Hip Dysplasia in the Child and Adolescent
Darin Davidson and Young-Jo Kim
Key Points
• Developmental dysplasia of the hip represents a spectrum of severity of involvement of the hip.
• A high degree of clinical suspicion can allow for early diagnosis of acetabular dysplasia.
• Early treatment of acetabular dysplasia can be effective in preventing later sequelae.
Introduction
Developmental dysplasia of the hip (DDH) is an idiopathic condition that presents as a continuum of hip instability, which may affect children and adolescents. Newborn or young DDH presents as a spectrum from hip joint laxity to dislocation (Fig. 40-1), which may be reducible or irreducible. In older children and adolescents, DDH is associated with variable components of acetabular dysplasia, proximal femoral abnormality, and ligamentous laxity. Acetabular dysplasia is characterized by a globally shallow acetabulum with a steep acetabular roof. Proximal femoral abnormalities consist of varying degrees of coxa valga and anteversion. Varying degrees of subluxation of the femoral head from the acetabulum are present. Some degree of ligamentous laxity in the affected hip joint is universal before treatment, and generalized ligamentous laxity is common. In addition to the primary anatomic abnormalities associated with DDH, a variety of secondary deformities may occur after local growth disturbances following treatment.

Figure 40-1 An anteroposterior radiograph demonstrating left hip dislocation in a 16-month-old female.
Epidemiology
Prevalence
The prevalence of DDH has been difficult to ascertain because of the wide spectrum of the disorder. The overall prevalence of dislocation has been reported to be 1.4 per 1000 live births, the prevalence of clinical findings consistent with acetabular dysplasia has been 2.3 per 1000 live births, and the prevalence of ultrasound abnormalities has been 8 per 100 live births.1 In addition, wide variation in prevalence among various ethnic groups has been recognized, ranging from 0.1 per 1000 live births in a Hong Kong population2 to 188.5 per 1000 live births in a Native Canadian population.3 Further complicating these estimates are the cases of subtle acetabular dysplasia not presenting until adolescence or adulthood and, therefore, not included in prevalence studies of infant DDH.
Risk Factors
Risk factors associated with infant DDH have been well studied. This condition most likely is multifactorial in nature. Implicated predisposing factors include ligamentous laxity, prenatal positioning, postnatal positioning, and genetic factors. Additional implicated factors are first born, female sex, and a history of oligohydramnios.4–6 The left hip has been affected more commonly in unilateral cases, possibly owing to left hip adduction in the most common intrauterine position of the occiput anterior.5,6
Prenatal positioning has been associated with DDH. Early studies demonstrated that 16% of newborns with DDH were born in a breech position,7 and this risk increased to 20% in a frank breech position.8 According to Dunn,5,6 it is the intrauterine position, not necessarily the breech position during birth, that is responsible for elevated risk of DDH because the prevalence of DDH among those in a breech position born via cesarean section was not found to be decreased. Postnatal positioning of newborns has been demonstrated to increase the risk of DDH on the basis of increased prevalence among populations who use cradleboards.9,10 Klisic and associates11 reported a 65% decrease in DDH attributed to an intervention with positioning newborns in hip abduction, instead of adduction. Other postural abnormalities have been associated with DDH, with the underlying proposed mechanism of so-called packaging disorders. Torticollis has been thought to coexist with DDH in 15% to 20% of cases.12 Metatarsus adductus has been associated with DDH in 1.5% to 10% of cases.13,14 Contradicting these so-called packaging phenomena has been the lack of association between clubfoot and DDH.15,16
Pathophysiology
Normal hip development is a complex process, both during the embryonic phase and postnatally. Its details are beyond the scope of this chapter, and interested readers are directed to other sources.1,17 Hip dysplasia represents a spectrum of pathophysiologic and anatomic abnormalities that, although initially potentially reversible, tend to become more severe and less correctable over time.1,17 Bony deformity in infant DDH is believed to be due to lack of normal mechanical forces in and around the joint, plus the application of abnormal mechanical forces on the elements of a joint with varying degrees of instability and subluxation. In the newborn with DDH, the capsule is lax and the posterosuperior acetabular rim may be abnormal, allowing the femoral head to subluxate or dislocate. Over time, the rim can become thickened and develops into the so-called neolimbus as the result of pressure exerted by the femoral head.18 If a newborn unstable hip becomes and remains persistently dislocated, secondary obstacles to reduction usually develop, including a fibrofatty pulvinar, hypertrophic ligamentum teres, a thickened transverse acetabular ligament, an inverted or hourglass labrum and cartilaginous acetabulum, and an interposed iliopsoas tendon. Complete reduction of the hip can allow for acetabular remodeling with further growth, with earlier improved restoration of normal containment. If, however, the hip is persistently dislocated or subluxated, certain characteristic bony changes tend to develop and become permanent, including the characteristic flattening of the acetabular roof, thickening of the medial acetabular wall, and, in the case of frank dislocation, development of a false acetabulum.
Natural History
The natural history of the unstable hip in the newborn is difficult to ascertain, in part because of the difficulty involved in defining an unstable hip. Barlow19 initially suggested that 60% of subluxatable or dislocatable hips resolved by 1 week and 88% by 2 months. Coleman9 reported resolution of only 5 of 23 unstable hips, illustrating a wide-ranging understanding of the natural history.
The natural history of persistent acetabular dysplasia includes progressive premature degeneration of the hip joint with the onset of osteoarthritis due to abnormal concentrations of mechanical hip joint forces on a decreased contact area. Wiberg20 defined abnormal femoral coverage as a center edge angle less than 25 degrees, which would lead to eventual osteoarthritis. Cooperman and associates21 reported that all dysplastic hips with a center edge angle less than 20 degrees developed osteoarthritis by 22 years’ follow-up. However, the onset of osteoarthritis was difficult to predict unless the hip was subluxated. Subluxation clearly worsens the prognosis greatly, no matter what the degree of acetabular dysplasia. Murphy and colleagues22 reported a study of the contralateral hip among 286 patients who were treated with total hip arthroplasty for osteoarthritis due to acetabular dysplasia. They found that all hips with good function at 65 years of age were associated with a center edge angle greater than 16 degrees.
Clinical Findings/Physical Examination
Typical physical examination findings associated with DDH depend, to some extent, upon the age of the child and the degree of instability and deformity. In the newborn period, usually up to 2 to 3 months of age, Barlow and Ortolani tests are performed. The Barlow test is a gentle test of stability, performed by adducting each hip sequentially and applying a posteriorly directed force. This test assesses the ability to subluxate or dislocate the hip. The Ortolani test is a test that assesses reducibility. It attempts to reduce the dislocated hip, and for this reason it is best performed before the Barlow test. It is performed by abducting the flexed hip with an anteriorly directed force applied at the level of the greater trochanter. These signs usually are not detectable, even in an unstable hip, after the age of 2 to 3 months. Note that the absence of a Barlow or Ortolani sign is no guarantee that a hip is normal. An irreducible dislocated hip will show neither sign!!
In the child older than 2 or 3 months of age with an unstable or dislocated hip, the ipsilateral adductor muscles tend to shorten, and some limitation of abduction is often present. In the older than 3 month age group, often Barlow and Ortolani signs are absent, but the limitation of motion will remain. Asymmetrical range of motion is suggestive of an abnormality, but the possibility of bilateral involvement must always be considered.
The Galeazzi sign is elicited by noting limb length discrepancy while flexing both hips and knees to approximately 90 degrees and comparing the relative levels of the knees. It is present if shortening of one femur is apparent. It is important to be aware of the possibility of bilateral hip dislocations, in which case hip abduction can be decreased bilaterally but symmetrical and the Galeazzi sign negative. The Klisic test can be of use to delineate this situation and is performed by placement of the index finger on the anterior superior iliac spine and the middle finger on the greater trochanter. A line between these two points should intersect the umbilicus if the hip is reduced and will be inferior to this if dislocated.
In the older child with a complete hip dislocation or high-grade subluxation, physical findings may include a limb length discrepancy with the shorter leg being the affected side, a positive Galeazzi sign, increased lumbar lordosis, usually related to hip flexion contractures, and decreased range of hip abduction in the dislocated hip. The hip with a complete dislocation usually is hypermobile in childhood, especially in rotation.
By midchildhood, certain symptoms associated with hip dysplasia may occur and may be elicited by careful patient questioning. The earliest symptoms of hip dysplasia usual are reported as postactivity ache over the greater trochanter. Later symptoms often include activity-related groin pain as the overloaded acetabular rim and the labrum begin to fail. If the labrum tears, this could lead to mechanical symptoms of locking and catching, although this rarely occurs before the time of maturity. With the onset of osteoarthritis after maturity, the joint may have persistent aching pain as well as night pain.
Imaging
Ultrasound
Ultrasound is the best imaging modality for assessing hip anatomy and stability during the first 6 months of life. Owing to the large cartilaginous component of the hip at this age, it is far superior to radiography. Graf23 was the first to quantify measurements to describe the anatomy of the newborn hip. The alpha angle represents the angle between the bony acetabular roof and the aspect of the ilium where it intersects the bony and cartilaginous components of the acetabulum. A normal alpha angle is greater than 50 degrees from birth to about 3 months of age, and greater than 60 degrees after 3 months of physiologic age. The beta angle represents the intersection between the line along the lateral margin of the cartilaginous acetabulum and a line intersecting the bony and cartilaginous aspects of the acetabulum. A normal angle measures less than 55 degrees. With progressive severity of dysplasia, the alpha angle will decrease and the beta angle will increase. The percent of head coverage on the coronal image is another commonly measured parameter, with the fraction of the head medial to the iliac line read as a percent. Less than 40% coverage is subnormal. Ultrasonographic assessment is technician dependent both for clarity of images and for ensurance that the correct planes are scanned. Recent recommendations suggest that ultrasound is a useful modality for stratification of hips as normal, immature, having mild dysplasia, or having severe dysplasia24 (Fig. 40-2).
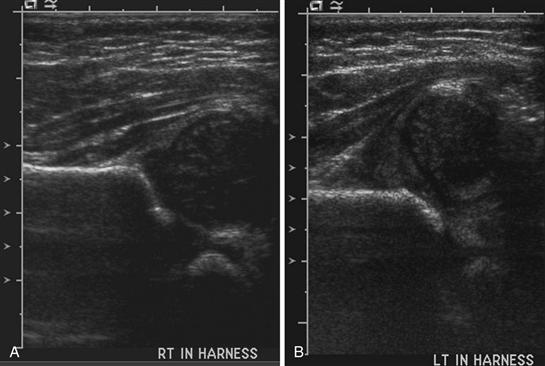
Figure 40-2 Ultrasound of both hips in a 7-week female. A, The right hip demonstrates a normal alpha angle and approximately 50% coverage of the femoral head. B, The left hip demonstrates a reduced alpha angle and a dislocated hip.
An alternative to the static ultrasound measurement of Graf is a dynamic ultrasound evaluation of the hip during performance of the Ortolani and Barlow tests with assessment of the extent of instability.25 Using this method, 4 to 6 mm of motion is believed to be normal in the first few days of life; however, guidelines for normal motion in older children have not been developed.25,26 Often, both static and dynamic methods are utilized. The general consensus in the literature is that ultrasound is a sensitive tool in assessment of the newborn hip.24,27-29 The resulting concern is the potential for treatment of newborns who do not require treatment.
A current issue that has not received much attention in the literature concerns the ultrasound appearance and clinical assessment of the premature infant. Much has been reported regarding the natural history of improvement in clinical stability and ultrasound improvement of the newborn over the initial weeks of life; however, the natural history has been less well documented. Simic and associates30 recently reported a study that attempted to investigate this issue. They studied 2045 newborns, 83% of whom were born prematurely at a mean gestational age of 34 weeks. They performed an ultrasound assessment and clinical evaluation of each hip and reported that 3.2% of all hips were unstable. They recommended early treatment of the unstable hip, even in the premature infant, by wide swaddling. No additional studies have explored the evaluation or treatment of premature infants.
