CHAPTER 25 Imaging findings in posterior instability
 Posterior instability of the shoulder is best imaged using a combination of computed tomography (CT) and magnetic resonance (MR) examinations.
Posterior instability of the shoulder is best imaged using a combination of computed tomography (CT) and magnetic resonance (MR) examinations. Posterior labral lesions, to include reverse Bankart lesions, Kim lesions, and POLPSA lesions, are best defined with MR arthrography.
Posterior labral lesions, to include reverse Bankart lesions, Kim lesions, and POLPSA lesions, are best defined with MR arthrography.Imaging modalities
Computed tomography (CT) of the shoulder can be performed with or without intra-articular contrast. CT is the best imaging modality for showing the bony anatomy of the glenohumeral joint. The glenoid contour is well evaluated with 3-dimensional CT imaging (Fig. 25-1), allowing estimation of bone loss caused by bony Bankart lesions. With intra-articular contrast, the labrocapsular structures can be evaluated, and the rotator cuff can be partially assessed.
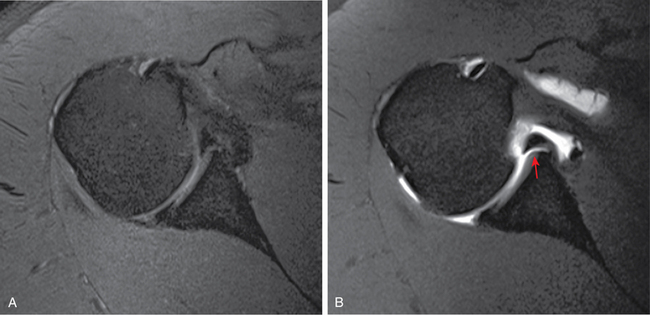
Magnetic resonance imaging (MRI) is the modality of choice for evaluation of the shoulder. Bone marrow abnormalities, labrocapsular tears, articular cartilage defects, and rotator cuff pathology can be identified using MRI. The reported detection of posterior labral tears on noncontrast MRI is mixed, ranging from a sensitivity of approximately 8%1 to 74%.2 The addition of intra-articular contrast with MRI enhances the ability to detect labral tears in general (Fig. 25-2). Chandnani et al compared CT arthrography, nonenhanced MRI, and MR arthrography (MRA) of the shoulder and found the labral tear detection rate to be 73%, 93%, and 96%, respectively.3 Recent improvements in MR technology have resulted in better spatial resolution and tissue contrast, leading some to conclude noncontrast MRI is as sensitive as MRA in detecting shoulder pathology. A recent study by Magee evaluating noncontrast examinations versus arthrograms using a 3 Tesla MR scanner demonstrated sensitivities for detecting anterior labral tears of 83% and 98%, respectively; posterior labral tears of 84% and 95%, respectively; and SLAP tears of 83% and 98%, respectively.4 Detection of articular surface partial tears of the supraspinatus also significantly improved with MRA. Magee found MRA altered the management in 27 out of the 150 patients in his study.4
Capsule
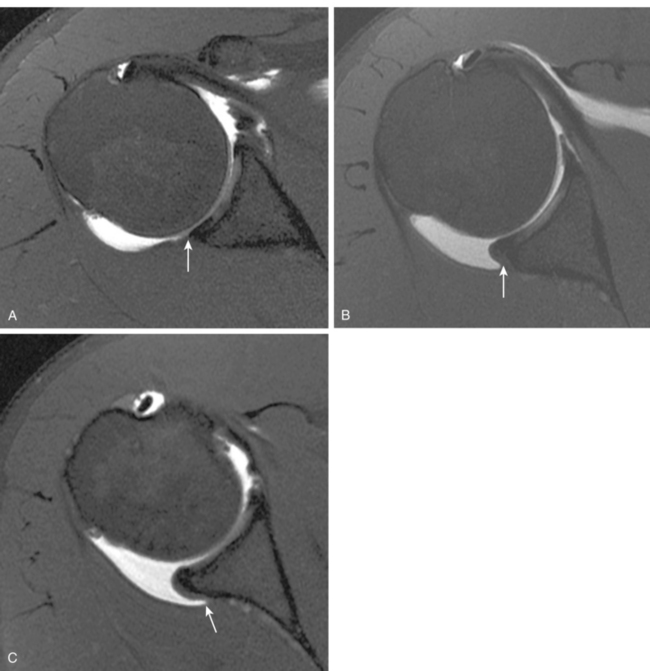
Insertion of the shoulder capsule onto the labrum or glenoid has been categorized previously according to a system by Mosley et al.5 A type 1 capsule inserts on the labrum, a type 2 capsule inserts on the junction of the labrum and glenoid, and a type 3 capsule inserts more medially on the glenoid (Fig. 25-3). The typical posterior capsule inserts on the labrum, either at the labral tip or the outer surface. This type of capsular insertion was present on all asymptomatic subjects in a study using MRI without contrast.6 Another study using MRA for evaluation of the capsule insertion showed more variability likely resulting from the joint distention. The results of this study showed 60% of posterior capsules had a type 1 insertion, 31% had a type 2 insertion, and 9% showed a type 3 insertion.7
