) Medial meniscal flap in a 53-year-old male seen on coronal fat-saturated proton density-weighted image, with blunting of the free inner margin of the body of the medial meniscus (arrow), with an associated inferior flap component in the medial gutter (between MCL and tibia) (dashed arrow)
Complex tears contain tears in multiple planes, typically with extensive morphological changes of the meniscus including loss of substance (Fig. 3.8).
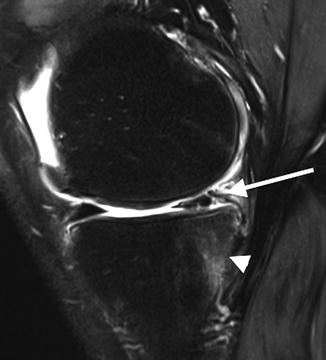
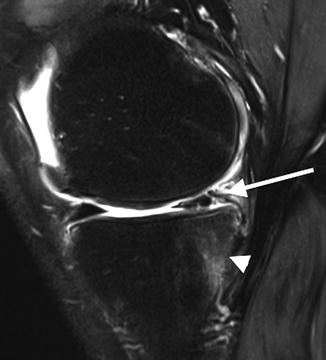
Fig. 3.8
Complex tear. Sagittal proton density image in a 66-year-old male shows a complex pattern of abnormal signal as well as morphological distortion of the posterior horn of the medial meniscus. Note reactive marrow edema of the adjacent tibia (arrowhead )
Another important type of meniscal tear is the root ligament tear or avulsion. Disruption of the root ligament of a meniscus disrupts the hoop tension and load distribution function of the meniscus [21]. The most common root tears occur in the posterior horn of the medial meniscus, typically representing a degenerative type of tear (Fig. 3.9a). Loss of the posterior anchor allows the meniscus to extrude medially and become less effective at shock dissipation.
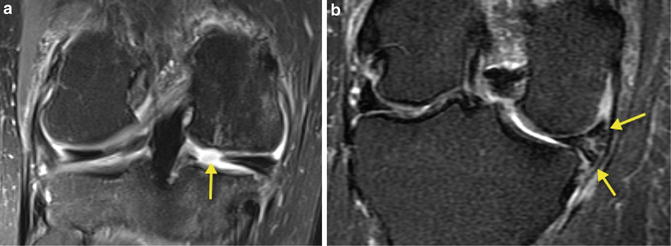
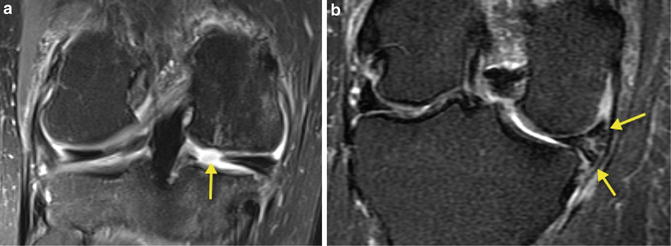
Fig. 3.9
Root ligament avulsions. (a) Coronal fat-saturated proton density-weighted image in a 50-year-old male shows a large tear of the root ligament of the posterior horn of the medial meniscus. (b) Peripheral extrusion of the body of the medial meniscus with a complex tear (arrows) in a 69-year-old female who also had a posterior root ligament tear (not shown)
A tear that occurs in the peripheral third of the meniscus may heal spontaneously or be successfully repaired, due to the vascular nature of this portion of the meniscus [18].
Associated and Secondary Signs of Meniscal Tears
Meniscal cysts are frequently associated with meniscal tears [22]. A meniscal (or intrameniscal) cyst is defined as a focus of high signal within a swollen meniscus. In the setting of increased pressure, fluid from an intrameniscal cyst can be squeezed or extravasated into the surrounding peripheral soft tissues, forming a parameniscal (also known as a perimeniscal) cyst [23]. Horizontal tears are also commonly associated with intra- or parameniscal cysts, as their orientation allows for synovial fluid extravasation through the tear but then acts as a one-way valve (Fig. 3.10) [19].
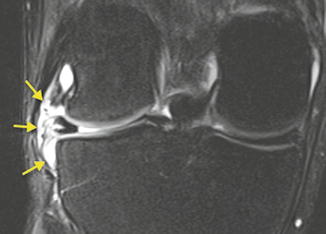
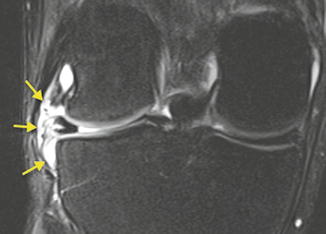
Fig. 3.10
Parameniscal cyst. Coronal fat-saturated proton density-weighted image in a 26-year-old male shows a lobulated parameniscal cyst (arrows) associated with a horizontal tear of the body of the lateral meniscus
Although laterally located cysts are more easily detectable clinically and potentially more symptomatic, the incidence of medial- and lateral-sided cysts is similar [24].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