Radiographs
Plain radiographs may demonstrate frank dislocation of the hips at any age, yet the largely cartilaginous nature of the hip before 6 months of age renders radiologic assessment generally inferior to ultrasound in this age group.24 Typical radiographic evaluation of dysplasia requires a well-centered and nonrotated film to identify the following parameters: (1) Hilgenreiner’s (horizontal) line between the triradiate cartilages bilaterally; (2) Perkin’s line, represented by a vertical line at the lateral extent of the acetabulum; (3) Shenton’s line along the inferior femoral neck and the inferior margin of the superior pubic ramus (Fig. 40-3) (Shenton’s line should be smooth and should not be broken by more than a millimeter); (4) the ossific nucleus of the femoral head, which, if present, should lie in the lower inner quadrant formed by the intersection of Hilgenreiner’s and Perkin’s lines; and (5) the acetabular teardrop, which is normally thinner centrally than proximally or distally. A V-shaped teardrop, which is wider proximally than distally, reflects abnormally deficient loading of the medial joint, which is a common component of the abnormal mechanics in a dysplastic hip.
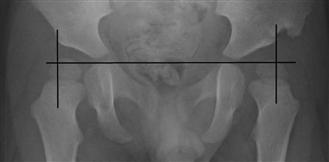
Figure 40-3 Radiographic demonstration of Hilgenreiner’s line (horizontal line) and Perkin’s line (vertical line). Note placement of the femoral heads in the lower inner quadrant, consistent with a reduced hip.
Certain standard radiographic measures are important in describing the immature and mature hip. The acetabular index (AI) as a measure of the obliquity of the bony acetabular subchondral bone is useful to quantify the extent of dysplasia in the immature hip. The AI is the angle between Hilgenreiner’s line, which is the horizontal line formed by connecting the triradiate cartilage, and a tangent to the acetabular articular surface (Fig. 40-4). The magnitude varies with age, with normal being less than 30 degrees in the newborn, less than 25 degrees by 1 year of age, and less than 20 degrees by 2 years of age.1,17 The Tonnis angle, which is the analogue of the acetabular index in the skeletally mature hip, is the angle between the horizontal line formed by connecting the centers of both femoral heads and a tangent to the acetabular sourcil; a normal value is less than 15 degrees.22,31 The lateral center edge angle of Wiberg is the angle between a vertical line from the center of the femoral head and a line from the center of the femoral head to the lateral edge of the acetabulum. A normal lateral center edge angle is greater than 20 degrees if the patient is younger than 13 years of age and is greater than 25 degrees in older patients.1 The acetabular teardrop should be assessed and if widened is suggestive of abnormal loading of the acetabulum, as would occur in a subluxated or dislocated hip.
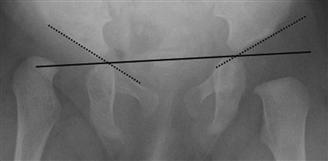
Figure 40-4 Radiographic demonstration of the acetabular index of both hips.
Arthrography
Arthrography employs contrast to outline the cartilaginous surfaces of the femoral head and acetabulum and to outline the labrum and the capsule. Radiopaque dye introduced percutaneously or during open surgery is usual, although air or carbon dioxide (CO2) has been used in the past. The risks of gas embolism make the use of air or CO2 relatively contraindicated. Arthrography is most commonly used intraoperatively for assessment of the quality of closed reduction. The so-called rose thorn sign represents the free border of the labrum and is a normal finding, if present.1 Another feature visualized on the arthrogram is the depth of reduction. When the reduction is not sufficiently deep within the acetabulum, a medial dye pool will be seen. More than 6 mm of pooling10 (Fig. 40-5) is considered abnormal.
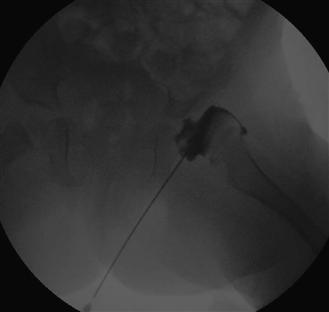
Figure 40-5 Arthrogram of a dislocated hip in a 17-month-old female. Note the increased medial dye pool, suggesting that the femoral head is not seated fully within the acetabulum.
Current recommendations for screening have been reported by the American Academy of Pediatrics.33 The Academy has suggested, on the basis of available evidence, that each newborn should receive a physical examination of the hips performed by the pediatrician, and the child should be referred for orthopedic evaluation if any abnormality is detected. The Academy has recommended against routine screening with ultrasound. An ultrasound evaluation was recommended in the setting of a female infant with a history of breech positioning, and such an evaluation was determined to be optional in the setting of a female infant with a positive family history of DDH or a male baby with a history of breech presentation. In Germany, Austria, and Israel, every baby is screened routinely at 6 to 8 weeks of age with an ultrasound of the hips; this universal screening has reduced dramatically the incidence of later-presenting dislocations and the incidence of surgery in DDH, and it has been shown to be very cost-effective in those countries. Such universal infant hip screening by ultrasound has not been recommended in the general population in Canada and the United States.24,34,35 Recently the benefits of any type of screening program for infant DDH have been questioned. Mahan and associates35A performed a decision analysis using the best evidence available and determined that the present universal physical examination screening with selective use of ultrasound screening was the optimal approach to minimizing the risk of development of hip osteoarthritis.
Screening studies have reported a prevalence of 7.7% with universal screening protocols, compared with 2.1% with only a clinical screening program.36,37 The recommendation in the literature is that universal screening does not impart additional benefit over selective screening because the prevalence of delayed acetabular dysplasia following selective screening was not found to be significantly greater than that following universal screening.24,38,39
Treatment
Stable Hip with Ultrasound Evidence of Dysplasia
Management of the hip that is clinically stable (Ortolani and Barlow negative) but has ultrasound evidence of dysplasia, in particular a borderline alpha angle of 50 to 60 degrees, has not been well described in the literature. Spontaneous improvement from deficient acetabular coverage diagnosed by ultrasound in the newborn period has been reported1,19,40; however, this has not translated into uniform recommendations regarding the time by which treatment should be instituted in the setting of a clinically stable hip with an abnormal ultrasound evaluation. Variation in recommendations regarding management of this clinical subgroup has been noted. Some clinicians institute treatment solely on the basis of the clinical evaluation without consideration of the ultrasound appearance; others advocate treatment, regardless of clinical stability, if the alpha angle is less than 50 degrees in the baby younger than 3 months old, and less than 60 degrees1 in the child older than 3 months. Another option that has been suggested is to base treatment on the combination of clinical stability and the ultrasound appearance at 6 weeks of age, with treatment consisting of a Pavlik harness if any abnormality is observed at the time of this assessment.
Bialik and colleagues40 studied the issue of overtreatment of initially abnormal hips in the newborn time period. Their study evaluated 8638 newborn hips by ultrasound soon after birth. Their protocol consisted of repeat clinical examination and ultrasound of those newborns with a stable hip at birth to 6 weeks of age. If the hips were unstable at birth, then the newborns were reassessed clinically and by ultrasound at 2 weeks of age. In either situation, a Pavlik harness was used for treatment if any abnormality was noted on assessment at the follow-up visit. Investigators reported that only 0.6% of hips studied required treatment. They did not encounter any complications as a result of delayed treatment using their protocol. This protocol has not been studied further in the literature.
Questions persist regarding patients with a clinically stable hip and an abnormal ultrasound. In particular, no definite recommendations have been put forth regarding management of the infant younger than 3 months of age with a borderline abnormal alpha angle of between 50 and 60 degrees. Similarly, whether treatment with a Pavlik harness or observation alone is necessary for the hip with an alpha angle less than 50 degrees or less than 30% acetabular coverage despite being clinically stable remains undetermined. It has been suggested, however, that if the hip is severely or moderately dysplastic with an alpha angle less than 50 degrees or with less than 30% coverage, then the hip should be treated with a Pavlik harness of an abduction brace. Furthermore, if the hip remains dysplastic beyond 3 months of life, then treatment should be initiated.
Serial imaging evaluation is extremely important in the dysplastic hip. Worsening of any abnormality and failure to improve with time represent relative indications to intervene or to change tactics.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