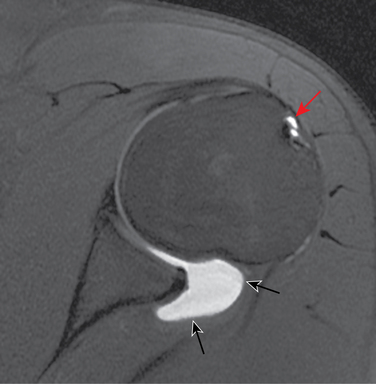
A lax posterior capsule is one of the potential causes of posterior shoulder instability. Posterior capsular laxity can occur in the presence or absence of tears of the labrum or supporting ligaments. Assessing posterior capsule redundancy in the absence of other structural abnormality can be difficult because few objective criteria currently are available. Dewing et al found a significant correlation between the cross-sectional area of the posterior/inferior capsule on MRAs, and patients with posterior and multidirectional instability.8 Variables that could cause an apparent capacious posterior capsule on MRA include overdistention of the capsule with contrast and external rotation positioning of the humerus during the examination9 (Fig. 25-4).
Glenoid version
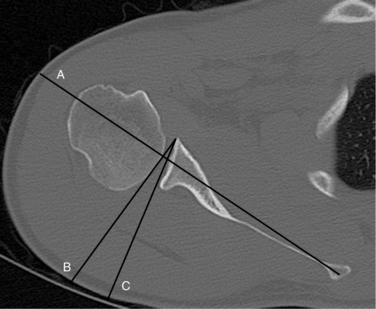
Glenoid retroversion, relative to the body of the scapula, can be a normal finding. However, a study by Weishaupt et al has shown a significant difference in the degree of retroversion between stable and unstable shoulders.10 Glenoid version is best evaluated using an axial CT image that includes the scapula body and is obtained at the mid-glenoid level (Fig. 25-5). A wide field of view axial MRI also can be used. Labral version also can be evaluated on axial MRIs, as well as axial CT arthrogram images.
Glenoid hypoplasia
Glenoid hypoplasia, posterior glenoid rim deficiency, and glenoid dysplasia may represent varying degrees of developmental bone loss along the posterior glenoid. Localized glenoid hypoplasia has been described as a sharp falling away, or more commonly, a pronounced rounding off of the posterior/inferior glenoid11 (Fig. 25-6). It has been identified in 18% of shoulder CT scans and MR studies.10 This study also associated posterior glenoid hypoplasia with shoulder instability. Another investigation determined the length of the posterior glenoid rim deficiency (1.2 cm), not the presence alone of glenoid hypoplasia, was the determining factor in distinguishing stable from unstable shoulders.9 Harper et al found a 14% incidence of moderate to severe glenoid dysplasia in a review of MRAs along with a high (64%) incidence of posterior labral tears in patients with dysplastic glenoids.12
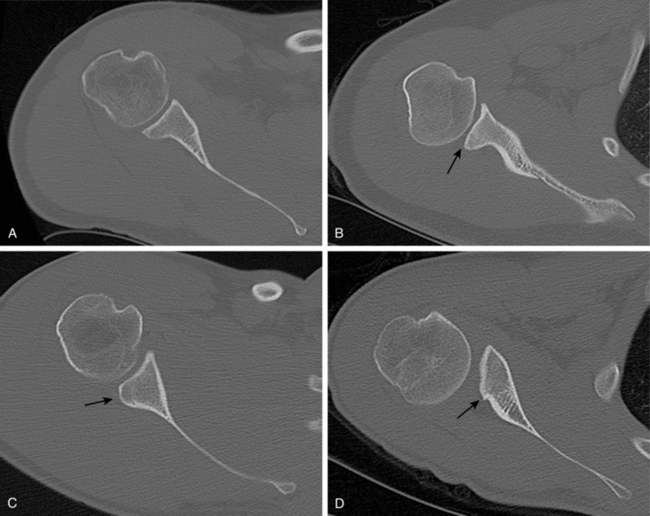
FIGURE 25-6 Axial CT images of four patients showing different configurations of the posterior glenoid. A, Normal glenoid shape with a pointed posterior lip. B, Mild posterior glenoid deficiency with a rounded contour to the posterior glenoid rim (arrow), described as a “lazy J” form.10 C, A triangular shaped deficiency (“delta” form9) of the posterior glenoid (arrow). D, Severe dysplasia of the posterior glenoid (arrow).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree