Fig. 7.1
(a) Proximal transverse shaft fracture with important shortening in a 15-year-old boy after bicycle collision. (b) Anterolateral plating. Postoperative AP and lateral views. (c) Control X-rays after 6 months. Free shoulder and elbow function
Fractures of the Middle Third
The patient is placed supine with the broken arm on a radiolucent side table. The larger area of the fracture must be visible under image intensification. The deltoidopectoral approach as described for fractures of the proximal third is extended distally. The skin incision is curved in its upper part and is straight as it runs more distally. Proximally, the humeral shaft is exposed between the deltoid muscles laterally and the biceps, coracobrachial, and pectoral muscles medially. Distally, the anterolateral cortex of the humeral shaft is reached by longitudinal splitting of the brachial muscle. Special attention must be paid to the course of the cutaneous brachii and radial nerves. The first runs ventral to the brachial muscle, the last perforates the septum coming from the dorsal and going to the anterior and lateral muscle compartments. After plate fixation and rinsing, a single Redon drain is placed, muscle bellies are connected with single stitches, and the subcutaneous tissue and skin are closed separately. The drain is removed the second day after surgery, and active motion is allowed as soon as possible.
Fractures of the Distal Third
The patient is placed in a prone position with the broken arm in 90° shoulder abduction on a radiolucent side table and with the lower arm hanging down. The larger fracture area must be visible under image intensification. The skin incision runs strictly dorsally, in line with the humeral diaphysis, starting distally at the tip of the olecranon and going up as far as needed. Depending of the precise localization of the fracture, alternative deep approaches can be chosen. In fractures, located far above the olecranon fossa, the dorsal cortex of the humerus is exposed through longitudinal splitting of the triceps muscle. In more distal fractures, medial and/or lateral mobilization of the triceps muscle is recommended (Fig. 7.2a–c). In fractures with a very distal extension, olecranon osteotomy can be considered. Most challenging is the exposure and mobilization of the radial nerve, which crosses the dorsal cortex of the humeral shaft at the transition of its middle to distal third. Many times, placement of a plate between the radial nerve and the bone surface is needed. During fracture exposure, reduction maneuvers and plate placement, damage of the nerve by traction must be avoided. After plate insertion and rinsing, the triceps muscle is closed by single stitches. Two drains are placed, one in the triceps muscle, another in the subcutis. Subcutaneous tissue and skin are closed separately. The drains are removed the second day after surgery, and active motion is allowed as soon as possible.
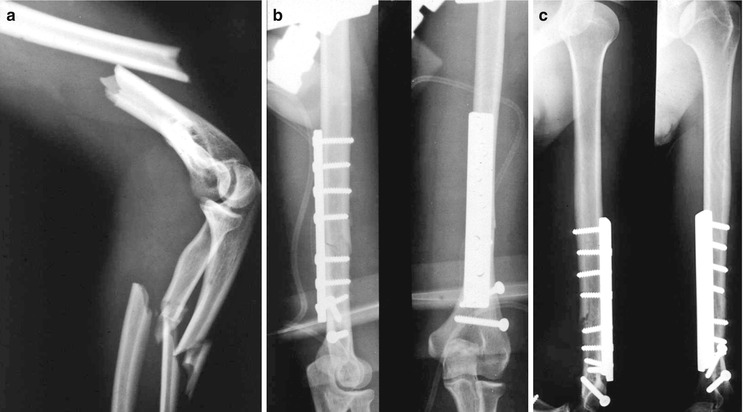
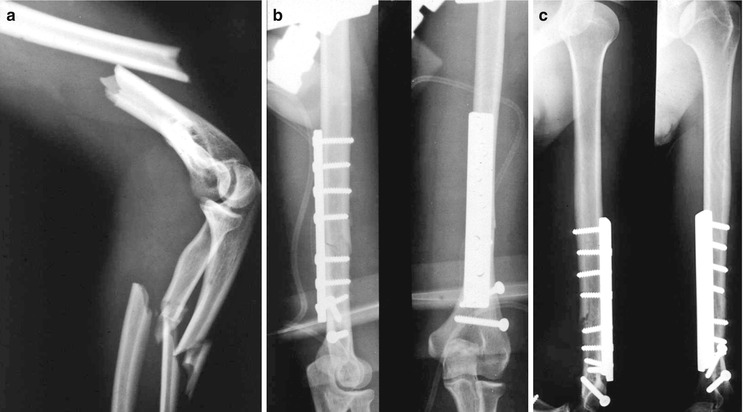
Fig. 7.2
(a) Floating elbow (distal humeral fracture and complete proximal lower arm fracture) of the left side in a 21-year-old male after car accident. Preoperative lateral view. (b) Dorsal plate osteosynthesis with broad DC plate. Additional lag screws for stabilization of intraarticular extension of the fracture. Postoperative AP and lateral views. (c) Control X-rays after 16 weeks. Free shoulder and elbow function
Complications
Problems that are specific for plate osteosynthesis are seen after humeral plating as well. Other complications are typical for the region in which the surgery is done. Delayed healing and pseudarthrosis is seen in between 5 and 10 % of cases. The main reason is deprivation of blood supply of fracture fragments resulting from careless manipulation. Other reasons are distraction of fracture fragments or bone defect in comminuted fracture types. Bone necrosis resulting from severe trauma is less frequent. Screw loosening or plate breakage leads to instability in the fracture site with axial deviation and pseudarthrosis. The origin can be found in severe osteoporosis or a weak bone-implant construct caused by a short plate and a small number of screws. Reosteosynthesis always will be needed, in most cases combined with cancellous bone grafting [9]. Deep infection is rare thanks to the excellent soft tissue coverage of the humeral shaft. It is the consequence of primary, severe traumatic soft tissue contamination or careless surgery. Secondary radial nerve palsy is a specific complication of plate osteosynthesis of fractures in the distal third of the shaft. The nerve must be exposed and mobilized to bring the plate on the dorsal cortex. Prognosis is good in cases of neuropraxia, but recovery of function can take several months [10]. Damage to the ulnar and median nerves or to the brachial artery is a rare complication. After surgery, a neurovascular examination of the operated extremity is compulsory to exclude or confirm any damage to these structures.
