, Michel Serrault1 and M. Mullins1
(1)
Department of Trauma, Hôpital Raymond Poincaré, Garches, Paris, France
Abstract
In young and active patients, hip arthritis remains a challenge, whatever the improvements in materials, design, bone fixation and interfaces of total hip prosthesis (THR). Resurfacing provides a solution to at least some of these problems.
The anterior approach is the traditional approach for hip replacement in our department, as described and practised by Robert and Jean Judet since 1947, initially for the historical acrylic cephalic prosthesis and subsequently for all types of THR. It can be used as a truly minimally invasive approach as described by Siguier. This approach is now our standard approach for THR, allowing implantation without tendon or muscular section and taking advantage of the anteversion of both the neck and acetabulum.
This short prospective series involving just two types of implant does not allow any conclusion to be made about resurfacing concept: We have a favourable initial impression but as yet no answers regarding uncemented fixation, the prevention of bone trabecular modification, the incidence of metal ion release and so on.
On the other hand, the anterior approach performed on an efficient orthopaedic table seems to be recommendable. The only absolute contraindications are resurfacing combined with femoral osteotomy or cases where simultaneous metalwork removal is required.
So, for the marriage of resurfacing and a minimally invasive anterior approach, we have only great hopes for the implant but a complete and unrestricted faith in the approach!
Keywords
Hip resurfacingAnterior approachYoung patients, Robert and Jean Judet approachSiguier minimal invasive approachNo tendon or muscles sectionIntroduction
What Are the Reasons for an Interest in Hip Resurfacing?
In young and active patients, hip arthritis remains a challenge, whatever the improvements in materials, design, bone fixation and interfaces of total hip prosthesis (THR). Resurfacing provides a solution to at least some of these problems; femoral neck elasticity and mechanical properties are preserved and the large head prevents dislocation. Moreover, it leaves the diaphyseal canal entirely intact to allow a more efficient and simple conversion to conventional total hip arthroplasty in the case of failure. Improvement of metal-on-metal bearings (McMinn [1–4], Wagner, Amstutz, etc.) since 1991 led us to suggest resurfacing for younger patients.
What Are the Reasons for the Anterior Approach?
It is the traditional approach for hip replacement in our department, as described and practised by Robert and Jean Judet since 1947, initially for the historical acrylic cephalic prosthesis and subsequently for all types of THR. It is basically a Hueter approach [3] which can be enlarged distally or, more frequently, proximally, as described by Smith-Petersen. On the other hand, it can be used as a truly minimally invasive approach as described by Siguier [4]. This approach is now our standard approach for THR, allowing implantation without tendon or muscular section and taking advantage of the anteversion of both the neck and acetabulum.
Since 2002, we have combined the accepted wide possibilities of anterior approach with the potential advantages of hip resurfacing [2].
Specificities and Details of Anterior Approach for Hip Resurfacing
The key point is to have a perfect view and instrumental control of both the acetabulum and femur for correct positioning and implantation.
Anatomic Basis
The anterior approach reaches the hip where the joint is the most superficial. It passes between two territories of innervation: the femoral nerve medially (sartorius (Sa), rectus femoris (RF) and iliopsoas (IP)) and the superior gluteal nerve laterally (tensor fascia latae (TFL), gluteus minimus (Gmin) and gluteus medius (Gmed)).
Neither muscle nor tendon is cut, except occasionally a release of the reflected tendon of rectus femoris. The anterior circumflex artery is the only vascular obstacle and is ligated.
Patient Set-Up and Operative Field Preparation
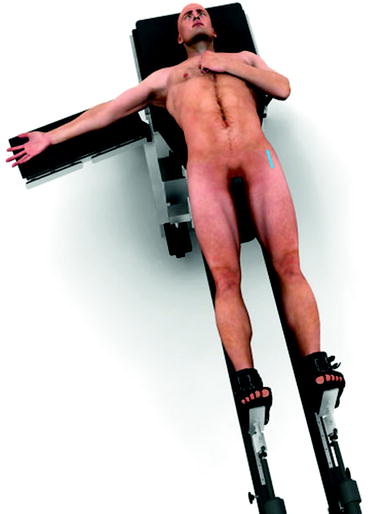
As always for the anterior approach, the patient lays supine on a fracture table which allows for any positioning of the lower limbs, particularly hyperextension, unlimited external rotation and adduction (Judet-Tasserit table, Collemier, France) (Fig. 10.1). Both antero-superior iliac spines and the pubis are accessible to palpation through the drapes, in order to confirm pelvic orientation. Likewise, palpation of the patella indicates the degree of external rotation. A rectangular 15 × 10 cm operative field is prepared, centred distally and laterally to the antero-superior iliac spine.