Humeral Shaft Fractures
EPIDEMIOLOGY
It is a common injury, representing 3% to 5% of all fractures.
Incidence is 14.5 per 100,000 per year.
Two percent to 10% are open fractures.
Sixty percent involve middle third, 30% involve proximal third, and 10% involve distal third of the diaphysis.
Bimodal age distribution with a peak in the third decade is seen in men and peak in the seventh/eighth decade is seen in women.
ANATOMY
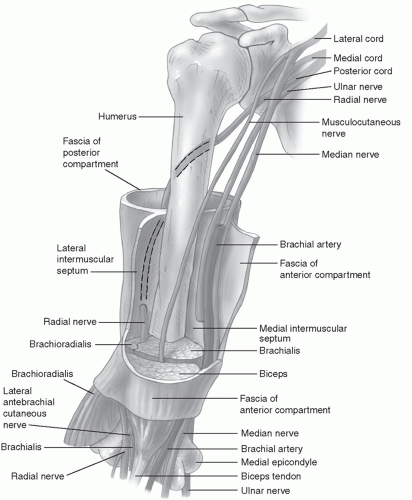
Humeral shaft extends from the pectoralis major insertion to the supracondylar ridge. Cross-sectional shape of humeral shaft changes from cylindric proximally to a narrower triangular shape distally.
Vascular supply to the humeral diaphysis arises from perforating branches of the brachial artery, with the main nutrient artery entering the medial humerus distal to the midshaft (Fig. 16.1).
Musculotendinous attachments of the humerus result in characteristic fracture displacements (Table 16.1).
Radial nerve can be identified 14 to 15 cm proximal to the lateral epicondyle or 20 to 21 cm proximal to the medial epicondyle.
MECHANISM OF INJURY
Direct (most common): Direct trauma to the arm from a blow or motor vehicle accident results in a transverse or comminuted fracture.
Indirect: A fall on an outstretched arm results in spiral or oblique fractures, especially in the elderly. Throwing injuries with extreme muscular contraction and arm wrestling have also been reported to cause humeral shaft fractures.
Fracture pattern depends on the type of force applied:
TABLE 16.1 Position of Fracture Fragments | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
CLINICAL EVALUATION
Patients with humeral shaft fractures typically present with pain, swelling, deformity, and shortening of the affected arm.
A careful neurovascular examination is essential, with particular attention to radial nerve function. In cases of extreme swelling, serial neurovascular examinations are indicated with possible measurement of compartment pressures.
Physical examination frequently reveals gross motion with crepitus on gentle manipulation.
Soft tissue abrasions and minor lacerations must be differentiated from open fractures.
Intra-articular extension of open fractures may be determined by intra-articular injection of saline distant from the wound site and noting extravasation of fluid from the wound.
RADIOGRAPHIC EVALUATION
Anteroposterior (AP) and lateral radiographs of the humerus should be obtained, including the shoulder and elbow joints. To obtain views at 90 degrees from each other, the patient, NOT the arm, should be rotated (transthoracic lateral), as manipulation of the injured extremity will typically result in distal fragment rotation only.
Traction radiographs may aid in fracture definition in cases of severely displaced or comminuted fractures.
Computed tomography, bone scans, and magnetic resonance imaging are rarely indicated except in cases in which pathologic fracture is suspected.
CLASSIFICATION
Descriptive
Open versus closed
Location: proximal third, middle third, distal third
Displacement: nondisplaced, displaced
Direction and character: transverse, oblique, spiral, segmental, comminuted
Intrinsic condition of bone: normal, osteopenic, pathologic
Articular extension
Orthopaedic Trauma Association Classification
See Fracture and Dislocation Compendium at http://ota.org/compendium/index.htm.
TREATMENT
Goals are fracture union with acceptable humeral alignment and patient return to preinjury level of function.
Both patient and fracture characteristics, including patient age and functional level, presence of associated injuries, soft tissue status, and fracture pattern, need to be considered when selecting an appropriate treatment option.