7.4.2.2 Intramedullary Nailing
This technique of stabilization has become the standard of treatment of femoral and tibial shaft fractures. Healing usually is uneventful, functional recovery quick, and the rate of complications low. Although used for more than 50 years, intramedullary nailing of humeral shaft fractures has only been widely accepted in the last decade. Older intramedullary implants bear the name of their inventors: Rush pins, Ender, Hackethal, Prévot nails. Their common characteristic is that they are flexible, thanks to their small diameter, and noninterlocked implants. They are introduced in an antegrade or retrograde way through small entry portals in the metaphyseal region. When the whole medullary canal is filled up, the construction has an adequate stability. As the rods are not fixed to the bone, a common problem is their migration proximally or distally with perforation of the shoulder or elbow joint, instability due to loosening, and shortening caused by telescoping of the fracture fragments. Flexible nails are widely in use for stabilization of humeral shaft fractures in children and adolescents.
The different nails in use for adults are thicker, more rigid, and can be interlocked statically or dynamically. Sometimes interfragmentary compression can be obtained. Nails are available as solid, cannulated, or hollow implants. Thicker nails are inserted after reaming; thinner nails can be introduced without previous reaming. The nails can be introduced in an antegrade or retrograde way. The indications for both approaches are slightly different as well as their difficulties and drawbacks [11, 12].
Antegrade Nailing
Midshaft and more distal fractures are the best indication for this approach [13, 14]. In proximal fractures, adequate stability after antegrade nailing is only guaranteed by multiple interlocking of the humeral head fragment. The patient is placed in a beach chair position with the upper extremity on an arm support. The broken humeral shaft together with the shoulder joint must be visible on image intensification. The skin incision runs anteriorly starting from the lateral edge of the acromion and has a length of only 2 cm. The muscle fibers of the deltoid muscles are split, the subacromial bursa opened, and the supraspinatus tendon identified. The tendon is split carefully in line with its fibers and separated to expose the cartilage of the humeral head. The entry portal for the nail is situated medial to the attachment of the supraspinatus tendon in the lateral cartilage area of the humeral head. The nail is inserted with careful rotator movements until its point reaches the fracture line. Under image intensification, the fracture is reduced and the distal fragment picked up with the tip of the nail. The nail is further introduced until it reaches its final position. If the nail is cannulated, its correct length can be read at the inserted guide wire; in case of solid nails, the length has to be measured preoperatively at the opposite extremity or at the reduced broken arm. At the insertion point, the nail must not protrude the articular surface of the humeral head. Double interlocking is recommended at each side of the fracture (Fig. 7.3a– e). Distraction must be avoided in the fracture site. Closure of the fracture gap or interfragmentary compression can be obtained by the use of a compression device in some nail types. Correct position of nail and screws is controlled under image intensification in two planes. The supraspinatus tendon is closed with separate stitches. A drain is placed between the supraspinatus tendon and the deltoid muscle. The deltoid muscle, subcutaneous tissue, and skin are closed consecutively. The operated extremity is placed in a collar and cuff bandage. The drain is removed on the second day and active motion of shoulder and elbow is allowed as soon as possible. As stiffness of the nail-bone construction is the lowest in the rotational plane, rotator movements of the arm are forbidden until bridging callus is visible on the follow-up X-ray controls.

