Fig. 6.1
Indication and surgical performance are major factors determining outcome after total knee replacement

Fig. 6.2
Clinical example of a female patient with little tibiofemoral OA but with patellofemoral OA undergoing a TKR. She complains about persistent heavy knee pain
On the other hand, a technically poorly performed TKR in a patient with the correct indication will also not lead to a pain-free and happy patient. Preoperatively, a number of factors have to be evaluated to optimise outcome after TKR.
An optimal outcome can be achieved when only the initial indication for surgery is correct. A poorly indicated TKR will rarely lead to good outcome after TKR. A well-performed TKR in a patient with only early OA has a higher chance of persistent pain than in a patient with severe OA. It is of utmost importance to exclude a hip or spine pathology, which could also result in severe knee pain.
6.2 Optimal Patient Selection: Patient-Related Factors Predicting Outcome After TKR
Optimal patient selection and unambiguous identification of the cause of the patient’s problems are decisive for achieving a satisfied patient after TKR.
It is a well-known fact that patients with a moderate or low degree of OA have worse outcomes undergoing TKR than patients withsevere OA [5]. This could be due to different pain adaptation and coping strategies between those groups. Hence, in our experience, it is recommended to postpone surgery in such patients. In the meantime, the patient can be treated with conservative treatment modalities such as pain therapy, injections into the knee or physiotherapy (Fig. 6.2). If there is failure to respond to conservative treatment for more than 6 months, TKR can be reconsidered.
The patient should be meticulously assessed for current pain, deformity, joint laxity, instability and preoperative range of motion. Here, in particular, flexion or extension deficits or hyperextension needs to be noted.
The patient needs to be informed about the expected range of motion after TKR. Here there is a paradox: patients with a full range of motion preoperatively will always lose some movement and patients with stiff knee and reduced range of motion will gain movement. This fact needs to be adequately explained to the patient. Some authors advise preoperative physiotherapy sessions to enhance the patient’s adaptability to the TKR rehabilitation protocol.
Optimal patient selection and unambiguous identification of the cause of the patient’s problems are decisive for achieving a satisfied patient after TKR.
Another subgroup of patients is the one suffering from crystal arthropathies or inflammatory arthritis such as gout. In particular, for gout or chondrocalcinosis, it is not rare that even after a well-performed TKR, joint effusion and pain will persist (Fig. 6.3). Therefore, it is advisable to consult a rheumatologist to adapt medical treatment even before undergoing TKR. The rheumatologist should be a vital part of the management team in such patients.


