Humeral Shaft Fractures: Intramedullary Nailing
James C. Krieg
INTRODUCTION
Humeral shaft fractures are relatively common injuries and are estimated to account for up to 3% of fractures seen in clinical practice. The majority of fractures occur as isolated injuries; however, a small but significant number occur as part of a more complex constellation of upper extremity trauma or occur in a multiply injured patient.
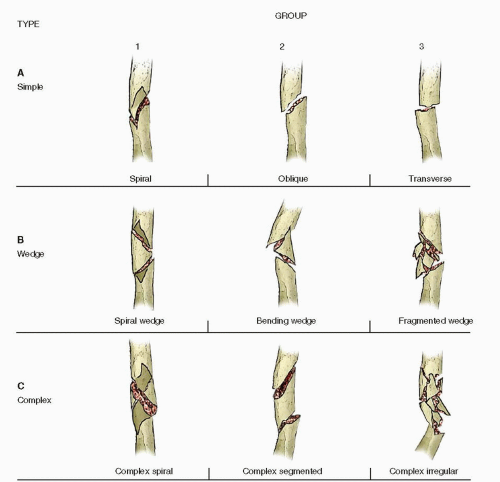
There is a classic bimodal pattern of injury, with older patients sustaining fractures following low- and intermediate-energy falls. On the other hand, injuries may be due to high-energy mechanisms, such as motor vehicle or motorcycle accidents, falls from heights, industrial injuries, gunshot wounds, etc. in younger patients. Depending on the mechanism of injury, fractures range from fairly simple patterns, such as spiral or transverse, to complex ones, which can be segmental or comminuted. Fracture patterns commonly seen in the humeral shaft are illustrated in the OTA/AO classification (Fig. 7.1).
Historically, isolated lower-energy humeral shaft fractures have been treated nonoperatively, with excellent results. Numerous authors have shown union rates of 95% to 98% with this method of treatment (1,3). However, in patients with higher-energy or displaced fractures, nonoperative treatment is less successful, and most of these patients benefit from internal fixation.
INDICATIONS AND CONTRAINDICATIONS FOR SURGERY
The goals of treatment following a humeral shaft fracture are union of the fracture, with minimal deformity that does not impair function or become a cosmetic issue. Treatment must allow early functional restoration of shoulder and elbow motion and recovery of muscle strength.
NONOPERATIVE TREATMENT
Nonoperative management is indicated for most closed, isolated, lower-energy humeral shaft fractures. The functional fracture brace method of Sarmiento remains the treatment method of choice for closed management. The patient is initially placed in a plaster coaptation splint until the acute swelling and pain have diminished. Most patients can be safely placed into a Sarmiento functional fracture brace a week following injury. Today, these braces are prefabricated, come in numerous sizes, and are easily adaptable to individual patients. The brace consists of polyethylene anterior and posterior shells. The margin of one shell fits inside the other. The halves are secured with velcro straps, allowing for continuous adjustment. Patients are encouraged to wear it snugly, adjusting daily (1).
Slings are discontinued after a few weeks to minimize shoulder or elbow stiffness. Patients are instructed in shoulder pendulum exercises and active and passive range of elbow motion. The brace is worn for 8 to 12 weeks, until healing is seen radiographically and arm motion is pain free. Success rates with this method of treatment are very high, with union rates >95% reported (1).
SURGICAL TREATMENT
There is a large group of patients in whom closed, nonoperative functional humeral bracing is not indicated. In these patients, surgery is required to restore limb alignment, provide access to the soft tissues, mobilize the extremity, or permit weight bearing through the extremity when lower extremity function is impaired.
There are several consistent indications for internal fixation of humeral shaft fractures using either plate osteosynthesis or intramedullary nailing. These include pathologic or impending pathologic fractures in order to relieve pain, improve stability, and facilitate cancer chemotherapy or radiation. Open fractures of the humerus typically benefit from early fracture stabilization to improve the treatment of the open wounds, thereby reducing the risk of infection. Similarly, humeral fractures associated with arterial injuries are best treated with early fixation to protect the brachial vessel repair. Another strong indication for surgery is the patient with ipsilateral fractures of the humerus and forearm. Stabilization of both fracture sites allows for early range of elbow motion. In patients with bilateral humerus fractures, at least one, and often both, should be fixed surgically to
decrease morbidity and facilitate activities of daily living. Lastly, in patients with an ipsilateral brachial plexus injury, surgery is typically indicated to reduce the risk of nonunion and facilitate early therapy.
decrease morbidity and facilitate activities of daily living. Lastly, in patients with an ipsilateral brachial plexus injury, surgery is typically indicated to reduce the risk of nonunion and facilitate early therapy.
Relative indications for operative management of humeral shaft fractures include displaced segmental fractures. These fractures are difficult to control in a fracture brace, increasing the relative risk of nonunion or malunion (2). In polytraumatized patients, internal fixation of a humeral shaft fracture may improve pain control, allow activities of daily living, and facilitate patient mobilization.
Operative treatment is also indicated in patients in whom an acceptable reduction cannot be obtained or maintained in a fracture brace. Surgery may be indicated in a patient with closed humeral fracture and softtissue injuries or abrasions that preclude brace application. Other patients do not tolerate bracing due to persistent pain or fracture instability due to their body habitus. Social considerations, such as job impairment, family needs, self-care, etc., may lead some patients to request operative treatment, which should be individualized.
In the critically ill or multiply injured patient, most closed fractures of the humerus are best treated initially with a coaptation splint. Once the patient’s overall condition has improved, internal fixation, when indicated, can be performed.
Implants: Plate Versus Nail
Several prospective randomized trials have shown comparable outcomes in patients with humeral shaft fractures treated with a plate or nail. Nevertheless, plate osteosynthesis remains the standard in surgical treatment of the majority of operative fractures of the humeral shaft in North America. Advantages of plating include anatomic reduction and compression fixation of noncomminuted fracture patterns. In addition, open surgery allows for exposure and protection of the radial nerve. In comminuted fracture patterns, bridge plating with restoration of length, alignment, and rotation is usually possible. With the advent of periarticular, anatomic specific plates, fixation can be performed for fractures that extend proximally or distally into the epimetaphyseal regions. Nevertheless, there are a number of disadvantages with plating, generally related to the large surgical exposure through the zone of injury. This carries with it the risk of fragment devascularization, iatrogenic nerve injury, and infection. In addition, it often leaves a long unsightly scar along the length of the arm.
Intramedullary nailing of the humerus, while used less frequently than plate osteosynthesis, has several mechanical and biologic advantages. Mechanically, intramedullary nails are strong implants, which can effectively share load. They are inserted using “minimally invasive” closed techniques. This eliminates direct exposure of the fracture site, reducing blood loss and decreasing the risk of infection. Intramedullary nails are ideally used to stabilize fractures in the middle three-fifths of the humerus. Many fractures that extend above the humeral diaphysis can be treated with either a plate or a nail. In the past decade, advances in nail design have improved fixation stability by the addition of multiplanar interlocking screws that often lock into the nail. This has expanded the range of fractures that are amenable to intramedullary nailing (Fig. 7.2).
Antegrade nailing with the patient in the supine position is used for the vast majority of patients. Retrograde nails are rarely used because of the risk of insertion portal comminution or fractures in the distal humerus. In addition, there is a need for the patient to be in the prone position. Numerous studies support the preferential
use of a reamed antegrade intramedullary nail, rather than a plate, in the following circumstances: (a) pathologic or impending pathologic fractures, (b) segmental fracture patterns, (c) severe osteoporosis, (d) long zones of comminution (Fig. 7.3), or (e) compromised soft tissues.
use of a reamed antegrade intramedullary nail, rather than a plate, in the following circumstances: (a) pathologic or impending pathologic fractures, (b) segmental fracture patterns, (c) severe osteoporosis, (d) long zones of comminution (Fig. 7.3), or (e) compromised soft tissues.