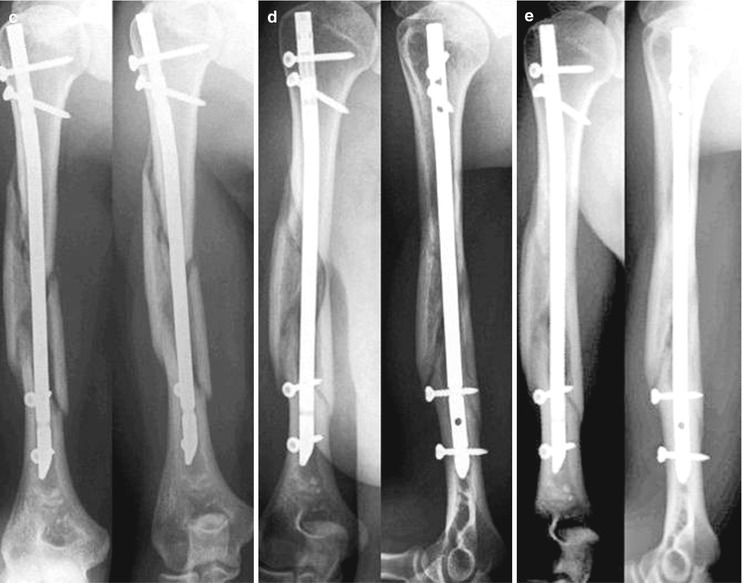

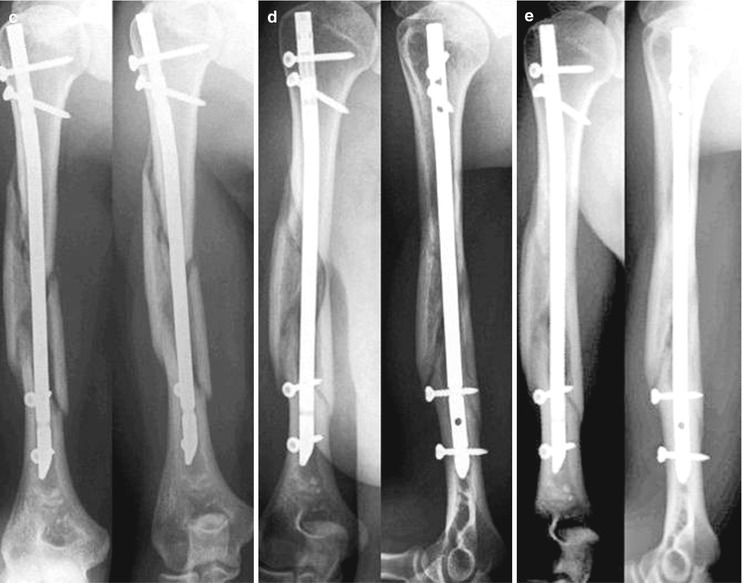
Fig. 7.3




(a) Closed multifragmental fracture of the right humerus after motorcycle accident in a 27-year-old male. AP and lateral views. (b) Antegrade nailing with double interlocking in the proximal and in the distal fragment. Postoperative AP and lateral views. (c) Control X-rays after 4 weeks. AP and lateral views. (d) Control X-rays after 16 weeks. AP and lateral views. (e) Control after 1 year, before metal removal. AP and lateral views. Free shoulder and elbow function
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