Fig. 6.3
Clinical example of persistent pain and effusion due to chondrocalcinosis after TKR. Anterior-posterior (AP) radiographs before TKR showing chondrocalcinosis
A subset of patients still undergoes TKR for extrinsic pathologies such as ipsilateral hip OA or degenerative spine disease [6]. Al Hadithy et al. reported that about one third of patients presenting with unexplained pain after TKR had undergone TKR for hip OA or degenerative spine disease [6]. Hence, we need to give more emphasis on ruling out such a problem before TKR. Due to specialisation as a knee surgeon, this problem might become more frequent in the future, as we might not put enough emphasis on the assessment of adjacent joints. We need to be aware of referred pain and be very cautious with patient selection. Thus, it is pertinent to perform hip or spine X-ray before TKR.
A high BMI is also an important cause for postoperative pain. A higher BMI does correlate with higher pain scores postoperatively [7]. However, it is unclear whether the higher pain scores are due to more comorbidities in these patients, are due to a psychological issue or are really due to the increased BMI.
Any previous surgery of the patient on the affected knee has to be documented and recognised. A previous surgery can alter postoperative pain and such patients should be identified before TKR. Plans should be made in advance for how to deal with such patients. Finally, one must consider the patient’s psychological well-being as a factor for outcome after TKR. Numerous studies have demonstrated a relationship between preoperative anxiety, depression and pain tolerance and persistent pain after TKR [8–10]. Such patients should be carefully counselled for surgery. In certain cases, it will also be necessary and helpful to get a psychologist’s or psychiatrist’s opinion before TKR. If the patient is averse to meeting with such a specialist, at least a clinical psychologist should be in the treating team. All patients undergoing TKR should be given a realistic picture of what to expect after TKR. Unrealistic patient expectations can lead to a dissatisfied patient. Thus, any postoperative pain will be noted as unsuccessful surgery in the patient’s mind. In the patient’s mind, surgery will be successful only if his or her expectations are closely met after TKR.
Patients suffering from crystal arthropathies or inflammatory arthritis such as gout or chondrocalcinosis are known to have persistent or recurrent joint effusion and pain even after a well-performed TKR. Therefore, it is advisable to consult a rheumatologist to adapt medical treatment even before undergoing TKR.
6.3 Key Points for Clinical Examination
A thorough and detailed clinical examination before TKR helps to establish the correct cause of a patient’s problems (see Chap. 25).
Special emphasis has to be put on the skin condition over the surgical site, preoperative knee range of motion, flexion contractures, angular deformities or relevant instability of the knee joint.
Assessment of gait might give additional information on the underlying knee pathology. Joint laxity/varus thrust and hyperextension are best identified while the patient is walking. In certain cases, patients should be referred to a gait analysis laboratory for documentation and analysis of gait.
The combination of deformities and instability adds to the complexity of TKR. Proper preoperative planning in such cases is required since these patients may require more constrained prostheses such as a condylar constraint (CCK) TKR.
In an unstable or hyperextended knee, minimal bony resection should be planned and a more constrained TKR should be made available. In cases with severe flexion deformity, posterior capsular release and adequate bony cuts are essential to correct the deformity.
Assessment of the knee should include foot progression angle and both malleoli rotation to decide the angle of rotation deformity. This makes us aware that in such a patient proper rotation of the femoral and tibial component is critical to a good outcome. Also, a preoperative CT scan can help in such cases. Hind foot abnormalities have been stressed lately, as the actual ground mechanical axis is affected by the deformities at ankle and subtalar joint level. If correction of deformity is possible at this level, the mechanical axis does not need to be altered. However, if these joints are fixed in varus or valgus deformity, it could result in an under- or overcorrection of the mechanical axis.
Integrity of the extensor mechanism (quadriceps and patellar tendon) [11] should be assessed preoperatively. An insufficiency of the extensor mechanism may be present in 1 % of cases and this could lead to poor postoperative outcome. Especially in cases with fused knees or with neurological disorders, an atrophy or hypotrophy of the adjacent knee muscles needs to be identified. A prolonged rehabilitation period is to be expected and physiotherapy protocols have to be adapted accordingly.
A complete neurological and vascular assessment of the lower limb should be performed preoperatively. In all cases, clinical examination of the adjacent knee and adjacent joints including ankle, hip and spine should be done.
6.4 Key Points of Radiological Evaluation (See Chaps. 28, 29, 30, 31 and 32)
1.
Radiography: Long leg weight-bearing radiographs
Standard weight-bearing long leg radiographs are the most important X-rays for the planning of TKR. Standing view of both legs allows assessment of the mechanical axis (a line drawn from the centre of the femoral head to the centre of the ankle joint). Also, the femoral and tibial anatomical axes can be defined here.
On these radiographs, the angle between the mechanical and anatomical axis of the femur can be used to plan the distal femoral cut as a reference for TKR surgery (Fig. 6.4). Mcgory et al. however found that it did not significantly aid in obtaining a neutral mechanical axis compared with performing a standard cut of 5° [12]. This may be due to increased femoral bowing, variation in neck shaft angle and possibly geographical variations.
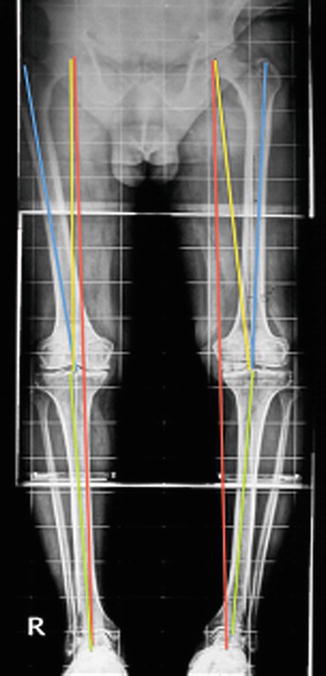
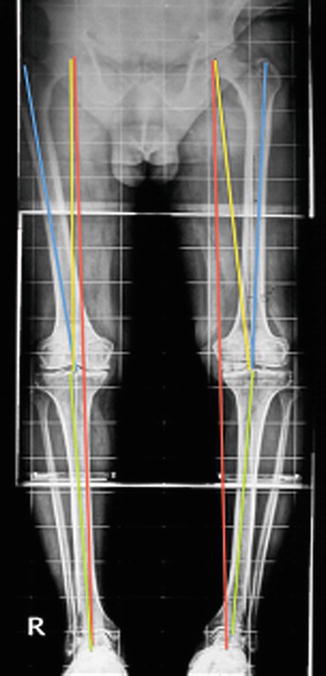
Fig. 6.4
Angle between the mechanical and anatomical axis can be used as a reference for TKR surgery
Preoperative planning to replicate the neutral mechanical axis should be individualised for every patient and cuts should be planned accordingly [13]. In cases with severe deformities, the use of a standard intramedullary guide may not be possible and could be misleading. Here, computer navigation may be helpful. Extra-articular deformities are better recognised in long leg radiographs and can be missed on standard knee X-rays.
2.
Weight-bearing AP, Rosenberg and patella skyline view—Standardised true weight-bearing radiographs (AP) are crucial for grading of OA. A Rosenberg view (40° flexion PA view) allows assessment of the intercondylar notch in cases of flexion deformity. A limitation of these radiographs is that joint deformity is underestimated and they do not account for extra-articular deformities.
3.




In cases with bone defects, proper assessment of the defect size and planning regarding augments should be done. This radiograph can also provide an idea regarding proximal tibia vara in cases of varus knee or post high tibial osteotomy (HTO). This will be an important deciding point while placing the tibia tray.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