 FIGURE 7.2 A fixed angle, spiral blade interlock can help with proximal interlock stability. The blade is locked to the nail, reducing risk of loosening. |
It is important to emphasize that closed humeral nailing is contraindicated when the status of the radial nerve cannot be determined preoperatively. This occasionally occurs in patients with head injuries, altered consciousness from drugs or alcohol, mechanical ventilation, or polytrauma. In these circumstances, either open nailing with visualization of the nerve or plate fixation is safer. In patients with an open fracture as well as a radial nerve palsy, it is recommended that the nerve be explored. In these patients, plating seems preferable to nailing, since the majority of the exposure has been done at the time of nerve exploration. Intramedullary nailing is inferior to plating in treating humeral nonunion, and should not be used (11). The main disadvantages of antegrade humeral nailing are postoperative shoulder pain and higher incidence of hardware removal. This may be a significant consideration in patients whose work or avocations include significant overhead activity.
PREOPERATIVE PLANNING
There are a number of fracture-related, as well as patient-related, issues that must be analyzed when developing a treatment plan for a patient with a humeral shaft fracture. Fracture-related issues, such as the location of the fracture, the geometry or morphology of the fracture, associated soft-tissue condition, and the magnitude of displacement must be considered. In addition, patient-related issues such as medical comorbidities, body habitus, functional demands, the bone quality, as well as concomitant injuries, either in the same limb or elsewhere in the body, affect the choice of treatment.
HISTORY AND PHYSICAL
The history should include not only the mechanism of injury, hand dominance, occupation, and recreational activities, but the health status of the patient as well. Medical comorbidities, such as cardiovascular disease, diabetes, or a history of cancer, may influence diagnosis or treatment. The patient’s social history may provide useful information about their ability to cooperate with a rehabilitation program.
The patient and the injured limb must be carefully and systematically examined. Most patients have localized swelling, pain with palpation, or movement of the arm, and decreased range of motion of their shoulder and elbow. The skin must be examined to rule out an open fracture, which may be subtle. The brachial, radial, and ulnar pulses should be symmetrical with the opposite limb. Diminished or absent pulses or a cool hand after reduction require a vascular workup. The neurologic exam should include specific testing of the motor and sensory function of the radial, ulnar, and median nerves. Approximately 10% of patients with displaced humeral shaft fractures present with a radial nerve injury. Careful evaluation and documentation of the neurovascular status have both medical and legal significance. The vast majority of patients with a closed humeral fracture who present with a radial nerve palsy have a neuropraxia. These have an excellent prognosis, and the vast majority recover spontaneously. The indication for surgery is based more on the fracture status rather than
the radial nerve lesion. The management of a patient with a humerus fracture whose radial nerve function is lost after reduction and splinting is controversial. Various studies support both observation and early surgery. On the other hand, there is wide consensus that a radial nerve injury that occurs in the presence of an open fracture should undergo nerve exploration at the time of irrigation and débridement of the open fracture.
the radial nerve lesion. The management of a patient with a humerus fracture whose radial nerve function is lost after reduction and splinting is controversial. Various studies support both observation and early surgery. On the other hand, there is wide consensus that a radial nerve injury that occurs in the presence of an open fracture should undergo nerve exploration at the time of irrigation and débridement of the open fracture.
Imaging Studies
In a patient with a suspected humeral shaft fracture, a full-length AP and lateral x-ray of the humerus should be obtained. If the fracture extends into the proximal or distal epimetaphyseal areas, dedicated shoulder and elbow radiographs should also be obtained. It is imperative to understand the proximal and distal extent of the fracture if an intramedullary nail is to be used. The nail can only be inserted to the lowest extent of the medullary canal, which ends several centimeters above the olecranon fossa in most individuals.
In the painful arm, it can be difficult to obtain an axillary lateral of the shoulder. This is obtained by placing the x-ray cassette at the base of the neck with the x-ray beam directed from distal to proximal, through the axilla. This requires only a small amount of abduction, combined with forward elevation, of the shoulder. Occasionally, a CT scan may be necessary to completely understand the fracture.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree